Substance abuse is common among people with serious mental illness (
1 ), many of whom receive disability payments. People prone to addiction show higher use of drugs and alcohol when checks are received at the beginning of the month (
2,
3 ). Harmful consequences of drug use that also occur disproportionately when checks are received include discharge from residential substance abuse treatment (
4 ), emergency services visits (
5 ), and deaths related to drug and alcohol use (
6 ). Money itself can be a relapse trigger (
7 ), and benefit checks can facilitate the purchase of drugs and alcohol.
Based on the connection between substance use and mismanagement of personal funds, many treatment programs have instituted efforts to help psychiatric patients with co-occurring psychiatric and substance abuse problems to avoid diverting funds toward substance use (
8,
9 ). Money management services range from voluntary programs designed to provide information about budgeting (
10 ) to involuntary, mandated interventions, such as the assignment of a representative payee to receive and manage a patient's check. Assertive community treatment programs that treat patients with co-occurring substance use and psychiatric disorders often help with budgeting, storing funds, paying bills, and managing entitlements, but money management is only one of several interventions in assertive community treatment (
11,
12,
13 ), making it difficult to pinpoint the effects of money management among the other services.
In the sole randomized controlled trial involving involuntary money management, 184 veterans were randomly assigned to referral to a community-based payee program or to treatment as usual and followed for 12 months (
14 ). Compared with beneficiaries in the control group, beneficiaries in the payee assignment group used substances for fewer months and rated their money management as significantly better, but this pioneering trial's generalizability was limited by the fact that the active intervention was bundled with and included referral to extensive case management services in addition to the payee assignment. The benefits of payee assignment have been equivocal in other studies (
3,
15 ), although specialized payee services that are based at community mental health centers have shown promise (
16 ).
There have not been any controlled trials of an unbundled money management-based intervention. In this article we report on a 36-week single-blind, randomized controlled clinical trial designed to test the efficacy of a voluntary money management program, which we compared with a control condition, in fostering abstinence among veterans in treatment for mental illness, a substance use disorder, or co-occurring disorders. Secondary aims of the study were to determine to what extent participants engaged in money management—that is, attending sessions and allowing their funds to be managed—and how participants rated the experience.
Methods
Recruitment, enrollment, and randomization
Patients who were being treated for a psychiatric disorder, a substance use disorder, or co-occurring psychiatric and substance use disorders were recruited by advertisement and clinician referral at the main campuses of the Veterans Affairs (VA) Connecticut Healthcare System and the Northampton VA Medical Center Patients were enrolled who had spent at least $100 on cocaine, alcohol, cannabis, or a combination of these substances during the preceding 90 days and received at least $300 income per month. Patients were excluded if they already had a payee or other money manager or if they were physiologically dependent on opioids or alcohol. All study procedures were approved by the institutional review boards of the VA Connecticut Healthcare System and Yale University. All patients provided written informed consent, and enrollment was conducted from August 2000 until February 2004.
Patients were screened to determine eligibility, and eligible patients completed an extensive battery of assessments. Before we randomly assigned participants to an intervention condition, all patients were scheduled for an individual visit with the money manager to assess their finances and to explain the interventions in more detail. To avoid assigning patients who had no interest in money management to an intervention, random assignment occurred only for patients who came to the visit with funds to open a checking account or with their checkbook so that they could begin receiving advisor-teller money management (ATM), should they be assigned to that intervention. The substance for which each patient had spent the most in the previous 90 days was balanced between the ATM and control groups by urn randomization (
17 ).
Interventions
ATM. The ATM intervention is a therapy that uses voluntary money management to reduce substance use and incorporates elements of optimal payee practice (
18 ). Staff trained as money managers in this program performed three functions—serving as a teller to store patients' funds, training patients to manage their own funds, and linking spending to treatment goals. In the teller function, staff encouraged patients, but did not require them, to establish a checking account and to allow the money manager to store their checkbook, their automated bank card, or both. In the training function, patients and counselors planned a budget each month, and at the end of the month, they reviewed whether the budget had been followed.
