Looking back almost 100 years, one finds that scattered reports have documented overrepresentation of black patients relative to white patients in psychiatric inpatient treatment facilities (
1,
2 ). Controlled studies, too, using data from the 1980 National Institute of Mental Health Survey of Mental Health Organizations (
2 ), the 1987 National Medical Expenditure Survey (
3 ), or the 1990 National Comorbidity Study (
4 ), and studies using data from the 1997 Practice Research Network sample drawn from patients of practicing psychiatrists (
5 ) indicated that blacks receive inpatient treatment more often than non-Hispanic whites. Results from studies with insured samples are mixed, with some (
6,
7 ) finding overrepresentation of blacks in inpatient settings and others, which sampled both adults and children, finding no racial disparity between blacks and whites (
8 ).
Inpatient psychiatric treatment is particularly stigmatizing to patients and may fuel mistrust of the mental health treatment system among blacks (
9,
10,
11 ). Studies show that the experience of involuntary hospitalization can deter black individuals from seeking subsequent mental health treatment (
12 ) and that blacks are less likely than members of other racial-ethnic groups to comply with outpatient referrals after hospitalization (
13 ). Furthermore, in community samples, fear of hospitalization is a more prevalent treatment barrier for blacks than for whites (
14 ). This avoidance of voluntary treatment may contribute to subsequent psychiatric crises that lead to future involuntary confinement, creating a vicious cycle of repeated hospitalization. Thus racial disparities in psychiatric inpatient care are particularly important to document and explain.
Previous studies consistently point to inpatient overrepresentation of blacks, but they do not address whether this overrepresentation is clinically appropriate. According to the Institute of Medicine, racial differences in treatment levels are legitimate if they reflect actual differences in treatment need (
15 ).
The presence of a diagnosed psychiatric disorder is an important indicator of treatment need. Black Americans, paradoxically, show lower rates than white Americans of diagnosable lifetime disorders (
16 ), but disorders among blacks can be especially severe and persistent. In addition, the prevalence of schizophrenia is higher among blacks than among whites (
17 ). Thus it is possible that the greater inpatient representation of blacks may be the result of differences in clinical factors. Many of the inpatient utilization studies cited above did not include psychiatric diagnosis or other important covariates, such as the use of outpatient services.
Previous studies also are limited in how much the results can be generalized, and few are recent. Nationally representative samples have been rare, and most studies were completed a decade or more ago and may not reflect the changing role of inpatient treatment in the contemporary mental health system. With improvements in pharmacotherapy (
18,
19 ) and the greater emphasis on community-based, rehabilitation-oriented alternatives (
20 ), inpatient hospitalization is often used for short-term crisis stabilization rather than for longer-term treatment (
21 ). In keeping with this trend, public and private health insurance plans prefer lower-cost outpatient treatment to more costly hospital stays. We have not yet begun to assess black-white inpatient disparities in this new era of inpatient care.
Explaining black inpatient overrepresentation also requires understanding the heterogeneity of the black population and understanding which individuals are most likely to be hospitalized. Whether born in the United States or immigrating to this country, black persons who trace their origins to a Caribbean island nation may be an important group to consider separately. Blacks of Caribbean descent compose about 4.4% of the U.S. black population, and they may be at higher risk of psychiatric hospitalization than other blacks. Data from several European countries indicate that schizophrenia is more prevalent among Caribbean blacks than among European whites and that Caribbean blacks have higher rates of psychiatric hospitalization (
22,
23 ), with particularly high levels among European-born Caribbean blacks (
24 ). U.S. data show a higher prevalence of schizophrenia among Caribbean-origin black males and more use of specialty mental health services, especially among second- and third-generation Caribbean blacks (
25,
26 ). However, these studies do not distinguish between inpatient treatment and other kinds of care.
In this study, we investigated whether African Americans and Caribbean blacks were more likely than whites to receive inpatient treatment—whether in psychiatric or nonpsychiatric settings—for psychiatric problems. We used a nationally representative sample of blacks and whites interviewed between 2002 and 2003, and we controlled for key covariates, including psychiatric diagnosis. We also examined heterogeneity within the black population, examining inpatient service use among African Americans and U.S.- and foreign-born Caribbean blacks.
