Findings of excess morbidity and mortality among persons with serious mental disorders have prompted growing concern among mental health advocacy and provider organizations, consumer groups, and policy makers about addressing the physical health care needs of this population. Recent reports by the National Council for Community Behavioral Healthcare (
1 ), the Bazelon Center (
2 ), the National Association of State Mental Health Program Directors (
3 ), and Mental Health America (
4 ) have called for public-sector mental health programs to develop and implement strategies for improving the physical health of the clients they serve.
As the largest group of public-sector mental health providers in the United States, community mental health centers (CMHCs) stand on the front lines of this public health crisis. Single-site studies of clients at these clinics have suggested that they face problems in quality of diabetes treatment and outcomes (
5,
6 ), primary medical care (
7 ), and cardiovascular risk management (
8 ). However, in part because the community mental health system is so decentralized, no national data are currently available regarding the capacity of these organizations to screen, refer, or treat patients with medical problems.
We sought to address this gap by conducting a survey of the nation's CMHCs to understand their general medical screening practices, provision of on-site general medical services, and relationships with local community medical providers. The results can help inform policy, practice, and advocacy efforts seeking to improve health care for persons with serious mental disorders.
Methods
This study was conducted as a partnership between academic researchers and the National Council for Community Behavioral Health Care, the oldest and largest trade association representing CMHCs. (Although the term CMHCs can refer to the narrower set of organizations originally constructed under the 1963 Community Mental Health Centers Act, this brief report uses the term to reflect the broader range of public-sector, community-based providers of mental health services).
The study team developed a survey covering the following domains: priority placed by leadership on improving general medical care for its clients; capacity for on-site screening, assessment, and management of common medical problems (hypertension, obesity, hypercholesterolemia, and diabetes); presence of formal relationships with local community medical providers for medical screening, assessment, or treatment; and specific barriers to obtaining general medical services for clients.
The initial questionnaire was pilot tested with four CMHCs randomly selected from the National Council's membership. Input was solicited about burden of completing the survey, wording of items, and appropriateness of content. Results from this pilot study were used to refine the survey before distribution to the full National Council membership. [A copy of this survey is available as an online supplement at ps.psychiatryonline.org.]
The final survey was distributed during 2007 via mail and e-mail to the National Council's membership. All full-service CMHCs were included in the sampling frame (N=602). Two follow-up e-mails and a follow-up phone call were used to recruit a total of 181 community mental health organizations; the overall response rate was 30%. To generalize survey responses to the universe of CMHCs, nonresponse weights were generated on the basis of agency characteristics available for all National Council members. The weights account for differences between responders and nonresponders based on presence of substance use services or child and adolescent services, number of full-time-equivalent employees, number of unduplicated clients, annual budget, and geographic region.
Descriptive statistics, bivariate tables, and logistic regression models were used to describe the correlates of availability of general medical treatment services. All analyses were conducted by using SAS version 9.1 and included the weights.
Results
Compared with CMHCs that did not respond to the survey, CMHCs that did respond were more likely to provide substance use services and to be Medicare providers. There were no significant differences between responders and nonresponders in the provision of child and family services, annual budget, number of full-time employees, number of clients, or geographic region. [An appendix with a table listing the characteristics of responders and nonresponders is available as an online supplement at ps.psychiatryonline.org.]
In all, 169 (93%) CMHCs responding to the survey reported that improving their clients' general medical care was a medium priority (N=77, or 43%) or a high priority (N=93, or 51%) for their organization. Having an agreement with a community medical provider for addressing their clients' medical needs was reported by 75 (41%) respondents.