To encourage treatment-linked spending, breath-analysis tests and on-site urine tests were conducted at weekly ATM counseling visits. Patients were encouraged not to spend money if the tests were positive. Patients were encouraged to identify additional activities compatible with abstinence (
19 ) and make contracts to reward themselves the next week with their own discretionary funds if the activities were successfully carried out or if they had been abstinent. Patients who requested funds that had not been budgeted were encouraged to fill out a written request and wait two working days to be certain that the unplanned expenditure was prudent. An updated manual describing ATM is available for download (
20 ).
Control. For the control condition, patients were given a workbook in which they were asked to construct a budget and track their expenses and income. Counseling sessions involved supporting patients' efforts to use the workbook. The same bachelor's-level staff who served as ATM managers also guided the control intervention.
Data collection and measurement
Participants were paid for each of the 19 assessments and could earn a total of $325 if they completed all of the study assessments. Assessments were conducted by bachelor's-level staff. Baseline assessments characterized patients on a broad array of measures. Interviews using the Structured Clinical Interview for DSM-IV (
21 ) were conducted, and the Addiction Severity Index (ASI) (
22 ) was administered.
Breath-analysis tests, urine toxicology tests, and substance abuse calendars, completed with the timeline follow-back method (
23 ), were collected every two weeks. On-site toxicology tests (Dade Behring, San Jose) were administered and processed for cocaine, opioids, and cannabis. The follow-up version of the ASI was administered every four weeks. Observer-rated psychosocial function was measured every four weeks with the Global Assessment of Functioning (GAF) (
24 ).
Domains of money management were assessed every four weeks by having patients rate their agreement with statements rated on a Likert scale anchored by 1, strongly disagree, and 4, strongly agree (items available on request). The domains assessed, drawn from prior research (
25 ), were budgeting, perceived benefit from the intervention, degree of misspending, satisfaction with the intervention, and coercion by the money manager.
Data analysis
Data analysis proceeded in several steps. First, baseline characteristics of participants assigned to ATM and those assigned to the control group were compared by t tests and chi square tests to evaluate the success of the randomization and to identify unequally distributed characteristics to use later as covariates when comparing outcomes between the groups. To assess differences in the completeness of outcome data collected in the ATM and control groups, we compared time to last data collection by proportional hazards regression.
The primary outcome measures were weeks of self-reported abstinence from both alcohol and cocaine and proportion of urine toxicology tests free of cocaine metabolite. Secondary outcome measures considered included weeks of self-reported abstinence from cocaine, self-reported abstinence from alcohol, composite follow-up scores on the ASI alcohol and drug subscales (
26 ), the amount of money spent on drugs and alcohol, and GAF scores.
Generalized estimation equations with SAS PROC GENMOD were used for the dichotomous variables representing self-reported abstinence and toxicology-verified abstinence. Hierarchical linear models using PROC MIXED were used to compare the effects of group assignment on continuous outcomes, such as the follow-up scores on the ASI composite indices.
Results
Participants and sampling
Altogether, 167 of the 391 individuals screened (43%) did not meet eligibility criteria. Fifty-nine percent (133 veterans) of the 224 eligible participants were not assigned to an intervention; 36% (81 veterans) refused to participate, and an additional 23% (52 veterans) were excluded for other reasons (for example, they did not keep appointments or moved out of the geographic area). Eighty-five patients were randomly assigned to an intervention (44 to ATM and 41 to the control condition) and completed at least one follow-up assessment.
Forty of the 85 patients who were followed completed week 36 assessments, 20 of whom were assigned to ATM and 20 to the control condition. There was no significant difference between groups in length of time in which data were collected, and there was no difference in the mean±SD percentage of scheduled monthly follow-up assessments completed (control, 65%±34%; ATM, 58%±33%). Three study participants died from medical illnesses, two in ATM and one assigned to the control group.
