Use of seclusion and restraint has long been a controversial issue in managing the behavior of psychiatric inpatients (
1 ). Recently, a variety of factors have brought this topic into the forefront of mental health policy development, including the publication of a special section on use of these procedures in this journal (
2 ), increased efforts to monitor and restrict seclusion and restraint by regulatory and accrediting agencies (
3,
4,
5 ), a major funding initiative on the part of the Substance Abuse and Mental Health Services Administration to assist facilities in the reduction of seclusion and restraint (
6 ), and a call by the National Association of State Mental Health Program Directors to eliminate the use of seclusion and restraint altogether (
7 ).
The literature in this area focuses on such topics as identification of patients most likely to be subjected to seclusion and restraint (
8 ), variations in rates of use across treatment settings (
9 ), and changes in rates brought about by therapeutic interventions, staff training programs, or institutional policy changes (
10,
11 ). Although a variety of methodological and statistical strategies have been employed in order to shed light on these issues, a common data reduction method has been to aggregate data over time, individuals, or treatment units. For instance, Jonikas and colleagues (
12 ) examined the impact of a program designed to decrease use of seclusion and restraint by comparing changes in the rates of seclusion and restraint on three psychiatric units at a university hospital. Rates were calculated from aggregated data and then plotted over time. Examination of these data revealed decreases in seclusion and restraint rates contiguous with introduction of the intervention program.
In another study that illustrates commonly encountered data aggregation techniques, Way and Banks (
13 ) examined data for patients hospitalized at 23 New York State psychiatric facilities. They compared the demographic and diagnostic characteristics of 657 patients who had been secluded or restrained with those of 22,929 patients who had not been secluded or restrained by aggregating each group's seclusion and restraint use over a four-week period. This procedure revealed that the group that had been restrained was more likely to be younger, female, and involuntarily hospitalized.
Although such studies have provided useful information regarding a variety of issues pertinent to this topic, data reduction strategies that aggregate or average data across individuals, time, or treatment units may obscure possible individual differences in the frequency or patterning of seclusion and restraint. Such information may be of value to clinicians and administrators who seek to determine whether definable subgroups of patients respond differentially to treatment interventions or to those who seek to examine whether discrete trajectories of seclusion and restraint use exist that would be helpful in predicting long-term seclusion and restraint utilization.
In this regard, several recently employed statistical methods have been useful in the identification of groups, or classes, of individuals with relatively homogeneous behavioral trajectories (
14 ). Many of these have been described under the general rubric of growth mixture modeling; latent class analysis (LCA) is such a procedure (
15 ). When applied to data sets consisting of events or behaviors recorded over time in a sample of participants, LCA is capable of detecting the presence of groups ("latent classes") of individuals with relatively homogeneous trajectories. Importantly, this method is a multivariate classification procedure that can define groups on the basis of the patterning of seclusion and restraint data over an entire hospital course, in contrast to univariate methods that have relied on single aggregations of seclusion and restraint data over varying, arbitrarily selected time frames (
13 ).
Thus the study presented here represents an effort to examine trajectories of seclusion and restraint use among 622 psychiatric inpatients over a two-year period in order to determine whether discrete classes of trajectories exist and to examine demographic and clinical characteristics that may differentiate these trajectories.
Methods
Participants
Data were derived from a review of medical records from patients admitted to a Midwestern state-funded psychiatric hospital in the United States composed of minimum-security buildings (84 beds), intermediate-security buildings (175 beds), and maximum-security buildings (201 beds). The project was approved by the institutional review board of the University of Missouri Health Sciences Center and given exempt status; consent was not required, as the study relied on archival data. All patients admitted during a five-year period (September 2001 to September 2006) and having a stay of at least 60 days were included. A total of 622 patients met these criteria. The sample was composed of 80% of all patients admitted to the facility during this time frame.
