There are important reasons for mental health clinicians to be interested in the physical health of their patients. Physical illness occurs among more than 45% of psychiatric outpatients and often goes undiscovered (
1,
2,
3,
4,
5,
6 ), leading to lower quality of life, decreased functioning, and increased risk of early death (
7,
8 ). Individuals with severe mental illness die earlier than the general population because of poor health behaviors, medication side effects, inadequate preventive care, and insufficient medical care (
9,
10,
11,
12 ).
Primary care interventions that address the physical health of persons with mental illness include care coordinators, specialized primary care clinics, and medical teams within psychiatric settings (
11 ). An expanded medical role for mental health clinicians has been suggested but is less studied (
13 ).
Persons from racial and ethnic minority groups with comorbid physical and mental illness face even greater disparities in medical care, including low rates of treatment for chronic pain, asthma, hepatitis, and diabetes (
14,
15 ). However, most health disparities research examines physician behavior in nonpsychiatric settings. In mental health settings that serve as safety-net treatment facilities, social workers, psychologists, and nurses provide the majority of treatment, suggesting a need to examine their assessments of physical illness (
14,
16 ).
What degree of physical health management is reasonable to expect of mental health clinicians, particularly those with little medical training? Professional competencies for psychiatry, nursing, psychology, and social work all require elements of physical health management. The Group for the Advancement of Psychiatry recommends that psychiatrists facilitate follow-up for physical problems that are caused by psychiatric treatment, interact with psychopathology, or disproportionately affect psychiatric patients (
17 ). Current practice guidelines echo these recommendations (
18 ). Psychiatric nurse practitioner competencies also require monitoring for physical complications of psychiatric illness and treatment and making medical referrals where necessary (
19 ).
Although psychologists are not trained to assess physical illness, they are encouraged to consider psychological problems holistically in the context of other problems and illnesses (
20,
21 ). Competencies of clinical social workers also include a limited medical role. This includes attentiveness to the physical signs of illness and side effects of medications, as well as making medical referrals (
22 ).
This article addresses a gap in the health services literature by examining how mental health clinicians assess and respond to physical illness during mental health intake visits with an ethnically diverse group of patients (
14 ). Using a mixed-methods approach, we present physical illness discussions in patient-provider interactions, adding qualitative data analyses to enrich our understanding of clinician assessments of physical illnesses during evaluations.
Methods
Sample
Data were from the Patient Provider Encounter Study (
23 ). In this study, a patient's initial intake session was videotaped in order to analyze patient-provider interactions. In the study presented here, we report only on the physical illness content that was mentioned in the videotapes of intake sessions and in postintake research interviews. Forty-seven clinicians participated in the study. Clinicians were from eight clinics in the Northeastern United States serving uninsured patients, working families, and recent immigrants. Clinicians included 18 social workers (38%), 13 psychiatrists (28%), 12 psychologists (26%), and three nurses (6%); 31 (66%) were female, and 33 (70%) had at least six years of experience. Twenty-five clinicians were white (53%), 17 were Latino (36%), four were black (9%), and one was Asian (2%).
Patients were told the study aimed to understand how patients and doctors arrive at a mental health diagnosis and to improve matching of services to patient needs. Patient exclusion criteria included psychosis, suicidality, or need for interpreter services. Patients were approached through their clinicians or directly by research interviewers. Two patients were evaluated for participation, but they lacked the capacity to consent and were therefore not enrolled. A total of 171 adults were invited to participate in the study; 42 declined. This yielded a total sample of 129 adults in mental health or substance abuse treatment; 64 were Latino (50%), 15 were black (12%), and 50 were non-Latino white (39%). Most patients were aged 18 to 49 years (N=102, 79%), were female (N=77, 60%), had completed high school (N=83, 64%), had a household income below $15,000 (N=81, 63%), and were not working (N=70, 54%). Institutional review boards at each clinic approved the study before data collection. Patients were evaluated as to whether they were capable of providing consent before the initial intake visit (
24 ). After a complete description of the study was given to the participants, written informed consent was obtained.
