Burnout in human service occupations is of interest to researchers and practitioners in the mental health field (
1 ). Mental health professionals face additional strain by the very nature of mental health work and therefore may be more at risk than their colleagues in other areas of health care (
2 ). Maslach and colleagues (
3 ) have described burnout as a point at which important, meaningful, and challenging work becomes unpleasant, unfulfilling, and meaningless. Energy turns into exhaustion, involvement leads to cynicism, and efficacy is replaced by ineffectiveness. Personal and organizational factors have been associated with stress and burnout (
4 ), whereas job satisfaction was found to have a protective effect against them (
5 ). In Italy, psychological well-being of health care professionals working in different settings has been examined (
6,
7,
8,
9 ), but no study has been published on the association of job satisfaction, burnout, estimated psychiatric morbidity, and stress factors among mental health staff.
Psychiatric treatment in Italy underwent a radical change in 1978 with the passing of Law 180. Legal provisions sanctioned the replacement of psychiatric hospitals with health service facilities organized on a regional basis and integrated with the general hospital system. Although the theoretical model is universally accepted in principle throughout Italy, achievement of homogeneous results and practical application among the different regions of Italy is still difficult. Milan is in Lombardy, a northern region, and the city's reorganization of its health service facilities nearly achieves the structure described in the aspirational principles of Law 180. The basic structure in Milan is the Department of Mental Health, which is ultimately responsible for prevention, care, and rehabilitation in connection with mental illness in the adult population. The department also provides for emergency treatment at home or at hospitals; it provides acute admissions wards and hospital first-aid (emergency) units. In order to carry out their mental health programs, the Department of Mental Health draws on the services of outpatient centers or health clinics that provide treatment in a hospital setting or in residential or semiresidential communities.
The exploratory cross-sectional multicenter survey reported here aimed primarily to evaluate the prevalence of burnout and estimate psychiatric morbidity and job satisfaction among psychiatrists working in the Italian Public Health System hospitals in Milan. An additional aim was to investigate personal and environmental factors that may contribute to burnout.
Methods
A cross-sectional, descriptive, multicenter survey was coordinated by the Psychiatric Clinic, Fondazione IRCCS, Ospedale Maggiore Policlinico of Milan. All six departments of psychiatry within the Italian Public Health System in Milan were invited to participate. One department refused to participate because of concerns about insufficient time and organizational problems, leaving five departments of psychiatry that participated in the study. The survey was conducted from January 2007 to July 2007.
All of the departments were sent a set of test materials for each health care professional and were given a deadline of two weeks to return the survey, with a guarantee of anonymity. Institutional review board approval was obtained. Each department then collected all of the responses and sent the forms to the coordinating center, which excluded any forms that had not been correctly completed.
Each participant completed the Maslach Burnout Inventory (MBI) (
10 ), the 12-item version of the General Health Questionnaire (GHQ-12), the job satisfaction section from the Job Diagnostic Survey (JDS) (
11 ), and a study-specific questionnaire. We briefly describe these next.
The MBI is a 22-item self-completed questionnaire with the following subscales: emotional exhaustion, depersonalization, and reduced personal accomplishment. The respondent is asked to reply to each question, using a Likert scale to identify the frequency of the event over time (from 0, never, to 6, every day). Normative data for the Italian version of the MBI were used for dichotomizing the burnout scales (
12 ).
The GHQ-12 is a screening instrument that is mainly used in community medicine and occupational settings (
13 ). According to the Italian validating study (
14 ), the instrument has a sensitivity value of 75%, specificity value of 74%, positive predictive value of 50%, and negative predictive value of 90%. It consists of 12 questions designed to investigate 12 frequent psychiatric symptoms. Each item is scored 0, for "less or not more than usual," or 1, for "more or much more than usual." The sum of each of the item scores gives an individual score that can range from 0 to 12. Individuals scoring 4 or more are estimated to have psychiatric morbidity, and this threshold was applied.
We used the Italian-validated form of the job satisfaction section from the JDS (
11,
15 ). The section consists of five items, each measured on a 7-point Likert scale, where a higher score represents greater general job satisfaction.
Finally, we designed a 32-item questionnaire specifically for this study. Items were derived from the international literature and from a pilot study involving the physicians and nurses of the coordinating center. In addition to demographic variables, we investigated level of experience and work setting. Finally, we included items about sources of stress related to working environment and sources of stress related to patients, each scored 0 for no or 1 for yes.
A total of 115 questionnaires were distributed to the psychiatrists working in all five departments of psychiatry in Milan who were willing to participate. A total of 91 questionnaires were returned, of which ten were excluded because they were only partially completed, leaving 81 (70%) questionnaires for the analysis. There was no significant difference between respondents and nonrespondents in demographic variables or job characteristics.