Data collection
Institutional databases yielded information regarding patient age, gender, ethnicity, admission diagnoses, admission status, and frequency of seclusion and restraint episodes over the course of the hospital stay (
Table 1 ). A patient and staff injury database was also accessed in order to determine the frequency with which patients were named as perpetrators in incident reports involving injuries to self or others. Likewise, a hospital abuse and neglect database was accessed in order to determine the frequency with which patients in the sample were victims of substantiated physical abuse. Seclusion and restraint episodes were recorded as bimonthly counts over the first two years after the initial date of admission.
Statistical analyses
An LCA was conducted to determine whether there were distinct groups of patients with regard to their trajectory of seclusion and restraint episodes over time; LCA parses individuals into groups on the basis of their similarity across a set of indicator variables (
15 ). In this case, the indicator variables were bimonthly counts of seclusion and restraint episodes over the course of the first two years after admission. All patients had at least one data point (60 days), and approximately half had the full two years of data available. Missing data were due to either shorter stays or to patients who had been recently admitted and were still in the hospital at the time data were collected. LCA can derive a model based on all available information, including complete and incomplete cases, so all patients were included in the analysis (
15 ).
LCAs were run using Mplus software (
15 ). The LCAs specified a Poisson distribution for the indicator variables, as they are count variables that are not normally distributed. Several indices of model fit were used to determine the appropriateness of a latent class model, as well as the number of classes to retain.
Results
The first step of the analysis determined the number of classes needed to characterize the data set. This was done by testing LCA solutions with different numbers of classes and by comparing model fit indices. The Akaike information criterion (AIC) and the Bayesian information criterion (BIC) are relative indicators of model fit, with lower values indicating better fit of the model to the data. The AIC and BIC values decreased across solutions containing two, three, and four classes, suggesting that a greater number of classes fit the data better. However, decreases in AIC and BIC were much larger going from two to three classes than going from three to four classes. According to the Vuong-Lo-Mendell-Rubin test, three classes were a significantly better fit to the data than two classes (p<.001), but four classes did not improve model fit significantly beyond that of the three classes (p>.05). Therefore, the three-class solution was retained.
Next, the distinctiveness of the three classes was examined. Entropy is a coefficient ranging from 0 to 1, with higher values indicating clearer delineation of classes and values of .80 or greater considered desirable. The entropy of the three-class model was .93, indicating that the classes were very well defined. Additionally, the average probabilities of correct latent class assignment revealed that each case was typically assigned a very high probability of belonging to a certain latent class (greater than .95), with very low probabilities of assignment to the other latent classes (less than .05). This speaks to the very high degree of separation among the three classes identified.
Figure 1 displays a graph of the three classes (trajectories) identified. A majority of patients (N=443, or 71%) fell within a low-trajectory class that showed a near-zero rate of episodes of seclusion and restraint throughout the study period. This class demonstrated an overall rate of 2.55 episodes of seclusion or restraint per 1,000 patient-care days. A second trajectory class of patients (N=138, or 22%) fell into a group that showed a moderate initial rate of seclusion or restraint episodes (about four in the first two months), quickly falling to a low rate (with an overall rate of 30.29 seclusion or restraint episodes per 1,000 patient-care days). Finally, 41 patients (7%) fit in a trajectory class characterized by a high initial rate of seclusion or restraint (about 12 in the first two months), followed by a relatively steady decline. This class had an overall rate of 149.84 episodes of seclusion or restraint per 1,000 patient-care days.
To further confirm the reliability of the three-class solution, a split-half cross-validation procedure was employed. If an LCA model derived from just half the data is then imposed on the second half of the data and fits both halves about equally well, then the LCA solution can be deemed robust and reliable.
The sample was randomly split in half, and the same LCA procedure used across the full sample was applied to just the first half of the sample (N=311). Again, a three-class solution was the best fit to the data in this half of the sample. Similar to the solution found based on the entire sample, 71% of the patients (N=221) were in a low-trajectory class, 22% (N=68) were in a medium-trajectory class, and 7% (N=22) were in a high-trajectory class. The AIC of this model was 3,073.5, and the BIC was 3,148.3.
