Although researchers, policy makers, and clinicians recognize the high prevalence of mental disorders among incarcerated individuals, there has been little work to assess the burden of such conditions among persons placed on probation, the most common sentencing option used in the criminal justice system. To our knowledge only one study has provided estimates for the prevalence of mental disorders and the use of mental health services among probationers. Using data from the 1995 Survey of Adults on Probation, Ditton (
1 ) found that 16% of individuals on probation reported having a mental health condition, as measured by reporting that they had been informed by a health professional they had a mental disorder or by reporting that they had spent at least one night in an inpatient psychiatric setting. More than half (56%) of this group reported using some kind of mental health service in the community. These findings pose an interesting paradox if taken at face value. When these findings are compared with a Surgeon General report on the general population during the same period (
2 ), the rate of mental disorders is lower among persons on probation than in the general population (16% versus 21%), although the rate of mental health services use is more than twice as high (56% versus 23%).
In this study, we used a robust data set to examine among past-year probationers the prevalence of symptoms indicative of mental disorders, including an analysis of their type and the frequency of mental health services use. For the purposes of this study, we hypothesized that symptom prevalence, types of symptoms, and mental health service use would be the same or greater among probationers than among the general population.
Methods
We used data from the 2001 National Household Survey on Drug Abuse (NHSDA) (
3 ), a weighted, nationally representative annual survey of U.S. residents aged 12 years and older. The 2001 survey contains questions about symptoms of mental disorders, mental health service use, and criminal justice involvement. From this data set we identified adults between 18 and 64 years who reported past-year symptoms of panic, depression, phobia, general anxiety, posttraumatic stress disorder (PTSD), mania, and psychosis. For these categories, symptom severity was rated as none, mild, moderate, and high. Respondents also rated impairment of functioning (no difficulty, mild, moderate, and severe difficulty) for five domains: learning, activities of daily living, leaving the house, household responsibilities, and school and work performance. We established "caseness" (
4 ) for membership in the cohort on the basis of a minimum set of entry responses, including at least one symptom of mild severity with a mild impact on functioning.
Respondents reported involvement with probation, with and without arrest, during the past year. We excluded from the sample 295 individuals who reported mental disorder symptoms and arrest but no probation. Mental health service use was defined as at least one visit to a mental health center, private therapist, outpatient mental health service, or day treatment program. We rated mental health service use in a conservative fashion by excluding substance and general health services, categories well separated in the NHSDA interview. Data management and analyses were conducted with SAS, version 9.0. Probability comparisons for study groups regarding symptom prevalence and service use were analyzed with chi square tests.
Results
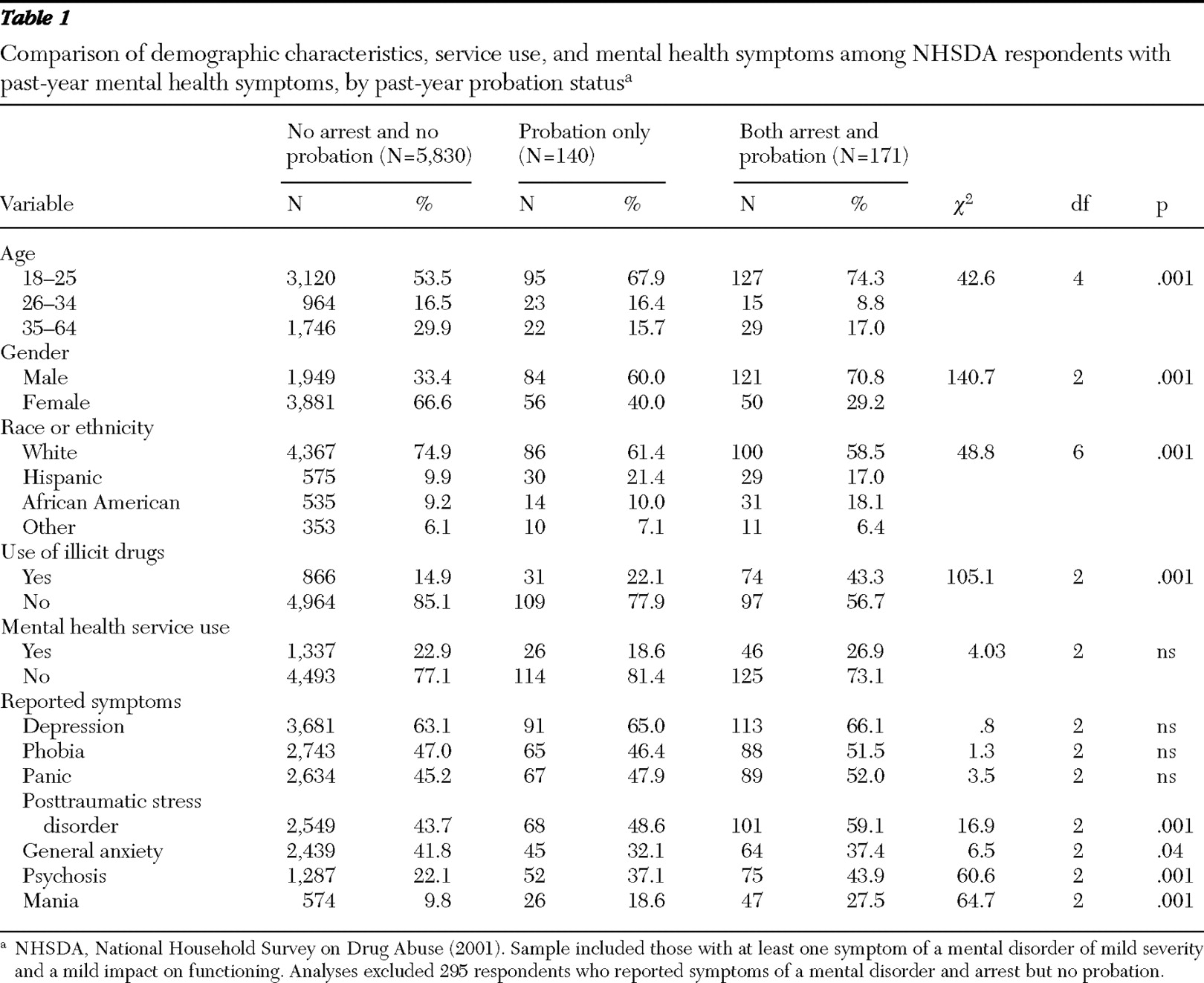
Results are reported in
Table 1 . Of the NHSDA adult population (N=35,693), 1,168 (3.3%) reported probation involvement during the past year. Of this group, 311 (26.6%) met our criteria for caseness (that is—had at least one symptom of mild severity with a mild impact on functioning). Within the general sample of the NHSDA not having any criminal justice involvement (N=34,230), 5,830 (17.0%) were classified as fulfilling our criteria. Compared with the group without past-year probation, the group with past-year probation was more likely to be younger, male, and nonwhite and to use drugs. Compared with the nonprobation group, the probation group also was significantly more likely to report symptoms of psychosis (p=.001), mania (p=.001), and PTSD (p=.001) but significantly less likely to report general anxiety (p=.04). There was no difference between the two groups in reports of symptoms of depression, panic, or phobia.