Methods
Data and sample
Data were drawn from the National Survey of American Life (NSAL) and the National Comorbidity Survey Replication (NCS-R). These data sets were part of the National Institute of Mental Health Collaborative Psychiatric Epidemiology Surveys (CPES) initiative that included three nationally representative surveys: the NSAL, the NCS-R, and the National Latino and Asian American Study. CPES's objective was to collect data from representative samples of majority and minority adult populations in the United States on the prevalence of mental disorders, impairments associated with these disorders, and treatment patterns. Individually and collectively, the surveys provide the first national data that offer sufficient statistical power to investigate cultural and ethnic influences on mental disorders. Furthermore, these publicly available data sets allow users to combine data from the three surveys as needed to create unified, nationally representative samples for special purposes (
27,
28,
29 ). Further information on CPES, including design and methods, may be found on the study's Web site (
27 ).
The NSAL data were gathered to estimate physical, emotional, mental, social, and economic conditions of black Americans. Data were collected through face-to-face interviews in English and with a computer-assisted personal interview system after participants provided written informed consent. Interviews lasted an average of two hours and 20 minutes. The NSAL included a household probability sample of 3,570 African Americans, 1,621 blacks of Caribbean descent (hereafter referred to as Caribbean blacks), and 891 non-Hispanic whites aged 18 years and older. Consistent with NSAL data analyses recommendations (
30 ), 4,180 whites from the NCS-R were substituted for the NSAL white sample to allow for more robust racial-ethnic comparisons. The final sample size for analysis was 9,371.
African Americans were persons who self-identified as black but did not report Caribbean ancestry. Caribbean blacks were persons who self-identified as black and answered affirmatively to any of these inclusion criteria: they were of West Indian or Caribbean descent, they were from a Caribbean-area country, or they had parents or grandparents who were born in a Caribbean-area country. The Caribbean black sample was selected from residential areas that were sampled to reflect the distribution of the black population and from additional metropolitan areas where Caribbean blacks constituted more than 10% of the population. Data were collected between February 2001 and June 2003. The overall response rate was 72.3% for whites, 70.7% for African Americans, and 77.7% for Caribbean blacks. The publicly available NSAL data set contains no personalized identifiers. All study procedures were approved by the University Office for the Protection of Human Subjects.
Variables
Dependent variable. A series of questions embedded in the diagnostic portion of the structured interview assessed lifetime psychiatric hospitalization. For all included psychiatric disorders (described below), if participants met criteria for a disorder, they were asked whether they had ever been hospitalized overnight for that problem. This question was also asked of persons who reported ever making a suicide attempt. Persons not meeting criteria for any disorder were asked, "Have you ever in your lifetime been admitted for an overnight stay in a hospital or other facility to receive help for problems with your emotions, nerves, mental health, or your use of alcohol or drugs?" A yes response to any of these questions was classified as indicating lifetime psychiatric hospitalization.
Covariates. Several demographic and clinical characteristics identified in previous studies as influencing psychiatric hospitalization were included as control variables. These were income, employment, marital status, age, education, gender, any lifetime mental disorder, and lifetime receipt of psychotherapy or counseling.
Annual household income was measured as total monetary resources (dollar amount) from all sources. Employment status categories were defined as currently working (coded 1) versus not currently working (coded 0). Marital status categories were represented as a series of dummy-coded variables: never married (1) versus all other marital statuses (0); partnered (1) versus all other marital statuses (0); and separated, divorced, or widowed (1) versus all other marital statuses (0). Education was measured as the number of school years finished. Race-ethnicity was coded 1 for African American, 2 for Caribbean black, and 3 for white. Gender was coded 1 for female or 0 for male. Included in the lifetime psychiatric diagnosis indicator were the following disorders: panic disorder, social phobia, agoraphobia without panic disorder, generalized anxiety disorder, posttraumatic stress disorder, major depression, dysthymia, bipolar disorder, substance use disorder, eating disorder, oppositional-defiant disorder, conduct disorder, attention-deficit hyperactivity disorder, and separation anxiety. The NSAL structured interview does not generate schizophrenia-spectrum diagnoses.
Finally, a dichotomous variable indicated whether respondents had ever received any counseling or psychological therapy. The question read, "Did you ever in your life have a session of psychological counseling or therapy that lasted 30 minutes or longer with any type of professional?"
Analysis
Bivariate analysis identified relationships between racial-ethnic background and other demographic variables and lifetime psychiatric hospitalization. Design-based F ratios were used to report examined differences between groups.