The solution derived from the LCA procedure conducted on the first half of the sample was then applied to the second half of the sample. In the second half of the sample (N=311), 72% of patients (N=224) were assigned to the low-trajectory class, 21% (N=68) were assigned to the medium-trajectory class, and 6% (N=19) were assigned to the high-trajectory class. Across both split halves, there was comparably strong separation of the latent classes and a high degree of similarity in the proportion of patients assigned to each of the classes. Further, the AIC of this second model was 3,079.1, and the BIC was 3,086.6. The AIC increased only slightly across the split halves, while the BIC actually decreased, indicating that the model specified fit both halves to a similar degree. Therefore, the three-class solution identified from the full sample is robust.
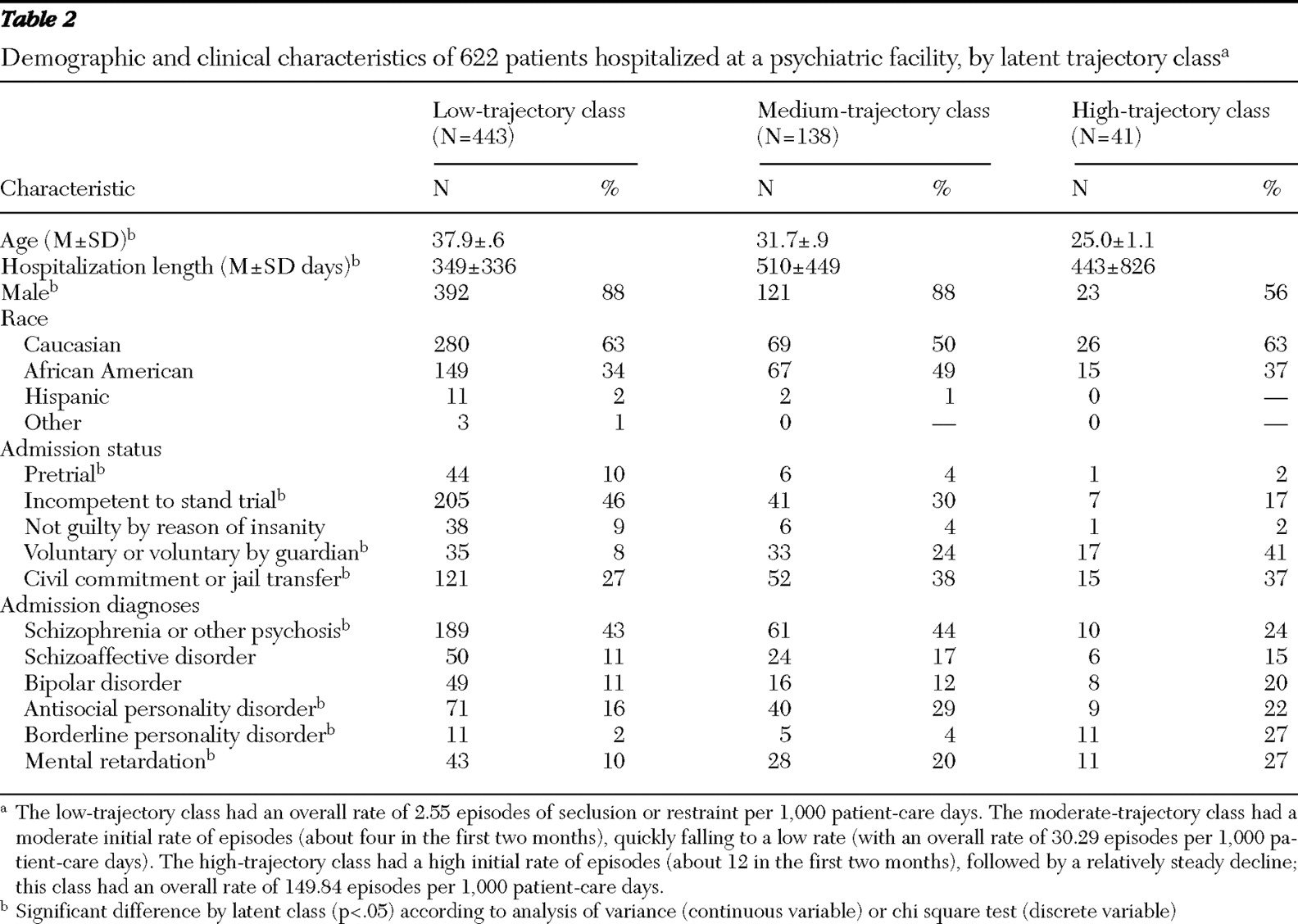
Having identified highly discrete trajectories of seclusion and restraint in the two years after the initial admission, we next examined a series of demographic and clinical variables to further characterize patients falling into each of the three latent classes. These findings are displayed in
Table 2 . Overall, patients falling into the medium and high trajectories tended to be younger, and women were overrepresented in the high-trajectory class. Patients admitted who were found to be incompetent to stand trial were significantly more likely to fit in a lower class, whereas patients who were voluntarily admitted or voluntarily admitted by their guardian were significantly more likely to fit in a higher class. Having an admission diagnosis of schizophrenia was more common among members of the low-trajectory class, whereas a diagnosis of borderline personality disorder was associated with members of the high-trajectory class and mental retardation was associated with members of the medium- and high-trajectory classes. Overall, it appears that certain demographic variables were consistently and significantly related to class membership.