Participant characteristics
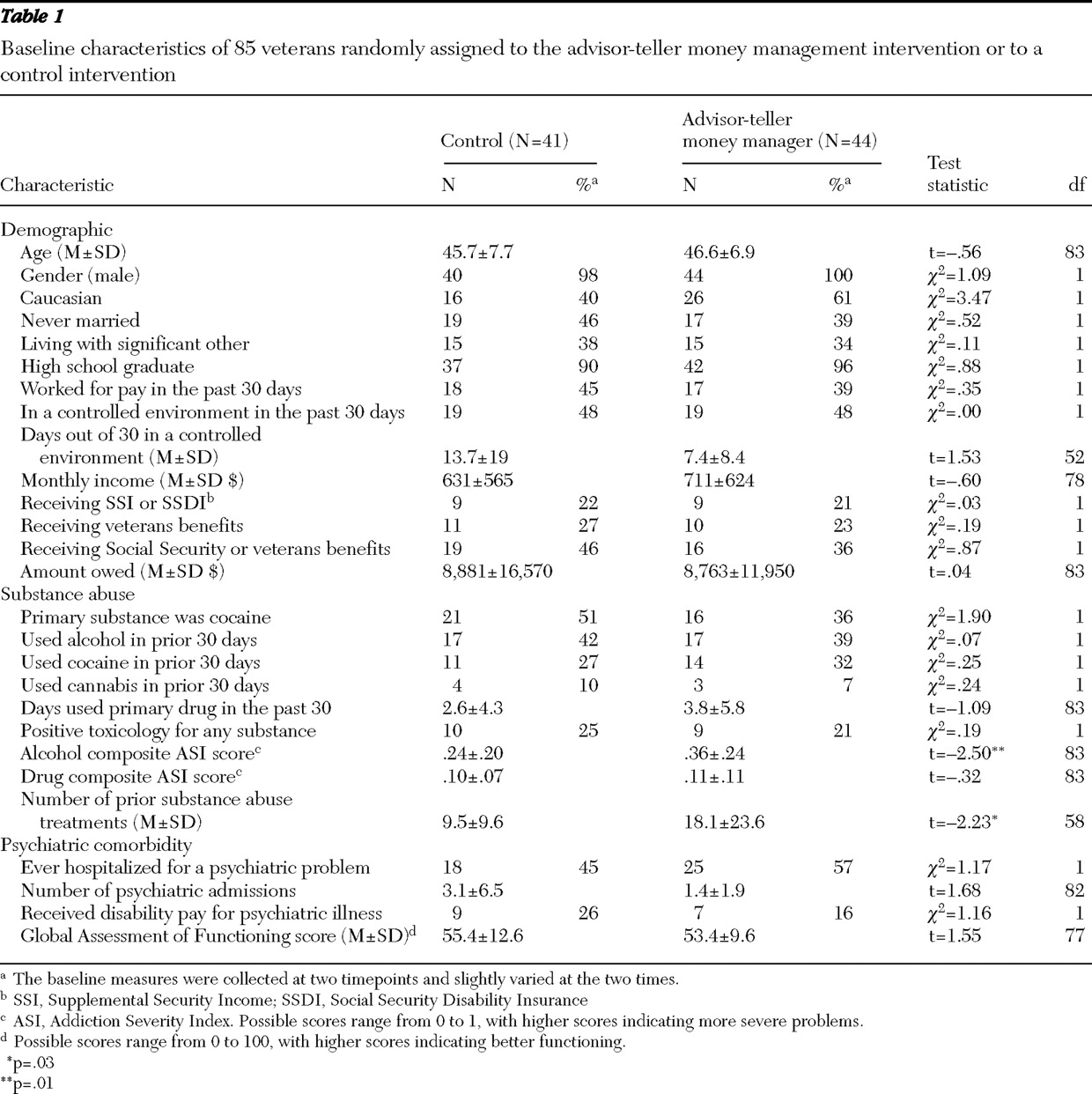
Participants were predominantly middle-aged, male veterans (
Table 1 ). Median monthly income was $655, and median indebtedness was remarkably high ($3,997). Seventy (82%) of the veterans owed more than $100.
