Concern has increased in recent years about the availability of mental health services in rural areas (
1 ), especially for people with serious mental illnesses. Assertive community treatment (ACT) has emerged as a widely used evidence-based practice for providing services to people with serious mental illnesses (
2 ). To date, however, there have been few efforts to provide ACT in rural areas (
3,
4 ).
Since 1987 the U.S. Department of Veterans Affairs (VA) has developed a large national network of programs based on ACT principles. Its mental health intensive case management (MHICM) program conforms to the ACT program criteria pertaining to human resources, organizational boundaries, service delivery, and substance abuse treatment (
5 ). MHICM currently operates at over 100 VA facilities, serves over 6,000 veterans per year, and has been shown to result in reduced hospital use and symptoms and in improved quality of life and client satisfaction (
5 ).
Within the MHICM program, several teams serve veterans in rural areas. Because the few studies of ACT in rural settings have been based on research specifically intended to evaluate the application of ACT to such areas, they have not allowed comparison of client characteristics or patterns of service delivery between rural and urban settings. The VA program is national in scope and has gathered uniform monitoring data on all participating teams and veterans. Administrative data obtained from VA MHICM programs thus offer a unique opportunity to compare the delivery of these services in urban and rural areas.
In this study we used rural-urban commuting area (RUCA) codes developed in 1998 at the University of Washington (
depts.washington.edu/uwruca/about.html ) and national evaluation data from the MHICM program to identify the types of settings where veterans lived, which ranged from large urban locations to isolated rural ones. Demographic, clinical, and community adjustment characteristics of veterans residing in each kind of community were compared along with patterns of MHICM service delivery. Because the VA program is not exclusively targeted to veterans living in rural areas, these comparisons allowed us to characterize distinctive client characteristics, needs, and patterns of service delivery for MHICM clients residing in various communities and may provide a foundation for the further development of intensive programs to serve people with serious mental illnesses in rural areas.
Measures