The hospitalwide patient and staff injury database was then accessed and cross-referenced against trajectory class membership data. Comparisons between and among classes revealed that during the course of their hospitalizations, patients in the high-trajectory class were named as a perpetrator in incident reports at an overall rate of 183.44 times per 1,000 patient-care days. By contrast, patients in the medium-trajectory class were named at a rate of 50.26 times per 1,000 patient-care days and patients in the low-trajectory class were named at a rate of 6.81 times per 1,000 patient-care days.
Comparisons between trajectory classes with regard to the incidence of substantiated physical abuse revealed that 18 of the 622 patients (3%) had been physically abused during their hospital stays. Only one of these patients was a member of the low-trajectory class (one of 433 patients, or .2%). Eleven patients in the medium-trajectory class had been abused (11 of 138 patients, or 8%), compared with six patients in the high-trajectory class (six of 41 patients, or 15%). Thus patients in the high-trajectory class were 75 times more likely than members of the low-trajectory class to have been physically abused during their stay (.2% versus 15%).
An analysis of variance (ANOVA) conducted on length-of-stay data yielded a significant F test for the effect of trajectory class; follow-up multiple mean comparisons (Tukey HSD tests) revealed that the low-trajectory class had a significantly shorter average length of stay than the medium-trajectory class (11.2 months versus 15.0 months). However, a comparison between the lowest and the highest-trajectory classes failed to achieve significance, although the trend was for patients in the high-trajectory class to stay in the hospital longer (11.2 months versus 14.2 months). Thus there was a trend for patients with greater frequencies of seclusion and restraint utilization to stay in the hospital longer. However, these findings need to be tempered by the fact that all data on length of stay were collected over a two-year time frame following admission and a substantial number of patients continued to be hospitalized beyond this two-year time frame.
A second ANOVA was performed on length of stay to assess the effect of admission status (voluntary, court ordered, pretrial, incompetent to stand trial, or not guilty by reason of insanity). This ANOVA also generated a significant F test. Tukey HSD comparisons revealed that patients voluntarily admitted or admitted after being found not guilty by reason of insanity had significantly longer hospital stays than patients who were admitted through a court order, pretrial, or after they were found to be incompetent to stand trial (619 and 585 days versus 276, 299, and 383 days, respectively).
Discussion
Results of this study strongly support the contention that, at least in the context of the sample presented here, three relatively discrete groups of patients exist with respect to seclusion and restraint trajectory. The significance of trajectory class membership is underscored by findings that compared with patients in the lowest trajectory, patients in the high-trajectory class were almost 30 times more likely to be named as a perpetrator in an injury report and 75 times more likely to be subjected to physical abuse during their hospitalizations. In regard to this last point, it should be pointed out that the rates of physical abuse reported in this study were obtained from hospital abuse and neglect investigation records and relate to abuse that was perpetrated by staff on patients during the course of their hospitalizations, not rates of abuse gained from reviews of psychiatric histories or reports of childhood or adolescent experiences.