We used logistic regression to estimate lifetime psychiatric hospitalization as a function of racial-ethnic background after controlling for sociodemographic indicators and lifetime psychiatric diagnosis. We first considered Caribbean blacks in aggregate and determined whether they, along with African Americans, differed from whites in hospitalization rates. In addition to odds ratios (ORs), we calculated marginal probabilities, expressing each group's likelihood of hospitalization after adjustment for covariates, and we compared adjusted probabilities with unadjusted probabilities from the bivariate analyses. We also conducted sensitivity analyses to evaluate whether our findings were sensitive to certain features of model construction. We then examined data separately for U.S.- and foreign-born Caribbean blacks, in comparison with data for both whites and African Americans.
We used the SVY LOGISTIC procedure of Stata 9.2 (
31 ) to estimate all models. All analyses used statistical weights to adjust for differential probabilities of selection and for nonresponse, and analyses were poststratified to represent the black population.
Results
Descriptive statistics
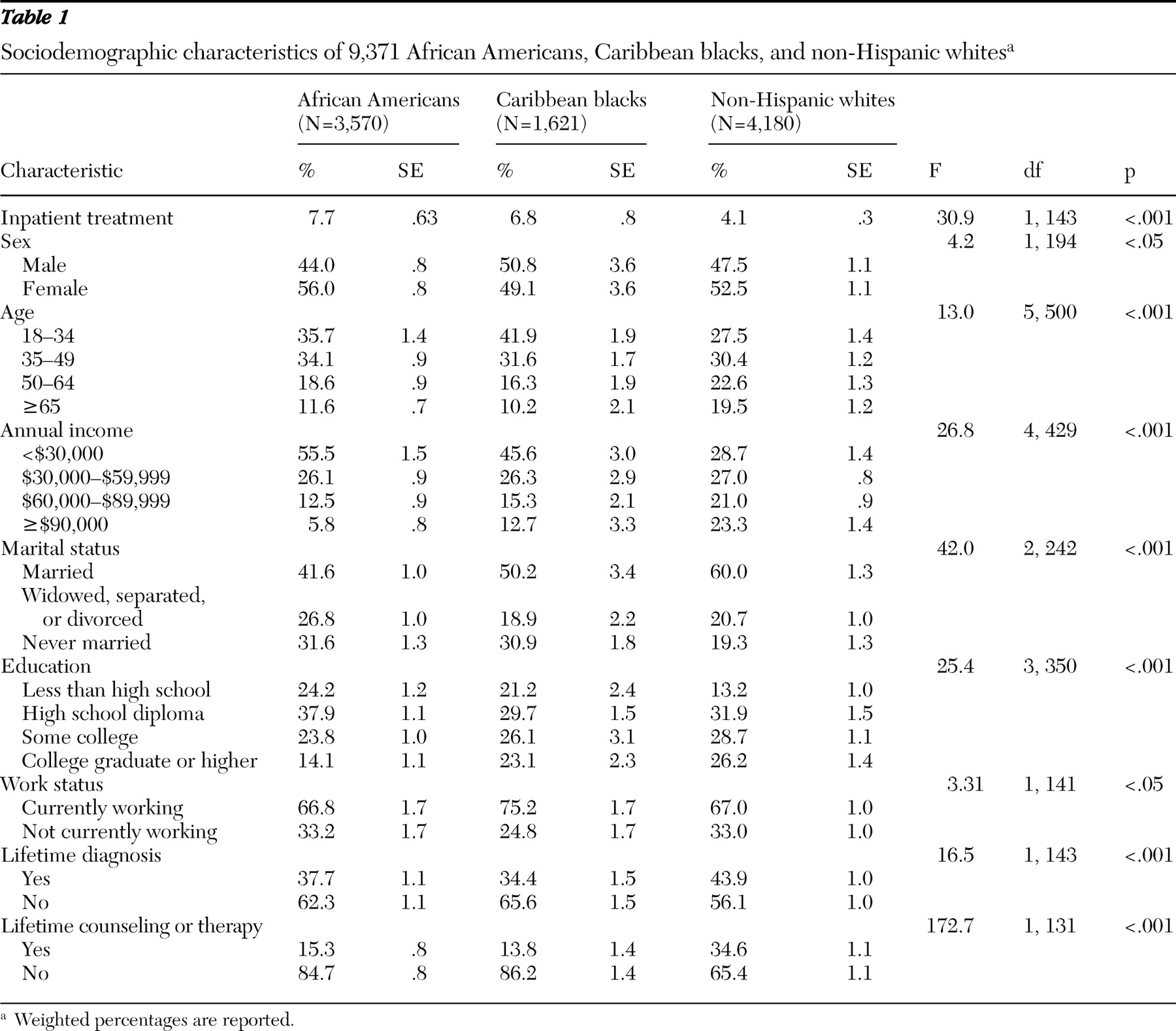
The means and standard deviations for key variables of interest are presented in
Table 1 . In our sample, women held a slight majority across groups, with the female-male ratio being slightly higher among African Americans than the other groups. African-American respondents were the least wealthy, with annual household incomes averaging $36,833, compared with $47,044 in Caribbean black households and $63,021 in non-Hispanic white households. Although respondents in this sample were likely to be married, the highest percentage of never-married persons was found among African Americans (N=1,176, 31.6%). The least educated were African Americans (mean±SD=12.4±.1 years) and Caribbean blacks (12.9±.2 years). Non-Hispanic whites had the highest prevalence of lifetime diagnosis for any mental health disorder (N=2,645, 43.9%), whereas African Americans and Caribbean blacks both had a prevalence about 10 percentage points lower.