A substantial proportion of the participants had concomitant psychiatric illnesses. Altogether, 28 (33%) met DSM-IV criteria for major depressive disorder, four (5%) for schizophrenia or an unspecified psychotic disorder, ten (12%) for bipolar disorder, and five (6%) for generalized anxiety disorder or dysthymic disorder. Altogether, 52 (61%) of the participants had one of these psychiatric disorders.
Two of 27 baseline measures suggested more severe substance use in the ATM group than in the control group. Participants assigned to ATM had significantly higher baseline ASI alcohol composite scores (p=.01) and had been hospitalized more times for substance abuse treatment (p=.03) than participants in the control group.
Extent of participation in ATM
As expected, compared with participants assigned to the control intervention, participants assigned to ATM attended many more money management sessions (20.6±14.9 versus 8.1±8.9 sessions; t=4.7, df=71, p<.001). Altogether, 22 of the 44 participants assigned to ATM attended more than 18 sessions. Twenty-seven (61%) of those assigned to ATM gave checkbooks to their money managers to hold, and an additional six (14%) gave the money manager a checkbook to hold but took it back later.
Weekly treatment contracting was encouraged but was not used extensively. Twenty of 44 participants (46%) assigned to ATM rewarded themselves with their own funds (via check or automated bank card) for completing activities they had contracted, but these participants reinforced themselves only an average of 2.6 times each. Reinforcing involved the veteran's writing a check to pay an expense or borrowing the stored bank card to make a withdrawal. The agreement to delay requests of unbudgeted funds to allow reconsideration of impulsive spending was rarely implemented; only five participants (11%) agreed to a delay of a day or longer before receiving requested funds.
Substance abuse outcomes
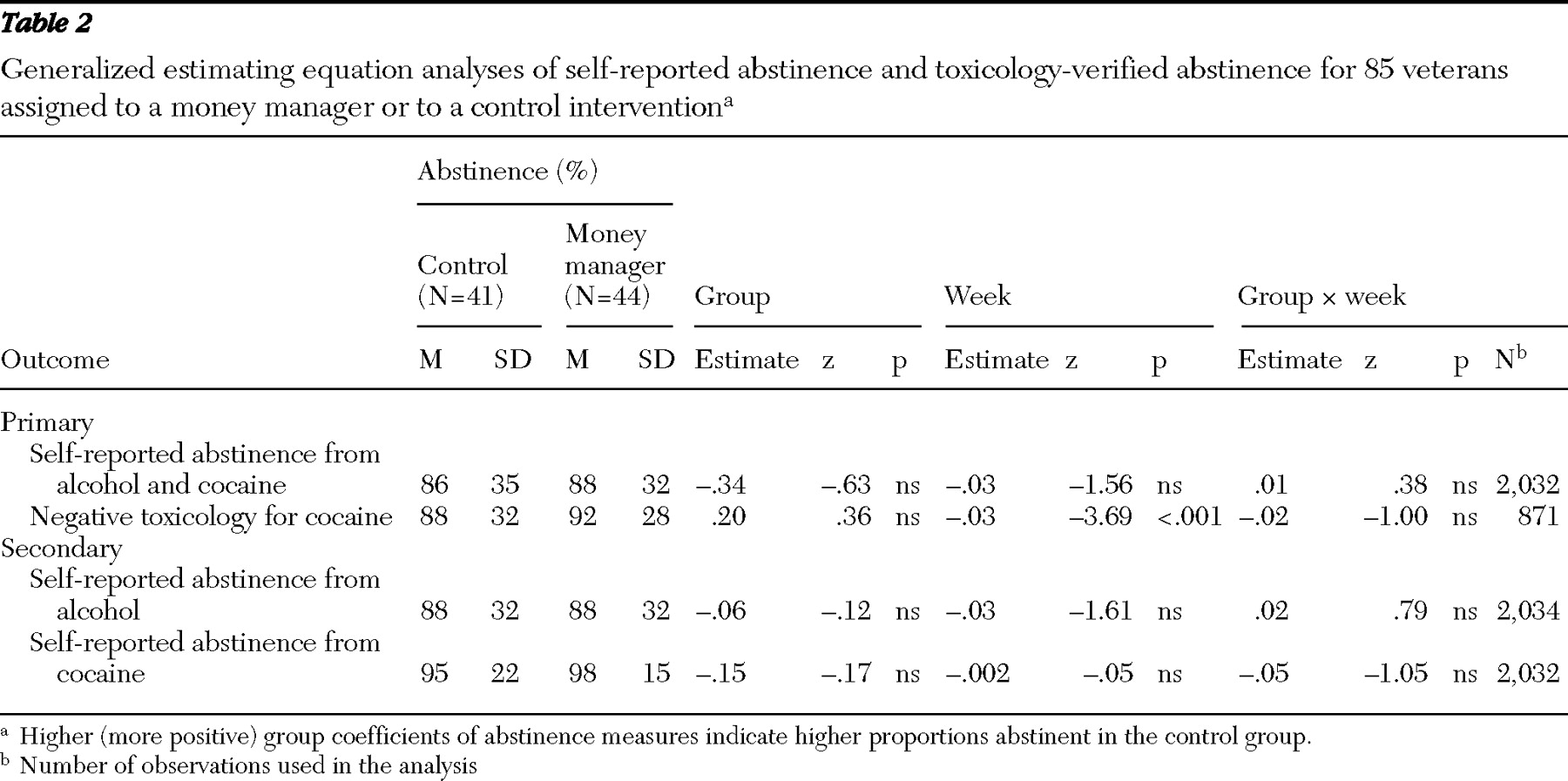
The proportion of outcome observations with self-reported abstinence from both cocaine and alcohol was 86% in the control group and 88% in the ATM group (
Table 2 ). Analysis yielded no significant differences associated with group assignment, time, or the group-by-time interaction (
Table 2 ). The other primary outcome, proportion of toxicology tests negative for cocaine, was high (control, 88%; ATM, 92%) and did not differ significantly between groups overall or over time. However, a post hoc analysis restricted to 37 patients who had primarily abused cocaine supported the efficacy of ATM; after covarying for baseline measurements, there were significantly more negative toxicology tests in the ATM group (p=.008). Results of analyses that separately considered self-reported abstinence from alcohol and abstinence from cocaine did not differ by group assignment (
Table 2 ).