It needs to be acknowledged that there are substantive differences in opinion among mental health researchers, clinicians, and administrators regarding what needs to be put forth as the ultimate goal with respect to seclusion and restraint. Some have called for elimination of these procedures altogether (
7 ); others believe that reductions in frequency are a more reasonable and attainable goal (
16 ). From a clinical decision-making standpoint, early and accurate identification of a patient's trajectory class would serve either of these alternatives. For instance, this information could be used to proactively identify individuals at risk and to develop individualized person-centered interventions for them (that is, personal safety plans or trauma-informed treatment planning), as well as to provide specialized training to staff who work with these patients, so as to help staff implement effective behavioral procedures designed to forestall seclusion and restraint use or serve as alternatives to such practices (
17,
18 ). Conversely, individuals in the low-trajectory class could be fast-tracked to less restrictive treatment environments or at least to lower-security inpatient environments that afford more personal freedom and opportunities to engage in a wider range of therapeutic activities less encumbered by security restrictions.
Differences between trajectories with regard to a variety of demographic and diagnostic variables (
Table 2 ) may provide important clues as to factors that may eventually lead to early identification of which trajectory class patients might fall into. In this regard, it is worth noting the work of Krakowski and colleagues (
19 ) and that of Arango and colleagues (
20 ). Although both parties studied aggressive behavior over much more compressed time periods and in much more diagnostically restricted patient samples, both outlined a number of variables that differentiated violent patients from nonviolent patients. In the investigation by Krakowski and colleagues, which studied patients over a four-week time frame, a variety of factors distinguished patients who were operationally defined as being transiently violent, as opposed to being persistently violent, including positive symptoms and neurological impairment. (However, it should be noted that Krakowski and colleagues' methods were different from those of our study, as we used empirical, statistically generated criteria, rather than operational definitions.)
It goes without saying that future efforts to predict seclusion and restraint utilization will need to be carefully replicated and cross-validated in the context of prospective study designs (
21 ). For instance, cross-validations of the three-class trajectory structure to populations that contain significantly different distributions of patients with regard to security levels and admission status may find very different proportions of patients in the trajectory classes. Supporting this notion are F tests of length-of-stay data comparing patients grouped by admission status and chi square tests of admission status by trajectory class membership (
Table 2 ).
The investigation presented here has focused on a limited number of factors associated with trajectory class membership, namely patient demographic and diagnostic characteristics. Given the essentially interactive nature of the interpersonal process that culminates in the application of seclusion and restraint, it is reasonable to expect that studying staff attitudes and behaviors regarding these procedures (which certainly play a role in the decision to employ seclusion and restraint) will shed additional light on these issues. Conceptualization of seclusion and restraint as resulting from a series of patient-staff interactions leads to the conclusion that research focused on these interpersonal processes will facilitate efforts to understand and predict seclusion and restraint patterns more completely, as well as aid in efforts to reduce the practice. Results of the study presented here may aid efforts to identify patient-staff interactional patterns that lead to seclusion and restraint utilization, because our data have identified a subset of patients with an extraordinarily high frequency of seclusion and restraint implementation. A study of staff-patient interactions that are characteristic of these individuals (as contrasted with those who would fall into the low-trajectory class) might be a fruitful starting point in this endeavor.
Conclusions
It needs to be pointed out that over the past several decades, use of seclusion and restraint procedures has become largely restricted as a response to patient behaviors that are highly aggressive or potentially injurious or that seriously degrade the integrity of the treatment environment. Nevertheless, some studies have documented significant heterogeneity in the behaviors that are associated with the decision to employ seclusion and restraint (
22 ). In other settings, alternative methods are being employed to deal with patient aggression (
11 ). Such factors suggest that in the future, institutional databases need to be developed that consist of carefully defined and recorded instances of aggressive behavior, regardless of whether seclusion and restraint are employed.
Acknowledgments and disclosures
The authors thank Philip Stinger for his work with several institutional databases that were adapted for use on this project.
The authors report no competing interests.