Some patients with diffuse nonpsychotic chronic disorders have long been identified as "difficult" patients (
1,
2,
3,
4 ). Although not well defined as a group, these patients share certain characteristics: heterogeneous and fluctuating symptomatology that is not easily diagnosed (
1,
2 ), difficulty in establishing a positive working alliance (
2,
3 ), active help seeking but ambivalent help-accepting behavior (
5 ), and consistent noncompliance with professionals' expectations (
4 ). Typical examples are patients with chronic affective disorders, patients with severe personality disorders, and patients with nonpsychotic diagnoses that shift between axes I and II and that are often combined with substance use disorders (
3 ).
Both the introduction of axis II in
DSM-III and the refinement of classification in
DSM-IV seem to have increased the ability to diagnose these patients' symptoms over the past 20 years (
3,
6 ). Many successful disorder-specific treatments have been developed. Chronic depression and borderline personality disorder have been transformed into delineated psychiatric disorders, resulting in more effective treatment for many, though not all, patients (
7,
8 ). However, patients with unclear, multiple, or shifting diagnoses do not fit into such treatments because they lack a
DSM-IV classification and therefore do not "exist" in the current nomenclature. Patients with nonpsychotic chronic disorders not otherwise specified have received little attention in recent professional literature. However, many professionals have frequent problematic encounters with patients in this group. The encounters are especially frequent in community mental health settings. These patients often receive community care because such settings use broader inclusion criteria for admission to treatment than specialty treatment settings and because the level of diagnostic specialization among professional staff is limited (
9,
10 ). The proportion of such patients in treatment populations varies across studies (10%–20%), and studies have shown that this group accounts for a large portion (50%–80%) of total mental health care costs (
11,
12,
13 ).
Despite the frequency of encounters with these patients and the substantial resources devoted to their care, they have not been well defined as a diagnostic subgroup. The frequency, nature, and urgency of these encounters and the problems experienced in community mental health settings in treating these patients are also poorly understood. More clarity and accuracy are necessary to develop adequate treatments and provide effective care for these patients. This study explored three research questions. What problems do mental health professionals perceive in providing community care for patients with nonpsychotic chronic disorders not otherwise specified? Which of these problems are considered most urgent? Which of these problems are considered most amenable to positive change through professional interventions?
Methods
A modified four-phase Delphi procedure was used to elicit and prioritize the views of mental health professionals about problems in the long-term care of patients with nonpsychotic chronic disorders not otherwise specified. The procedure was conducted in the Netherlands between June 2006 and March 2007. This patient group was defined on the basis of findings from a recent literature review (
4 ) and other relevant literature. Four categories of inclusion criteria were established: diagnostic difficulties, observed patient behavior, professionals' feelings toward patients, and length and intensity of mental health care use. [A list of criteria in each category is available as an online supplement to this brief report at
ps.psychiatryonline.org .] Patients with a clear diagnosis of a single disorder were not considered to belong to this group. Patients in this group should have no diagnosis (either definite or not otherwise specified) or they should have several coexisting psychiatric diagnoses or one or more shifting and thus unstable diagnoses. Because no patients were involved in this study, ethics approval was not required under Dutch law. Participants were fully informed of the Delphi procedure before it began.
To be eligible, Delphi participants had to have at least three years of experience working with this patient group and had to be employed in a nationally recognized center of expertise or be a nationally recognized expert on the basis of publications, lectures, or academic excellence. Experts were selected by searching recent literature and consulting with key figures in nationally recognized centers of expertise for "difficult" patients. Because research on these patients is not readily available, experts on difficult-to-treat patients and patients with chronic illness and high levels of service use were also considered eligible.
The expert panel consisted of eight mental health professionals, including two women, from different disciplines. Four were psychiatric nurses, two were clinical psychologists, and two were psychiatrists. Their ages ranged from 29 to 61 years. Treatment settings also varied. Five participants were from outpatient settings, two were from inpatient settings, and one was from a partial hospital. Six participants were from treatment settings not affiliated with an academic institution, and two were from university-affiliated institutions.
In round 1 of the Delphi procedure we used a focus group interview to elicit data, because the group format allows interaction between participants. It was facilitated by the first and second authors in a neutral space and lasted about 100 minutes. Discussion items were prepared by the researchers through a literature review (
4 ). However, items for discussion were mostly introduced by the experts in response to the opening question: What are the problems in psychiatric care for this patient group? The focus group interview was audiotaped and transcribed verbatim, and all text was manually coded through thematic analysis (
14 ) by use of MAXQDA text analysis software. All problems discussed in the focus group were described as precisely as possible, resulting in a list of 39 problems in five distinct categories—related to patients, professionals, their interactions, the family and social system, and the mental health system.