SPSS for Windows Version 11.0 was used to analyze the data. For quantitative data, descriptive statistics are presented as frequency and percentage distributions for categorical data and as means and standard deviations for continuous data. Given that a major purpose of this study was to investigate personal factors and factors of the working environment that may contribute to burnout, we first conducted bivariate analyses to compare each of the exploratory variables (GHQ-12 and JDS job satisfaction scores, demographic characteristics, level of work experience, time in current job, work setting, stress factors related to working environment, and stress factors related to patients) with the MBI subscale scores. We then performed a series of linear regression models, entering exploratory variables that met a threshold of statistical significance (p<.05) as potential predictors and entering MBI subscale scores as dependent variables.
Results
The mean±SD age of participants was 46.78±8.58 years. Most psychiatrists (N=47, 58%) were women. Forty-six (56%) psychiatrists worked in outpatient settings, 28 (35%) worked in acute wards, and seven (9%) worked in community settings. Finally, most respondents (N=69, 85%) had ten or more years of experience. For the MBI, the mean±SD scores were 21.33±13.28 for emotional exhaustion, 6.43±6.66 for depersonalization, and 35.78±8.94 for personal accomplishment. Using cutoff points suggested by Sirigatti and Stefanile (
12 ) for Italian mental health workers, the scores indicated a high level of emotional exhaustion for 40 (49%) psychiatrists, a high level of depersonalization for 32 (39%), and a low level of personal accomplishment for 18 (22%).
The mean±SD GHQ-12 score was 2.22±2.68, and the JDS job satisfaction score was 4.33±1.12. If we consider a cutoff score of ≥4 as an index of psychiatric morbidity (
13 ), 19 (23%) psychiatrists had an 80% probability of having a psychiatric disorder as described by Goldberg and Williams (
13 ).
In responses about sources of stress related to the job and to their patients, physicians seemed to be more stressed by excessive workload (N=49, 60%), inadequacy of health care facilities (N=49, 60%), and lack of funds (N=32, 39%) and by working with aggressive (N=41, 51%) and demanding (N=34, 42%) patients.
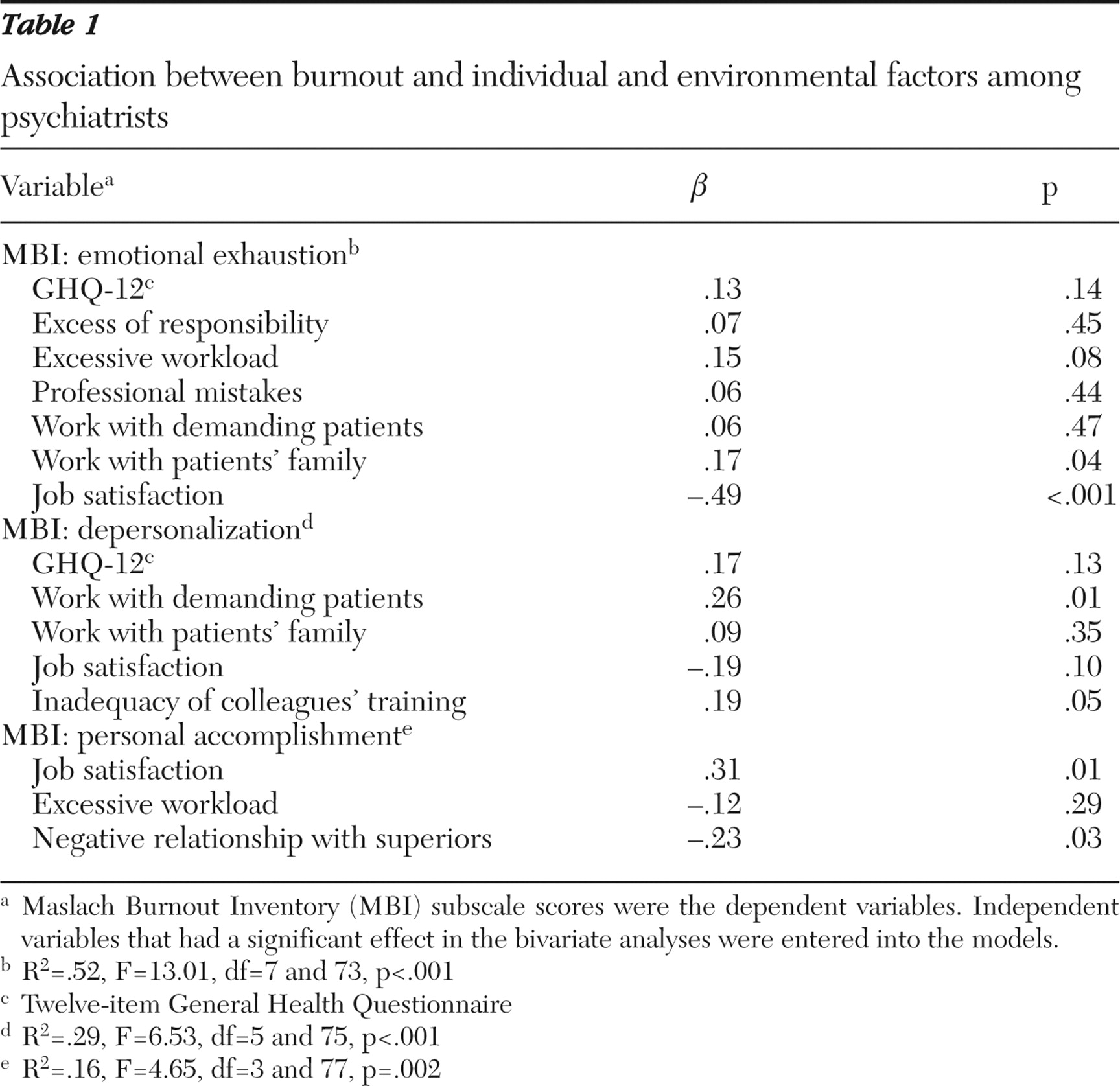
Table 1 shows the results of linear regression models that explored which personal characteristics and factors of the work environment contributed to the explanation of the dependent variables (MBI subscale scores). Potential predictors were the variables that met a significant threshold in preliminary bivariate analyses.