Table 1 also indicates that more African Americans were hospitalized (N=271, 7.7%) than Caribbean blacks (N=83, 6.8%) or non-Hispanic whites (N=251, 4.1%), a statistically significant difference (F=30.9, df=1 and 143, p<.001). Thus before we entered sociodemographic and clinical controls into the analyses, African Americans, Caribbean blacks, and non-Hispanic whites were found to differ in inpatient treatment rates.
Multivariate analysis
Principal analysis. Logistic regression equations estimated differences in hospitalization rates after analyses controlled for sociodemographic and clinical covariates (
Table 2 ). Results indicated that both African Americans (OR=2.52) and Caribbean blacks (OR=2.74) were significantly more likely to be hospitalized than non-Hispanic whites (p<.001).
We calculated marginal probabilities of hospitalization and compared the probabilities after adjustment for covariates with unadjusted probabilities taken from
Table 1 . After adjustment, 8.5% of African Americans were hospitalized, compared with 7.7% before adjustment; 8.9% of Caribbean blacks were hospitalized, compared with 6.8% before adjustment; and 3.4% of whites were hospitalized, compared with 4.1% before adjustment. If anything, statistical adjustment for covariates tended to widen disparities.
Sensitivity analysis. We reanalyzed the multivariate model in three ways: using a different operationalization of the dependent variable (psychiatric hospitalization), including an independent variable for psychotic symptoms, and removing the independent variable of receipt of counseling or therapy. As previously reported, respondents were asked in two ways whether they had a personal history of psychiatric hospitalization. Those who did not meet lifetime criteria for an assessed mental illness were asked, "Have you ever in your lifetime been admitted for an overnight stay in a hospital or other facility to receive help for problems with your emotions, nerves, mental health, or your use of alcohol or drugs?" Respondents who met criteria for any diagnosis or reported a suicide attempt were asked whether they had been hospitalized for the reported illness or attempt.
By providing a psychiatric context for formulating responses, the latter approach to questioning might facilitate recall and, because respondents had acknowledged symptoms of mental illness, minimize the impact of stigma. We therefore repeated our principal analyses with the subsample of respondents asked about hospitalization in the context of reporting symptoms of mental illness or a suicide attempt. With this subsample, of which 78% of the persons were hospitalized, the results were at least as favorable, if not more favorable, to our hypothesis (African Americans, OR=2.69, CI=1.95–3.69; Caribbean blacks, OR=3.49, CI=2.31–5.29).
The NSAL interview did not allow for diagnosis of schizophrenia-spectrum disorders, an important predictor of psychiatric hospitalization. However, the interview did elicit information about psychotic symptoms. Respondents were asked six questions about their lifetime experience of hallucinations and delusions while awake and not under the influence of substances. We included in the multivariate regression model the total number of psychotic symptoms endorsed. There was no change in findings (African Americans, OR=2.52, CI=1.91–3.33; Caribbean blacks, OR=2.74, CI=1.96–3.83).
Receipt of outpatient counseling or therapy was positively associated with psychiatric hospitalization, indicating that it complemented inpatient care rather than, as had been expected, protecting against it. We therefore removed receipt of counseling or therapy and reanalyzed our data. ORs were slightly reduced, but results remained statistically significant (African Americans, OR=1.67, CI=1.31–2.13; Caribbean blacks, OR=1.84, CI=1.37–2.48).