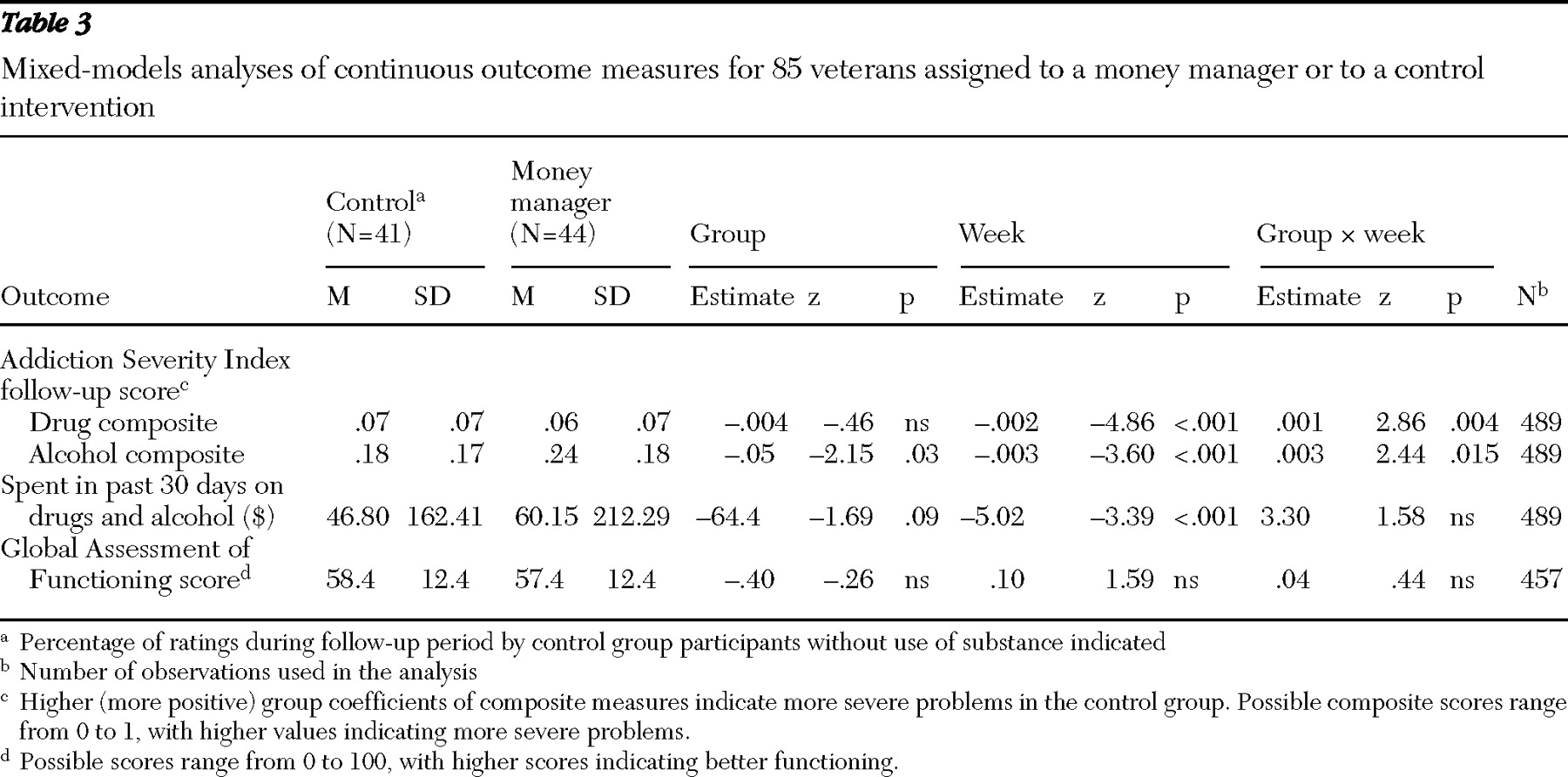
Table 3 shows the continuous outcome measures that were analyzed with mixed models. Study participants had less severe ASI drug composite scores over time, and this reduction in the drug composite scores was greater over time among ATM participants, as indicated by a significantly positive group-by-time effect. A similar pattern of results was apparent for the ASI alcohol composite scores. There was no difference between the groups by time in the amount of money spent on drugs and alcohol.