Each veteran's zip code of residence was identified by merging MHICM intake assessment data with the VA outpatient encounter file. Residential areas were delineated with the zip code of residence on the first MHICM outpatient encounter record. These zip codes were matched with zip code-specific RUCA categories (
depts.washington.edu/uwruca ) that classified each veteran's residence as urban, large rural city, small rural town, or isolated rural community. RUCA is a subcounty measure of rural and urban status based on census tracts. Thus it is based not only on the size of cities and towns but also on their functional relationships as measured by work commuting flows. There are 33 codes that allow demographers, health care researchers, policy makers, and others to aggregate data according to their needs. We used a four-group aggregation, which is often used by health care researchers.
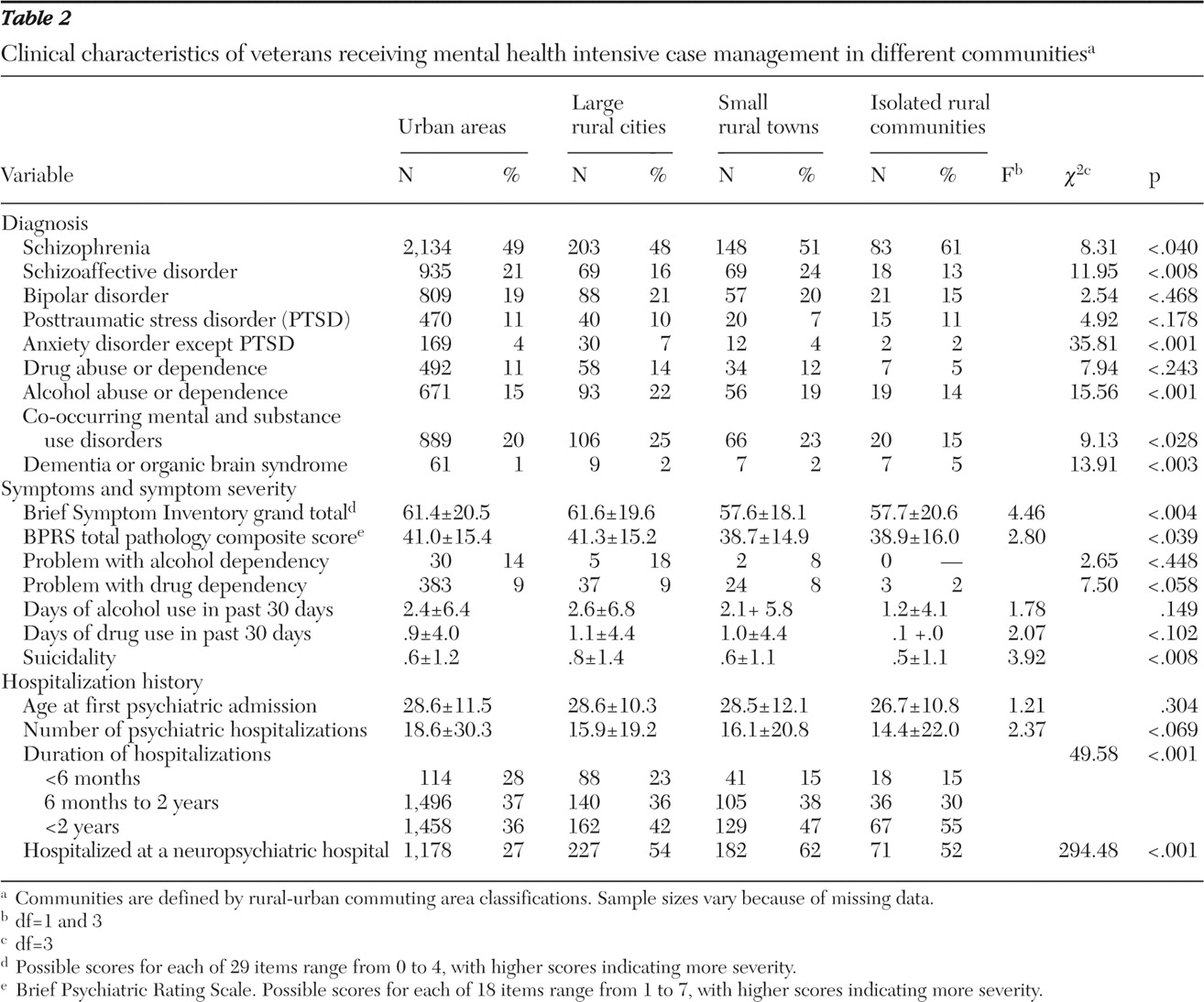
Sociodemographic measures included age, gender, race, education, marital status, employment, income, disability status, and assignment to a representative payee or fiduciary to manage the veteran's funds. Clinical measures included the diagnosis assigned to each veteran by his or her treating clinician at the time of enrollment in MHICM. The Brief Psychiatric Rating Scale (
9 ) was used to measure symptom severity, and the Global Severity Index of the Brief Symptom Inventory (
10 ) was used to measure subjective distress. Selected questions from the Addiction Severity Index documented alcohol and drug use in the previous 30 days (
11 ). Self-reported hospitalization data included age at first hospitalization, the number and duration of psychiatric hospitalizations, and whether the veteran's most recent VA hospitalization was at a traditionally long-term neuropsychiatric facility (similar to state mental hospitals and often located in rural areas) or at a more acute care-oriented, urban, general medical and surgical hospital.
Community adjustment was evaluated by using information on type of residence (independent housing, slightly to moderately structured housing, or highly structured housing), on overall functioning as assessed by the Global Assessment of Functioning (
12 ), and on selected items from the Lehman Quality of Life Inventory (
13 ) to assess satisfaction with life in general and with living arrangements, friendships, and family relationships. Violent behavior in the past month was rated on a scale from the National Vietnam Veterans Readjustment Study (
14 ). Role functioning was assessed with the Instrumental Activities of Daily Living (
15 ). Veterans were also asked whether they had been arrested or spent a night in jail for any reason during the previous six months.