In round 2 the list of 39 problems in five categories was sent by e-mail to all participants for validation. They were asked whether it gave a complete and accurate description of the problems discussed. All participants returned the list, and comments were examined by the research team, which resulted in some alterations to the problem list.
In round 3 the 39 problems were scored by all participants. They were asked to rate the urgency of each problem: To what extent do you rate this an urgent problem in the daily psychiatric care for this patient group? The term "urgency" was discussed during the focus group. It referred both to the large extent of problems and to the immediate need to respond to them. Participants also rated whether each problem could be changed: To what extent do you rate this problem to be amenable to positive change through professional intervention? In all rounds the participants were explicitly encouraged to use the full scale, which had response categories ranging from 1 to 7.
Mean scores and standard deviations were calculated. Problems for which the rounded standard deviation was above 1.5 were interpreted as indicating disagreement with the other participants. In accordance with the Delphi procedure, for a score that differed substantially (>1.5 points) from the group mean, the participant was asked to elucidate the rationale behind the score. All such statements were summarized for each item.
In round 4 all participants again received the list of 39 problems, together with the mean group scores and the summarized statements from round 3. They were asked to reconsider their own score for each problem in the light of these clarifications. After all participants returned data from round 4, definitive means and standard deviations were calculated.
Results
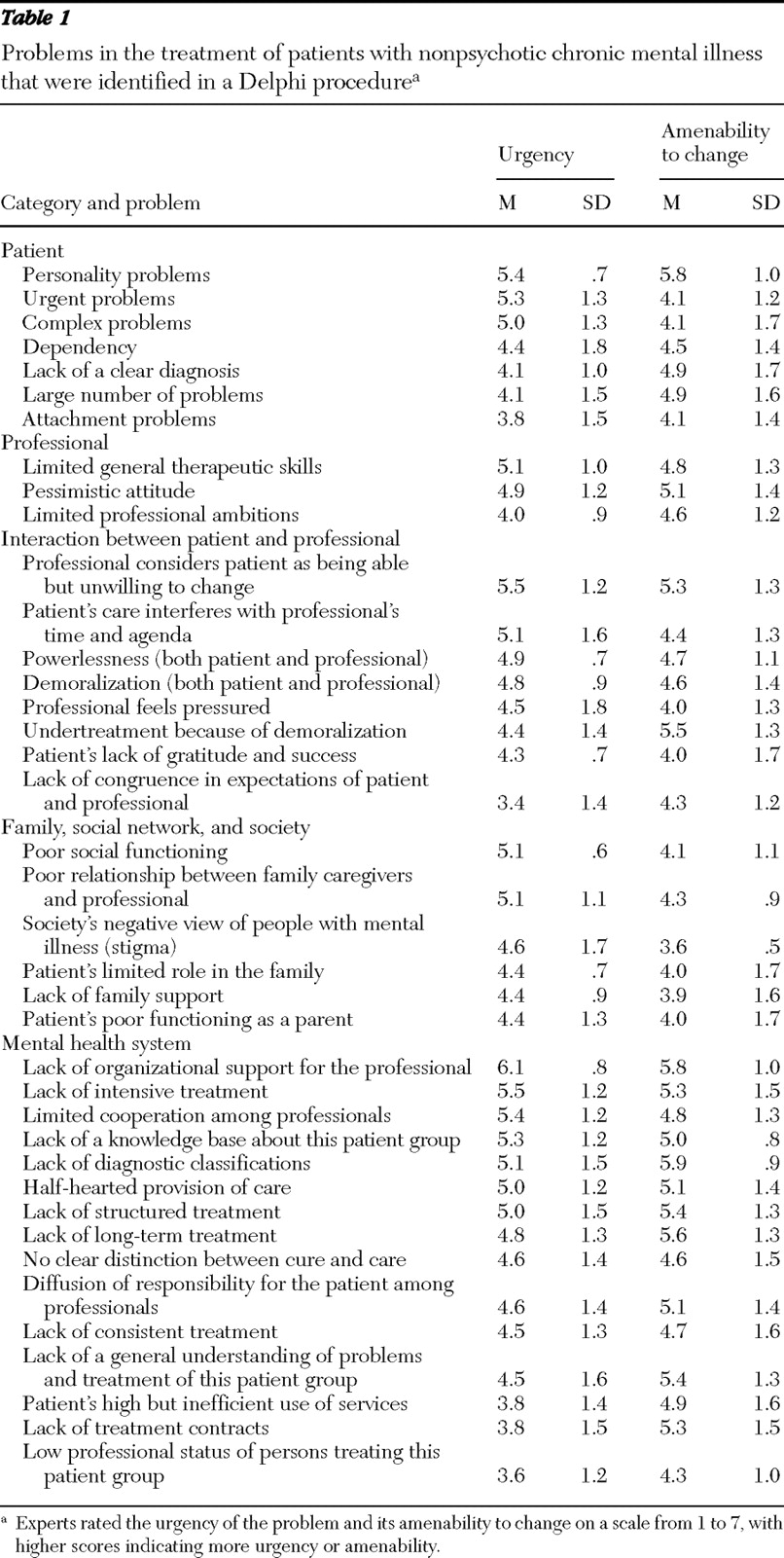
The participants' scores for the urgency and amenability to change of the 39 problems—a total of 78 scores—are shown in
Table 1 . Because 7 was considered to be the maximum score, the mean scores for all problems were quite high for both urgency (4.68±.59) and changeability (4.73±.59). The difference between these mean scores was not significant. To establish a clear distinction, we chose cutoff scores of 5.5 or higher for important items and 3.5 or lower for unimportant items and focused on those items.
Three items were highly urgent: belief that the patient is able but unwilling to behave differently, lack of organizational support, and lack of intensive treatment. Only one problem was rated as unimportant (≤3.5 in terms of urgency): a lack of congruence in expectations between the professional and the patient. In the area of amenability to change, scores for five items were particularly high: personality problems, undertreatment because of demoralization of both patient and professional, lack of organizational support, lack of proper diagnostic procedures, and lack of long-term treatment. No scores in this area were below the lower cutoff.