There was also no difference in mental health services use across groups. Among the 311 probationers, 26 of the 140 (18.6%) who had not been arrested in the past year and 46 of the 171 (26.9%) who had been arrested in the past year sought mental health care, compared with 1,337 (22.9%) of those without criminal justice involvement.
Discussion
Among all adults in the 2001 NHSDA, 18% (N=6,141) reported mental disorder symptoms and fulfilled our criteria for caseness. This rate is lower than the rate of diagnosable mental disorders reported by the Surgeon General (
2 ) (21%). Our study showed higher rates of mental disorder symptoms among those with past-year probation than Ditton's study of probationers (
1 ) (27% versus 16%); yet the probationers in our sample had service use levels far lower than Ditton's sample (23% versus 56%).
The broader scope of data available in the NHSDA allowed us to examine symptoms in greater detail, although the level of co-occurrence of symptoms noted in
Table 1 underscores a need for cautious interpretation. We found that the distribution of symptoms among probationers differed from the distribution among those without probation involvement, with probationers being more likely to report having psychosis, mania, and PTSD symptoms in the past year and less likely to report having general anxiety. Depression was the most commonly reported symptom and was roughly equal across groups. High rates of reported depression and mania in the group with past-year probation might suggest a greater prevalence of bipolar disorder, but this must be viewed in a tentative fashion, given the nature of the self-report data. The high rate of psychosis in the probation group may point to the presence of people with severe, persisting mental disorders, perhaps similar to other populations to which specialized intervention programs have been offered (
5,
6 ), although this cannot be confirmed from this data set. These findings also underscore the importance of continued development of specific practice guidelines for persons with past-year probation (
7 ).
Beyond the limitations noted above, this study has several important limitations. First, the nature of data collection did not allow examination of the temporal sequence of probation or arrest events and mental health service use. Second, we are acutely aware that symptom prevalence is not a proxy for diagnosis, despite our efforts to establish parameters for caseness. Third, as with the symptom reports, service use was self-reported, although the literature supports the reliability of such data for this population (
8 ). Fourth, although the overall sample was nationally representative, there was no readily available method to verify whether subgroup data were representative. (We chose this particular survey because its sampling methods were sufficiently rigorous to at least allow this possibility.) Fifth, the survey did not clearly delineate the source of referral for mental health services. It is possible that some originated from the court system; few, however, would have come from specialized mental health courts because these were new and uncommon in 2001 (
9 ), the year of the NHSDA data collection. Finally, differences in service use may be an artifact because we excluded substance use, medical, and all other treatments in this analysis, as well as persons arrested in the past year but not placed on probation.
Conclusions
On the basis of this sample, the prevalence of symptoms indicative of mental disorders was higher among probationers than in the general population. The type and distribution of reported symptoms were significantly different between those who had been on probation in the past year and those who had not. These are important considerations for probation departments when planning mental health service connections.
Acknowledgments and disclosures
The writing of this brief report was supported in part by grant P20-MH071897 (principal investigator, Dr. Caine) from the National Institute of Mental Health. This brief report draws on a portion of Dr. Crilly's dissertation, completed under the supervision of Dr. Friedman and coauthors.
The authors report no competing interests.