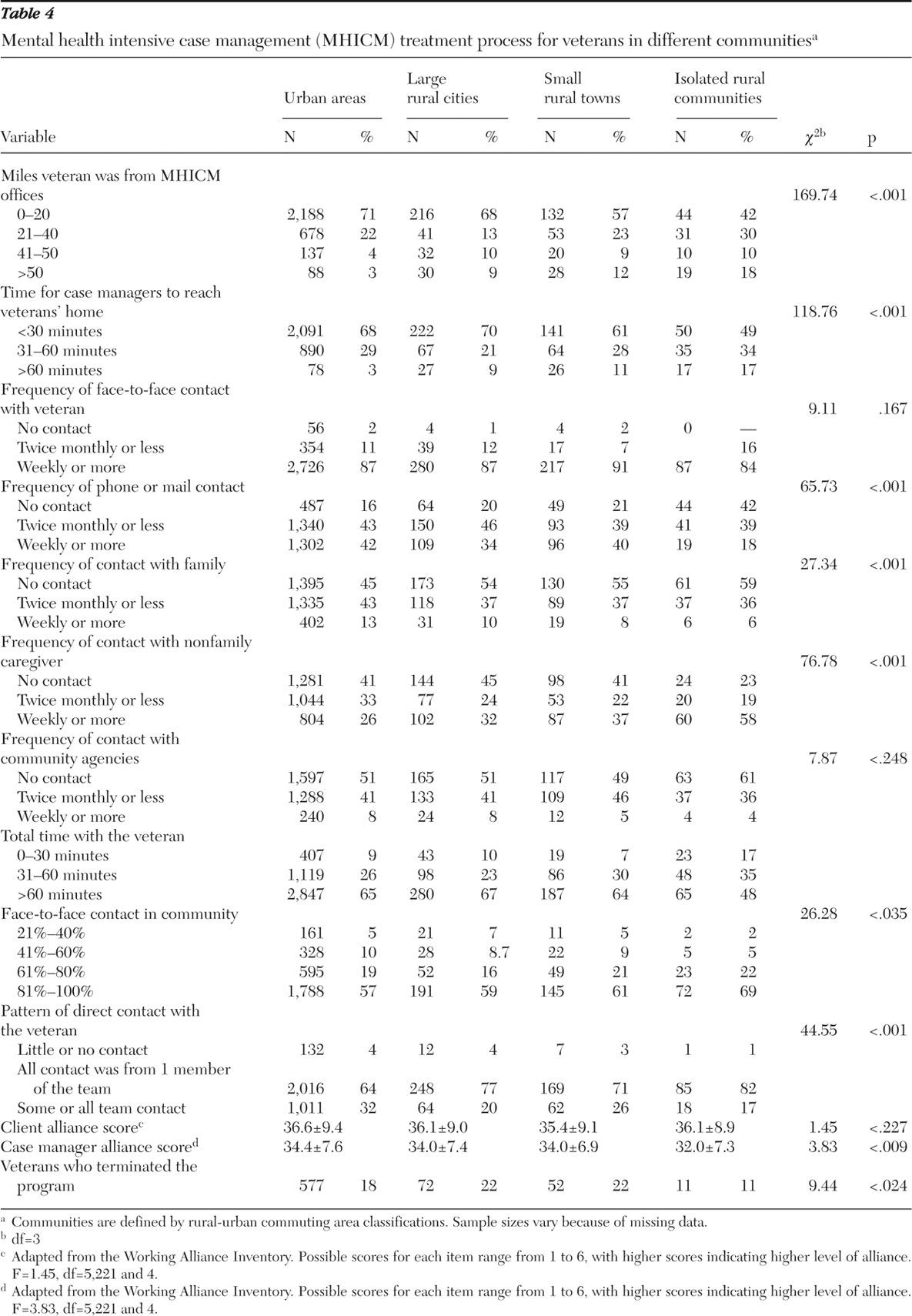
To assess MHICM treatment processes, case managers completed semiannual structured summaries of the MHICM services provided to each veteran. We present information from the first of these assessments, which documented distance and travel time from MHICM staff offices to the veteran's home as well as the frequency of face-to-face contacts, telephone contacts, contacts with family members, and contacts with nonfamily caregivers. The duration of contacts and case manager ratings of therapeutic alliance with the client were also recorded. Therapeutic alliance was assessed with parallel case manager-client versions of seven 7-point Likert questions about the nature of the clinical relationship, which were adapted from the Working Alliance Inventory (
16 ) for use in case management programs (
17 ). The form also documents general types of services that were provided during the six-month period (rehabilitation, psychotherapy, crisis intervention, managing psychiatric medications, screening for medical problems, and providing substance abuse treatment, housing, and vocational support).
Analysis
First we present descriptive data about the sample. Veterans receiving MHICM and living in various urban and rural communities were compared with a reference group of all VA patients who had a diagnosis of schizophrenia and were living in such communities. The comparison group represented a highly vulnerable population that was likely to be similar in needs to those served by the MHICM program. Next, we compared the sociodemographic and clinical characteristics and the community adjustment of MHICM clients receiving services in urban, large rural, rural, or isolated rural areas. Further, we compared patterns of MHICM service delivery among clients living in the different communities. Chi square analysis was used to test the significance of differences in categorical measures. Analyses of variance and covariance were used to compare continuous variables.
Discussion
ACT is a widely implemented evidence-based model for providing services to people with serious mental illnesses (
18 ), and the VA has been implementing MHICM, an intensive psychiatric community care program based on ACT principles, on a national basis for over two decades. This study used VA administrative data to examine the characteristics of veterans residing in urban areas, large rural cities, small rural towns, and isolated rural communities who received treatment from MHICM and to compare patterns of service delivery in these different geographic areas. Comparison of the 5,221 veterans enrolled in the MHICM program between FY 2000 and FY 2005 with 81,818 veterans treated for schizophrenia in other VA programs in FY 2006 showed that MHICM clients were less likely to come from large urban areas, slightly more likely to come from moderate-size cities, but less likely to come from small rural towns or isolated rural areas.