Although participants stated that they have some kind of "feeling" that helps them identify the patients in this group—in general those with personality problems—debate about their precise characteristics arose immediately in the focus group interview. All finally agreed on a working definition that patients in this group primarily have an axis II disorder in combination with a serious axis I disorder and often a substance use disorder. Participants noted that because the diagnoses of these patients tend to be unclear, tentative, or shifting, providing care was often problematic. This uncertainty precludes a clear treatment strategy and may result in patients' not being treated at all because professionals have no idea where to start.
The participants noted that these patients have many complex and urgent problems. They experience overwhelming problems in such areas as housing, finances, social contacts, health, family, and involvement with police. Intervention is problematic not only because of this complexity but also because these patients tend to ask for help in many different places—often the "wrong" places, such as asking the police for housing and asking housing services to provide psychological help. Participants attributed this style of help seeking mostly to the personality of these patients, which is characterized by dependency and by attachment problems.
In regard to problems related to professionals, the participants noted that the least educated and least experienced professionals tend to work most often with patients in this subgroup. A lack of general therapeutic skills was noted, especially self-reflection. Pursuing a "career in difficult patients" is currently very unattractive because it is difficult to advance in professional status in this field; thus many professionals "move up" to less difficult patients with more treatment possibilities as soon as they can. Study participants noted that professionals who continue to work with these patients have limited professional ambitions. They also spoke of the pessimistic and cynical attitudes among these providers. However, participants perceived and evaluated these attitudes differently. Some stated that cynicism is a necessary professional survival mechanism, and some believed that it indicates a lack of professionalism.
In the category of problems related to interactions, the scores highlighted one in particular: professionals consider patients as being able but unwilling to behave differently. Thus patients are thought to be in control of their difficult behaviors. The participants noted that these patients put pressure on professionals' time and agendas, which makes professionals feel pushed and responsible to intervene immediately ("to do something"). Their "space to maneuver" "becomes very limited." "Impossible" demands leave the professional feeling powerless and demoralized. Participants noted that professionals may be tempted to offer false hope or employ desperate interventions, such as admitting the patient to a hospital, referring the patient to another professional, or adding another medication without a clear rationale. Feelings of powerlessness may also lead to a lack of belief in treatment possibilities, the participants noted, resulting in undertreatment of problems that may in fact be treated effectively.