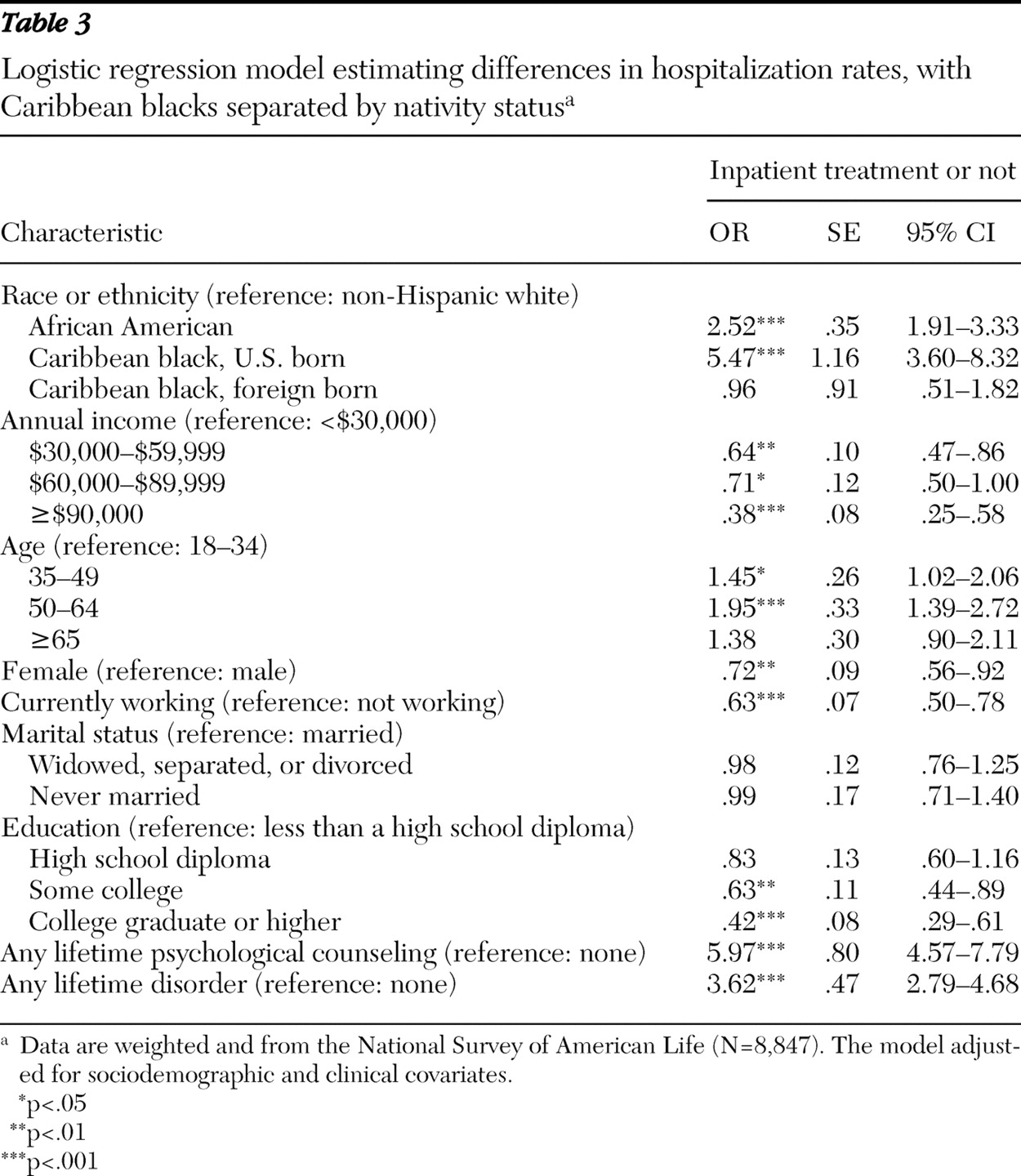
Caribbean blacks' nativity
Previous studies have reported that U.S.-born Caribbean blacks are especially likely to receive mental health treatment. To investigate possible differences among Caribbean blacks in psychiatric hospitalization, we separated respondents by U.S.-born and foreign-born status for further analysis. In a regression equation comparing U.S.- and foreign-born Caribbean blacks with non-Hispanic whites (
Table 3 ), the odds for U.S.-born Caribbean blacks of having any lifetime hospitalization were greater than the odds for non-Hispanic whites (OR=5.47) and appeared notably higher than the odds for African Americans. On the other hand, the odds of hospitalization for foreign-born Caribbean blacks were not significantly different from those of non-Hispanic whites (OR=.96).