MHICM veterans residing in isolated rural areas were significantly more likely to be unemployed, to receive VA disability compensation, and to have a payee or fiduciary. Although they appeared to have more severe disabilities than those from other areas, these differences were modest in magnitude. Greater proportions of MHICM clients in rural areas were diagnosed as having schizophrenia or organic brain syndrome, and they had spent more time in psychiatric hospitals than clients in urban areas. When we controlled for the effect of hospitalization at neuropsychiatric hospitals, symptom severity among clients in rural areas was not significantly different compared with those in other communities. Differences in past hospital utilization and disability remained significant between MHICM veterans living in different types of communities. These data demonstrate that there were sizeable numbers of veterans living in rural and especially isolated rural areas who received MHICM services, and their clinical characteristics were similar to those of veterans provided MHICM services in urban areas.
Veterans living in rural areas spent more time than those in other communities living in residential facilities with minimal to moderate supervision, to which they were most likely transferred to extended stays in long-term inpatient units, many of which have closed in recent years. They thus appeared to have been modestly less likely than veterans in urban areas to be living in either independent housing or in highly structured facilities. It is also possible that because there are fewer hazards of exposure to crime, drug dealing, or street traffic in isolated rural settings, less supervision is needed or that the potential isolation of living independently in a rural area makes group living more appealing. It is notable that veterans living in isolated rural communities had higher levels of satisfaction with life than MHICM participants from other areas.
As expected, rural veterans lived farther away from the MHICM team offices and it took MHICM staff significantly more time to travel to their residences. But it is also notable that even among MHICM clients living in isolated rural locations, only 18% (N=19; data missing from denominator) were located more than 50 miles away and only 17% (N=17; data missing from denominator) lived more than 60 minutes away from the nearest VA facility. Although the current MHICM teams clearly serve some veterans living in rural areas and these veterans had needs similar to those served in urban areas, the program did not seem to reach people living in areas that are more remote from VA centers. There may thus be a need for additional programs, particularly programs that specialize in rural service delivery to assist veterans who live beyond the reach of standard MHICM programs.
As expected, veterans living in more rural areas who were served by these programs had slightly less frequent contacts with MHICM staff but were seen somewhat more frequently in the community rather than at the medical centers, possibly because of distance and travel time. However, because of the categorical nature of the distance variable, this association could not be statistically verified. Also, more veterans in rural areas received services from just one case manager rather than from the entire multidisciplinary team that is characteristic of ACT. The greater travel times may make multiclinician team visits less efficient and less practical. Veterans' contact with their families was also less frequent in rural areas, but contact with nonfamily caregivers was more frequent, perhaps because of the greater use of moderately restrictive supervised housing.
It is notable that although the discrepancy between service intensity among rural and urban veterans was small, a smaller proportion of veterans in rural areas received recovery-oriented services, such as rehabilitation services, psychotherapy, or practical assistance with housing or vocational support. Less frequent delivery of such services to rural participants could reflect the fact that the focus of case managers during their contacts may be limited to community maintenance and symptom monitoring rather than skill building or other recovery-oriented services.
It is encouraging that the MHICM program serves a substantial proportion of veterans living in rural areas, although a somewhat smaller proportion than among general VA mental health patients diagnosed as having schizophrenia. Although MHICM participants who live in rural areas have problems generally similar to those living elsewhere, these programs do not seem to have served many veterans in settings more than 50 miles from VA offices, and veterans in rural areas received less intensive and less recovery-oriented services.
To meet these needs, the VA Strategic Mental Health Plan, the VA's response to the President's New Freedom Commission on Mental Health, called for a demonstration program to be implemented at rural locations, with the goal of delivering the full array of MHICM services to veterans with serious mental illness in rural and isolated rural settings. This 20-site demonstration, which is named MHICM Rural Access Networks for Growth Enhancement (RANGE), was implemented in FY 2007 and was based on the assumption that smaller rural MHICM programs would need to better coordinate their services with those of the parent VA facility to ensure proper medical and psychiatric care and make greater use of telemental health technologies. The RANGE program should provide valuable additional lessons and quantitative data to inform future delivery of intensive community-based services to people with serious mental illness in rural settings. The VA continues to recognize the need for reaching out to veterans living in rural areas, and the Veterans Health Administration's mental health handbook strongly encourages VA medical centers to offer MHICM services to rural veterans (
19 ).
Two limitations of this study require comment. The RUCA coding system is imperfect, because single zip codes can often include several different kinds of communities (for example, small rural towns and isolated rural communities). In addition, the representativeness of our sample and its relevance to systems other than VA (nonveterans systems) are unknown.