Family and social networks are largely absent in the lives of these patients. These patients—and the professionals who treat them—have few or no contacts with patients' family members. However, when family members do have contact with professionals, they often pressure them strongly. Participants noted that the social functioning of these patients is poor, that they have little to offer to or to expect from their families, and that they suffer from societal stigma. Generally, these patients have very little social support, which may result in use of mental health care for social reasons (for example, to ease loneliness), which is usually considered improper by professionals, the participants noted.
By far the largest number of problems were related to the mental health system. The problem with the highest score was a lack of organizational support for professionals working with these patients. Participants noted that expertise is diffusely spread out over teams, which inhibits collegial cooperation and accumulation of knowledge. The experts also noted that very few treatment options exist for these patients. The fact that current treatments are not a good fit for these patients was seen as a major problem. Some participants stated that they believed that these patients would cease to be "difficult" if they could participate in a program designed to meet their needs. Participants partly blamed the lack of suitable treatments on the poor diagnosis of these patients. They also criticized the term "difficult patients" because it may invoke half-hearted care, or what participants termed "pampering and dithering," and little interest in making additional therapeutic efforts. Substantial debate arose in the focus group about the value of better diagnosis of these patients versus their inevitable presence in the mental health system. Some experts stated that the label "difficult" served to keep these patients from view and distracted from a proper diagnosis. Others believed that the perceived difficulty of these patients stems largely from characteristics of the therapist and the organization and only partly from patient characteristics.
Discussion
This exploratory study revealed the types of problems that experts perceive in providing care for patients with nonpsychotic chronic disorders not otherwise specified. Among the highest-scoring problems, five are related to the mental health system, two are related to the interaction between patient and professional, and only one is related to the patient.
The study had several limitations. It was based on a small sample of eight experts. The Delphi procedure, however, can be well executed with small samples, especially when the sample is carefully drawn. The sample was created by consulting important stakeholders and inviting identified experts. The process resulted in a diverse group of men and women of different ages from varied professions who had specific expertise and experience working with this patient group. The Delphi procedure yielded only three problems deemed highly urgent and five problems deemed amenable to change, even though participants were strongly encouraged to use the full range of scores on the scale. We are not sure whether the small number of high-scoring problems is a consequence of our modified procedure (inclusion of a focus group) or of the multiple connections between problems, which would make it difficult to distinguish particularly relevant items. However, we analyzed a verbatim transcript of the focus group discussion, described the identified problems clearly, and asked all participants to review the problems and comment on their appropriateness in a separate Delphi round before scoring. Thus we believe that the small number of high-scoring problems is a valid outcome of this study.
The most striking finding is the difficulty that professionals reported to have in maintaining a positive attitude toward the patients in this group. Because these patients do not behave or seek help according to expectations, they are easily perceived as able but unwilling to change. Consequently, they are at serious risk of undertreatment because of professionals' negative attitudes. Also, because intensive treatment options and organizational support are limited, it is easy for both professionals and patients to become demoralized. The experts in our study believed that change is possible for these patients, but they had different ideas about how to bring it about—for example, by improving diagnostic classifications or by improving accessibility of services. An underlying question is whether the solution should be technical—make a correct diagnosis that results in effective treatment—or interpersonal—have a correct professional attitude that results in an improved therapeutic alliance and better treatment. Our guess is that both approaches are correct to a certain extent and that both should be exercised to improve patient care.
The concept of "illness behavior" (
15 ), which refers to the different ways in which individuals perceive, evaluate, and respond to symptoms, may be helpful because it offers a neutral, value-free vocabulary for describing help-seeking behavior that many would perceive as unusual. However, the distinction between symptoms and illness behavior can be very hard to make. Further research may result in a more correct psychiatric diagnosis for this patient group and may illuminate causes of their behavior other than psychopathological causes, such as sociodemographic variables, social consequences of having a psychiatric illness (for example, secondary gain), differences in patients' perceptions of their needs and in their use of care, and differences in the responses of various professionals and in various treatment settings (
15 ).
Conclusions
Apart from the lack of organizational support for professionals working with patients who have nonpsychotic chronic disorders not otherwise specified, the second most urgent problem is professionals' perception of these patients as able but unwilling to change. Diagnostic procedures—the area in which change was considered most likely—that focus not only on individual psychopathology but also on factors related to illness behavior may improve care.
Acknowledgments and disclosures
Funding for this study was provided by grant 100-002-031 from ZonMW Geestkracht and by Altrecht Mental Health Care and Gelderse Roos Mental Health Care. The authors thank the expert participants.
The authors report no competing interests.