In the model for emotional exhaustion, low job satisfaction and work that involved patients' families remained significant. Depersonalization seemed to be associated with working with demanding patients, whereas reduced feelings of personal accomplishment seemed to be directly related to job satisfaction and inversely associated with a negative relationship with superiors.
Discussion and conclusions
The most striking findings of the survey were the high levels of emotional exhaustion and feelings of depersonalization. The rating of emotional exhaustion was 49%, which was almost double the rate reported by Bargellini and colleagues (
7 ) among physicians working in anesthesiology and intensive care, by Grassi and Magnani (
6 ) among hospital physicians, by Renzi and colleagues (
8 ) for dermatological health care staff, and by Klersy and colleagues (
9 ) among health care providers of dialysis. At the same time, the ratings of depersonalization were much higher in comparison with rates reported in these other studies. These data suggest that mental health workers may be more at risk of burnout than their colleagues who work in general medical care, as observed by Moore and Cooper (
2 ). High emotional involvement and high idealistic expectations among mental health workers allow one to achieve a high level of professional satisfaction; however, these factors can also produce high levels of stress and frustration if they lead to an excessive sense of responsibility and impotence toward chronic and invalidating pathologies.
The scores on all three MBI subscales were not significantly different from those of studies conducted in the United Kingdom (
5 ). According to GHQ-12 scores, estimated psychiatric morbidity was 23%. These data are similar to those found in the Italian normative sample (22%), in a sample of general practice and hospital physicians (20% and 24%, respectively) (
6 ), and to findings in the British literature (22%–30%) (
5 ).
In our sample, psychiatrists considered factors linked to the place and organization of work to be more stressful than other factors. Several studies have highlighted the role of perceived workload and organizational problems in the development of burnout (
4 ). Maslach and colleagues (
3 ) have argued that the main causes of burnout are related more to the working environment than to personal characteristics, and therefore preventive steps should be taken to improve the factors related to the working environment. Regarding factors linked to patients' characteristics, physicians perceive aggressiveness to be the most stressful factor, according to other studies in literature (
4 ).
According to the regression model, job satisfaction predicted lower levels of emotional exhaustion (a negative effect) and higher levels of personal accomplishment (a positive effect), as reported by many studies in literature. This relationship suggests that job satisfaction plays a protective role against the development of burnout (
1,
5 ). The association of emotional exhaustion with the variable for working with patients' families can be explained by the fact that for physicians, being with patients' relatives often means confronting the inadequacy of the health care system and psychiatrists' own impotence in satisfying the high, and sometimes unrealistic, expectations of the relatives. The relationship between the depersonalization subscale and the variable for working with demanding patients showed the negative effects of burnout on psychiatrists' ability to relate with patients. Finally, the inverse association between personal accomplishment and a negative relationship with superiors is in line with findings reported by Leiter and Harvie (
1 ). A higher level of personal accomplishment was associated with a perception that the decision process is democratic, not "top down," that decisions are based on awareness and accurate information, and that staff are involved in decisions influencing their work.
Some of the limitations of this study deserve comment. First, the cross-sectional design of the survey did not allow for the establishment of causal relationships between the variables investigated with the study-specific questionnaire and the prevalence of burnout. Prospective cohort design may be used to further understand which factors predict burnout.
Second, no standardized interviews were conducted to diagnose psychiatric disorders among respondents with high GHQ-12 scores. It is well known that psychometric tests cannot replace a formal psychiatric evaluation and that persons with a high GHQ-12 score should be evaluated by a psychiatrist.
Furthermore, using only a self-report style of questionnaire may have affected the results. To better understand how sources of stress influence staff members' well-being and views of their jobs, a qualitative study may be conducted to allow consideration of how burnout and poor mental health might be prevented or improved among mental health staff. Another limitation is related to the fact that almost 30% of psychiatrists refused to participate in the survey. On the one hand, it is possible that nonrespondents presented higher levels of burnout and dissatisfaction than respondents. On the other hand, according to Renzi and colleagues (
8 ), it is possible that totally satisfied professionals did not complete the survey because they felt they had nothing to complain about.
Acknowledgments and disclosures
The authors report no competing interests.