Money management processes
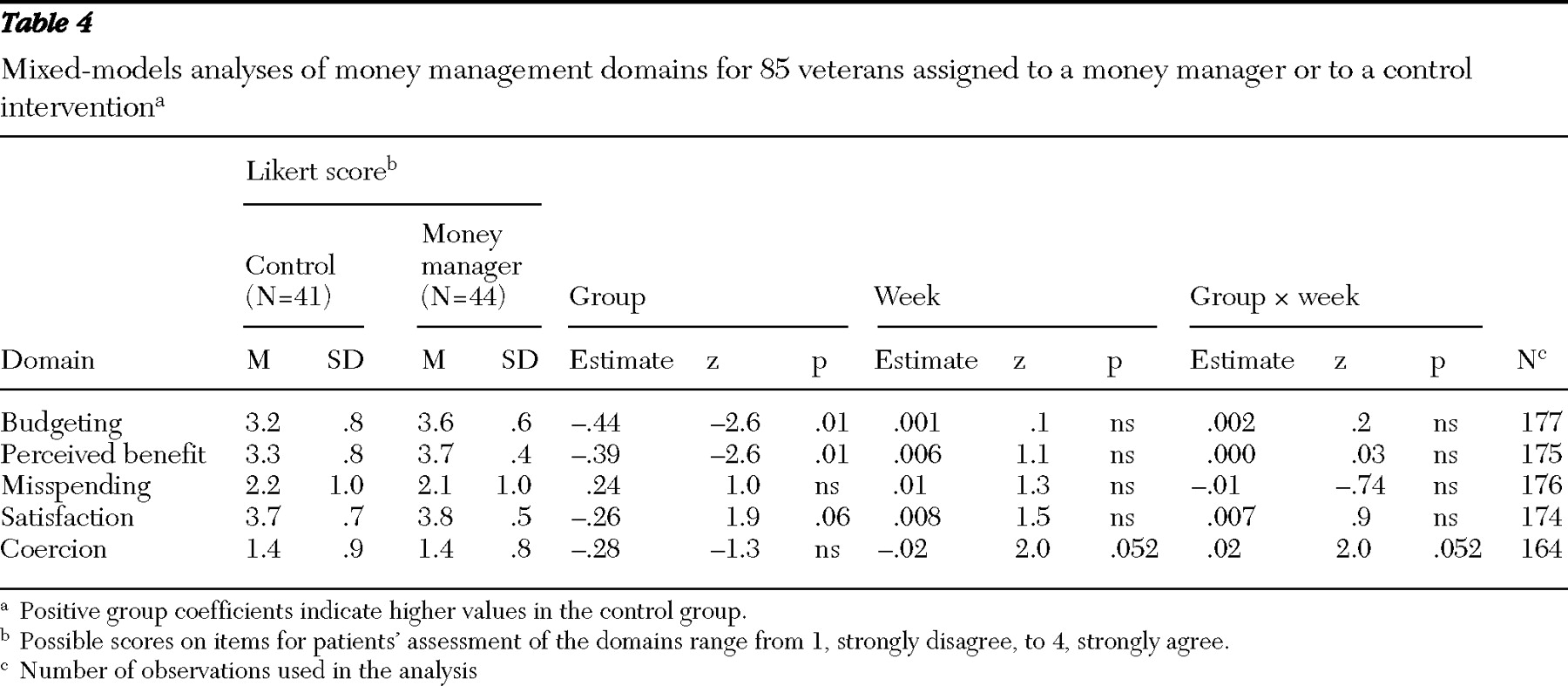
Compared with participants in the control group, participants in the ATM intervention rated higher agreement with statements about having benefited from treatment and agreed more with statements indicating that they planned and adhered to a budget (
Table 4 ). These rated advantages of ATM did not appear to be related to nonspecific appreciation of ATM because overall satisfaction ratings did not differ between the two groups. Ratings of coercion were low and did not differ between groups, and the trend toward a group-by-time effect on coercion was not in the direction of more coercion over time in the ATM group.
Adverse effects of ATM
One participant in the ATM intervention suspected that his money manager was responsible for his being billed by the VA for his appointments. A participant with schizophrenia temporarily believed that the VA had taken his money but changed his mind with treatment. Another participant with a history of irritability became upset during counseling and discontinued study participation. There were no other adverse events related to the money management intervention.
GAF
There were no significant changes in GAF scores over time and no significant differences between groups (
Table 3 ).
Discussion and conclusions
ATM was well received, in that a substantial proportion of people assigned to this voluntary intervention attended money management sessions, stored their checkbooks or bank cards with the money manager, and contracted to receive more of their funds when they achieved individually chosen goals. Despite a ceiling effect caused by the overall high levels of abstinence among veterans who were followed, ATM showed promise as a treatment.