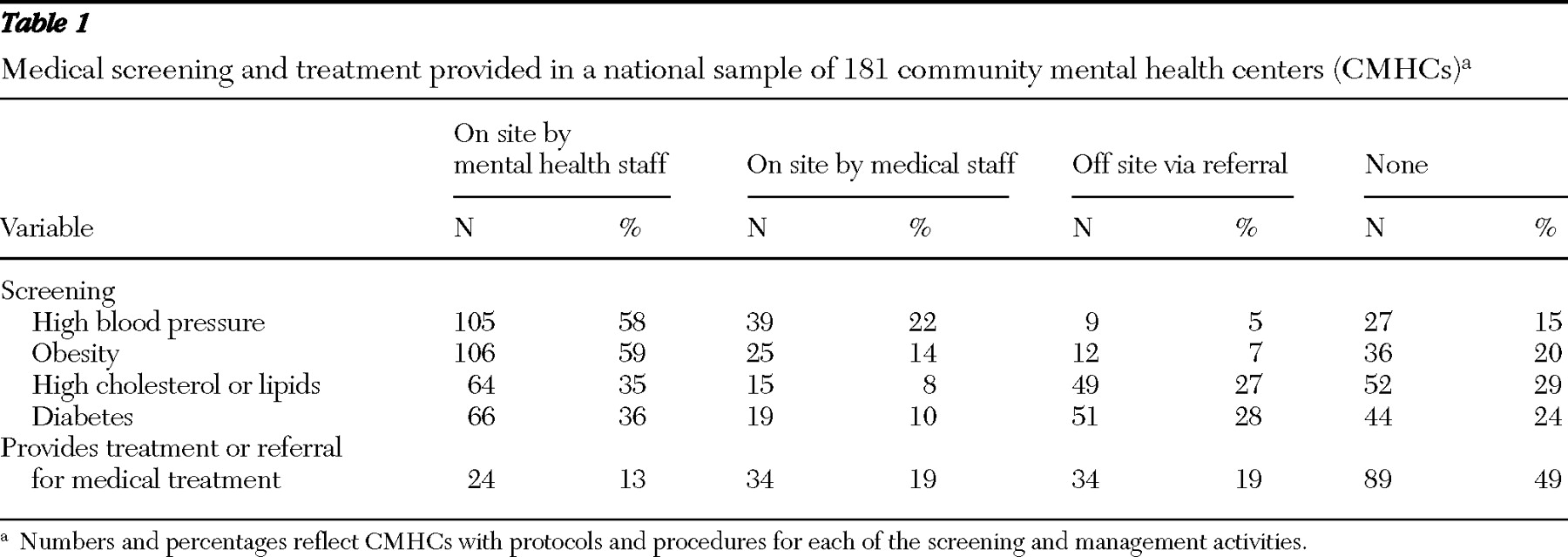
Most CMHCs reported routinely screening patients on site for hypertension (N=144, or 80%) and for obesity (N=131, or 72%) (
Table 1 ). A smaller percentage reported screening on site for dyslipidemia (N=79, or 44%) or diabetes (N=85, or 47%). Among sites with on-site screening capability, three-fourths to four-fifths reported that mental health staff rather than medical staff performed those screenings.
A smaller proportion of sites reported that they had clients screened off site for these problems, ranging from nine (5%) for blood pressure to 51 (28%) for diabetes. In all, 128 (71%) CMHCs reported a capacity to provide medical screening services either on site or off site.
In contrast, only 92 (51%) sites had the capacity to provide medical treatment for these problems, with 34 (19%) providing treatment on site via medical staff and 24 (13%) providing care on site via mental health staff (including psychiatrists). An additional 34 (19%) sites reported addressing these problems via off-site medical referrals (
Table 1 ).
Respondents reported a variety of barriers to providing medical management for their clients. The most common barriers were problems in reimbursement (N=130, or 72%), workforce limitations (N=124, or 69%), space and physical plant constraints (for example, lack of available space or equipment) (N=110, or 61%), and lack of options for referrals to community medical providers (N=101, or 56%). [An appendix with a table presenting data on barriers to the provision of general health services is available as an online supplement at ps.psychiatryonline.org.]
The only structural variable that was significantly correlated with capacity to provide medical care for CMHC clients in either bivariate or multivariate models was whether the site delivered substance use services. (Full results are available from the first author on request.) Of the 105 sites providing substance use services, 47 (45%) had the capacity to provide general medical services, whereas of the 76 sites not providing substance use services, 45 sites (59%) had such capacity. In multivariate models adjusting for all other available structural characteristics, sites providing substance use services were .39 times as likely to report capacity to provide their clients with medical care as sites not providing substance use services ( χ 2 =3.9, df=1, p=.04).
Discussion
Although a majority of CMHCs reported that improving their clients' medical care was a priority, they reported varying degrees of success in their capacity to provide assessment and screening for medical problems. CMHCs reported relatively high rates of procedures and protocols for screening, but they reported lower capacity to actually address their clients' medical problems, either on site or via referrals.
More than half of CMHC leaders reported that improving the general medical services received by their clients is a high priority, and more than 90% described this as either a high or medium priority for their organizations. This rate is surprisingly high, given the fact that these organizations have not historically considered their clients' medical problems as being within their purview (
9 ). A recent convergence of events, including findings about adverse metabolic side effects of second-generation antipsychotic medications (
10 ), the widespread adoption of the recovery paradigm and its emphasis on wellness (
11 ), and recent reports from key advocacy and provider groups (
1,
2,
3,
4 ), may be contributing to the high priority placed by CMHCs on improving their clients' medical care.
CMHCs are, to varying degrees, beginning to adopt routine screening for common cardiovascular and metabolic problems among their clients. The great majority of CMHCs reported having the capacity to perform routine blood pressure and obesity screenings on site, and most reported having the capacity to screen clients for all of the key metabolic parameters, either on site or via referral.