To directly test for differences between the two Caribbean black groups and African Americans, an additional regression analysis was performed with African Americans as the reference group instead of non-Hispanic whites (data not shown). Results indicated that U.S.-born Caribbean blacks had significantly higher odds of being hospitalized than African Americans (OR=2.17, CI=1.45–3.23) and that foreign-born Caribbean blacks had significantly lower odds of hospitalization (OR=.38, CI=.20–.72). Thus the risk of hospitalization was highest for Caribbean blacks born in the United States, second highest for African Americans, and lowest for non-Hispanic whites and Caribbean blacks born outside of the United States.
Discussion
Like others before, we documented overrepresentation of blacks compared with non-Hispanic whites in inpatient psychiatric settings. Our data came from a nationally representative sample of community-dwelling individuals, and our research design controlled for important covariates, including psychiatric diagnosis.
Caribbean blacks born in the United States were more likely than foreign-born Caribbean blacks, as well as African Americans and non-Hispanic whites, to be hospitalized. This pattern may parallel the "Latino health paradox" (
32 ), whereby greater acculturation among Latinos is associated with more general medical problems and mental health problems. Such an explanation is consistent with data indicating that U.S.-born (
25,
26 ) and European-born (
24 ) Caribbean blacks have higher rates of mental illness, particularly schizophrenia, than other groups. It may be that U.S.-born Caribbean blacks experience pressure to accommodate and succeed in mainstream society while adhering to traditional Caribbean values, which might lead to higher levels of serious distress requiring inpatient treatment. The hypothesis that acculturative stress contributes to the elevated rate of hospitalization of U.S.-born Caribbean blacks remains to be tested.
The overrepresentation of blacks we observed in our study mirrored that of earlier studies (
1,
2,
3,
4,
5,
6,
7 ) despite changes in the mental health treatment system affecting when and where patients receive inpatient care. The number of inpatient psychiatric hospital beds declined by more than half between 1970 and 2000, largely because of a precipitous decline in state and county mental hospital beds where blacks were most overrepresented (
21,
33 ). However, psychiatric inpatient care itself actually increased between 1988 and 1994 (
34 ), as rates of general hospital discharges for mental illness rose almost 35% between 1995 and 2002. The increase in general hospital discharges for mental illness was particularly great among blacks (
35 ). Contemporary black overrepresentation might reflect a continuing higher inpatient placement rate, despite a shift toward short-stay, nonspecialty sector placement. The proportion of overrepresentation that is a contemporary disparity versus a historical artifact—a lingering effect of earlier cohorts—is a question for future research.
Several limitations warrant mention. First, we could not distinguish hospitalization for mental illness from hospitalization for substance abuse. We do not know which source contributes most to inpatient confinement or to the black-white differential.
A second limitation is that we lacked important contextual information that might have helped explain these racial differences in hospitalization rates. For example, we did not know whether treatment episodes were voluntary or involuntary or whether differences in levels of functioning at the time of hospitalization might help to explain differences in hospitalization rates.
Finally, schizophrenia-spectrum diagnoses were not available from the NSAL database. This limitation was mitigated by high comorbidity between schizophrenia-spectrum disorders and other assessed disorders (
36,
37 ) and by our supplemental analysis incorporating psychosis symptoms and demonstrating persistent overrepresentation of African Americans and Caribbean blacks. Nevertheless, schizophrenia-spectrum disorders are more often associated with higher rates of hospitalization than are many other disorders. If blacks have a higher prevalence of schizophrenia than whites (
17 ), then omitting this disorder might lead to an overestimation of black-white hospitalization differences.
Conclusions
Overall, results from this study indicate that black-white disparities persist in inpatient hospitalization. These disparities did not appear to be accounted for by differences in prevalence of psychiatric disorders. Furthermore, global racial-ethnic group comparisons covered up important sources of heterogeneity within the black population.
Acknowledgments and disclosures
This study was funded by faculty grants.
The authors report no competing interests.