ATM was not associated with significant benefit, as shown by a group-by-time interaction, on self-reported abstinence or on cocaine-negative urine toxicology tests, but the intervention was associated with significant reductions in the ASI alcohol and drug abuse composite scores. Unlike dichotomous measures of abstinence or use, ASI composite scores are continuous measures reflecting other factors, such as the extent of drug-related problems and how much treatment is needed. One possible explanation for the effect on the drug and alcohol use composite scores and lack of significant effects on self-report and toxicology is that ATM may mitigate the severity of substance-related problems without reducing the proportion of weeks of substance use. It is noteworthy that the patterns of group-by-time effects concerning cocaine use all were in the direction of efficacy of the ATM intervention. In addition to the significant effect on drug use composite scores among participants assigned to ATM, there were statistically nonsignificant trends toward less self-reported cocaine use, fewer positive urine toxicology tests, and less money spent on substances of abuse.
A money management intervention was unacceptable to many potential participants, as suggested by the fact that only 41% of eligible participants proceeded to the random assignment portion of the trial, but it was impressive that participation in ATM was extensive after randomization and that subjective ratings of ATM were quite favorable. These results are consistent with those of other studies in which participants in a community-based payee program indicated that although enrollment was involuntary, patients found money management helpful over time (
27 ). Participation in ATM also reflected the fact that the participants wanted help with their finances. The desire for help with finances was also reflected in the surprisingly high participation in a control condition that offered little counselor input beyond support for completing a budgeting workbook. People with little income and people who have serious mental illness indicate a desire for help with concrete financial concerns (
28 ), and the satisfaction of material needs typically takes precedence over other needs (
29 ).
The tested version of advisor-teller money management involved storing checkbooks and bank cards instead of a version of ATM more akin to representative payee practice, in which the money manager receives the patient's funds and stores them in an account that can be accessed only by the payee. Although most veterans assigned to ATM agreed to have their savings materials stored and to meet a money manager to budget, few participants (five out of 44 ATM participants) allowed the money manager to delay unplanned spending to reconsider the unplanned expenditure. It is possible that the intervention's effects would be greater if the budgeting and training components of ATM were used in conjunction with the restrictions on beneficiary access to funds implemented by assigned representative payees.
Limitations of this study include the restriction to veterans, almost all of whom were male, and high abstinence rates in both groups. Several factors mitigated against finding a robust effect of ATM in this population. The high rates of abstinence among study participants created a control group ceiling effect that was hard to improve on. This ceiling effect did not appear to be caused by selective dropout of participants with more severe baseline addiction, because post hoc analyses showed no association between baseline addiction severity measures and percentage of follow-up interviews that were completed. Further evidence that selective attrition did not account for the high abstinence rates comes from another study of patients with psychiatric disorders and concomitant substance abuse, conducted at the same sites and during the same period as our study, which also reported extremely high abstinence rates (
30 ). Our randomly assigned sample of 85 had sufficient power to detect an effect size of .4 with power of .8 and significance of .05, two-tailed (
31 ), but enrollment of people who used alcohol alone also may have diluted the study's power to detect an effect of ATM on cocaine use. Although the "check effect" of more substance use when checks are received at the beginning of the month has been demonstrated for both alcohol and other drug use (
6 ), approaches based on money management may be more effective for cocaine because cocaine binges are more expensive.
In summary, this study found that a money management-based treatment targeting cocaine and alcohol use is feasible, acceptable to participants, and potentially efficacious.
Acknowledgments and disclosures
This research was supported in part by VA Research Development; by grants R01-DA012952, K02-DA017277, and P50-DA09241 from the National Institute on Drug Abuse; and by Veterans Integrated Service Network 1 of the Mental Illness Research, Education and Clinical Care Center.
The authors report no competing interests.