However, as with the case of screening for common mental disorders in primary care (
12 ), screening for medical disorders in public mental health settings will be of limited value unless there is a mechanism in place for follow-up and treatment. Only half of the sites that had screening programs in place for their patients had the capacity to provide medical care to clients who screened positive. Providers and managers may face a clinical and medicolegal dilemma if they screen for metabolic problems but do not have the ability to provide follow-up care for patients with positive findings.
Approximately two-thirds of sites with capacity to provide medical care delivered that care on site, with the remaining one-third providing that care via referrals to community medical providers. Providing care on site versus referral to off-site medical care may involve tradeoffs between access to care, which is optimized through on-site provision of services, and depth of expertise, which may be optimized through referrals to full-service medical facilities (
13 ).
The most common type of barrier to improving medical care identified by CMHC leaders was financial. Examples of these problems include difficulties in billing under Medicaid for medical services by mental health agencies, prohibition in some states of billing Medicaid for mental health and primary care services on the same day, and difficulties in finding community providers who are willing to provide care for uninsured patients (
13 ). One potentially promising strategy for overcoming some of the regulatory and reimbursement barriers is for a CMHC to partner with a community medical provider organization, which can provide services on site but bill and document under the umbrella of the medical organization (
1 ). However, the optimal strategy for arranging and paying for medical services will vary on the basis of the local environment, including an organization's size, insurance case mix, and local financing and scope-of-practice regulations.
Two closely related problems ranked second and third in provision of medical services for CMHC clients—workforce limitations and physical facility constraints. It is notable that among sites that had the capacity to provide medical treatment, mental health staff were commonly responsible for providing those services to clients. Most staff in CMHCs do not have general medical backgrounds (
14 ), and even staff with some medical training (for example, psychiatrists and psychiatric nurses) are often not comfortable screening for or managing common medical problems. Thus it is unclear what the implications are for quality of care at sites where mental health staff are the primary providers delivering general medical care. Lack of office space, examination rooms, and adequate equipment are likely to further limit the ability of these staff members to provide adequate on-site care or to perform laboratory screening tests. Addressing these issues is likely to require medical education to train existing staff; allocation of adequate space and equipment for providing medical resources; and where possible, hiring new staff, such as medical case managers with training and a job description that specifically focuses on coordination of delivery of medical services.
The other most commonly cited problem was lack of options for referrals to medical services in the community. Even sites providing some on-site medical services require the ability to refer patients with more complex medical problems to community medical providers for ongoing care. Improving linkages between community-based behavioral health organizations and safety net medical providers is likely to be a key strategy in improving medical care for persons treated in CMHCs. As recommended in the recent National Association of State Mental Health Program Directors' report (
3 ) on morbidity and mortality, "Good public policy will work to sustain, support and require integration of services between the two 'safety net' systems of Community Health Centers and [mental health] providers with integration ranging from coordination of care to full integration of medical and behavioral service."
Several limitations should be considered in interpreting the study findings. Most important, despite a relatively intensive plan to encourage survey response, including following up with both e-mails and phone contacts, there was only a 30% response rate. This problem is mitigated by the fact that the responders were similar to the overall National Council membership and that all results were weighted to reflect the small differences that were identified. Nonetheless, because respondents may have been more oriented toward these medical issues than nonrespondents, the results may overestimate the medical capacity in CMHCs nationwide. Second, the results were reported only at the level of the CMHC rather than the individual client. "Potential" access to care, as measured in this study, is a necessary but insufficient criterion for "realized" access, or actual use of services by individual patients (
15 ). Thus the reported availability of medical services described in this study likely represents an upper bound on the medical services actually received by CMHC clients.
Conclusions
The study provides the first national data on the provision of medical services by CMHCs in the United States. Given the broad reach of these agencies, leaders of these organizations will play a critical role in addressing the medical needs of persons with serious mental illness in the United States. However, they cannot accomplish this goal alone. Programs to address these needs will not be sustainable unless they can be reimbursed under Medicaid and state grants for the uninsured. Even sites that provide on-site medical services will continue to require partnerships with community medical providers. Such efforts will also require the active participation of consumers, who are the ultimate reason that the programs must succeed.
Acknowledgments and disclosures
This project was sponsored by grant K24-MH-075867 from the National Institute of Mental Health and by funding from Pfizer, Inc.
Dr. Marcus has received grants from Ortho-McNeil-Janssen Pharmaceuticals and has been a consultant to Eli Lilly and Company, Bristol-Myers Squibb, AstraZeneca, and Pfizer. Ms. Mauer is a paid consultant to the National Council for Community Behavioral Healthcare. The other authors report no competing interests.