Procedures
Clinicians were recruited through clinic meetings. They were told the study aimed to learn about their experience with diagnostic interviews and improve matching of mental health services to patient needs. To minimize the influence of the research on interviews, we encouraged clinicians to interview as they normally would. Clinicians were limited to five intake visits each to ensure diversity of patient-provider interactions. Interviews were videotaped between March 2006 and March 2008, and the mean±SD intake duration of the intake sessions was 50.8±11.8 minutes.
Research assistants set up the videotaping of the intake session, but they were not present during the interview. All participants completed survey measures and completed semistructured postintake research interviews (in English or Spanish, as preferred) that were conducted by the researchers. Interviews that were conducted after the intake sessions were audiotaped and transcribed. Questions were asked in the postintake research interview that assessed perceptions of the presenting problem, therapeutic rapport, and the influence of sociocultural factors on patient help-seeking behavior or clinician treatment planning. Clinicians were also asked whether they reviewed medical records before intake. Interviewers were research assistants who were trained and supervised by the second author, a senior consultant in qualitative research.
Survey measures
Patients reported age, gender, race or ethnicity, employment, education, socioeconomic status, and physical health (from the 12-Item Short-Form Health Survey [SF-12] measure) (
25 ). Clinicians reported age, gender, race or ethnicity, socioeconomic status, discipline, and years in practice.
Information checklist
An information checklist was developed to analyze all videotaped evaluations. Items on the checklist included
DSM-IV criteria for axis I disorders, psychosocial variables, and 21 physical illnesses derived from the National Latino and Asian American Study interview (
26 ). The item "problems with physical health" captures nonspecific physical complaints, and the item "physical illness" captures mention of illness without specific diagnoses. Items were coded as either elicited by clinician or volunteered by patient, thereby capturing who first raised physical concerns in the intake session. If information on a given item was elicited or volunteered, the item was coded as "discussed." The items that were discussed were then summed. Items were coded as "endorsed" when patients disclosed having been diagnosed as having a given illness.
A team of seven clinicians were trained on the checklist and coded all the videotapes. Checklist data were available for only 120 intake sessions, because of poor video quality for eight sessions and the lack of assessment by a mental health counselor in one session. For the last videotape coded, overall agreement was 86%–87% and agreement for discussed items was 66%–73%. Demographic characteristics and information checklist frequencies were summarized with descriptive statistics (SAS, version 9.1). Differences in checklist frequencies by clinician discipline and patient ethnicity were determined by chi square test.
Qualitative analysis
A sample of 28 assessments of physical illness was selected for qualitative analysis to understand how clinicians structure discussions of physical problems. We included patients who endorsed more than three physical illnesses on the information checklist and who endorsed problems because of physical health at least "most of the time" on the SF-12 (
25 ). We included all black patients with axis III diagnoses because of the small sample. This approach yielded 13 women (46%) and 15 men (54%). Thirteen (46%) were white, nine (32%) were black, and six (21%) were Latino. The most common axis I diagnoses were anxiety, mood, and substance use disorders. Axis III disorders in the qualitative analysis were chronic pain (nine diagnoses), hepatitis C (seven diagnoses), hypertension (four diagnoses), sleep apnea (four diagnoses), asthma (three diagnoses), headaches (three diagnoses), and injury (three diagnoses). Clinicians were social workers in ten cases (36%), psychiatrists in nine (32%), psychologists in five (18%), and nurses in four (14%).
Any discussion of physical illness in the videotapes selected for qualitative analysis was transcribed by the first author. An initial group of 15 transcripts was read independently by the first and second authors, coded line by line, and compared. Close reading of these transcripts revealed categories and themes related to physical illness assessment, which were formalized in an NVivo 7 codebook (
27 ). [A table showing the codes used in qualitative analysis is available as an online supplement at
ps.psychiatryonline.org .]
Using this codebook, the same authors independently coded the 28 intake transcripts. We compared our separate codings, noted recurring themes, and used disagreements to revise the codebook. This helped the reliability of codes and moved the analysis toward saturation of common themes. Using this same codebook, we also coded the clinician and patient postintake interviews for each of the 28 intake visits. The postintake interviews presented an additional resource for understanding how clinicians and patients integrated physical problems into their planning and their experience of the intake, respectively.
Results
Total sample
In almost half of all intake visits, clinicians said they had access to (N=55 of 117, 47%) or reviewed (N=48 of 117, 41%) medical records before intake. At one site only, clinicians entered clinical data into computers during intake visits.
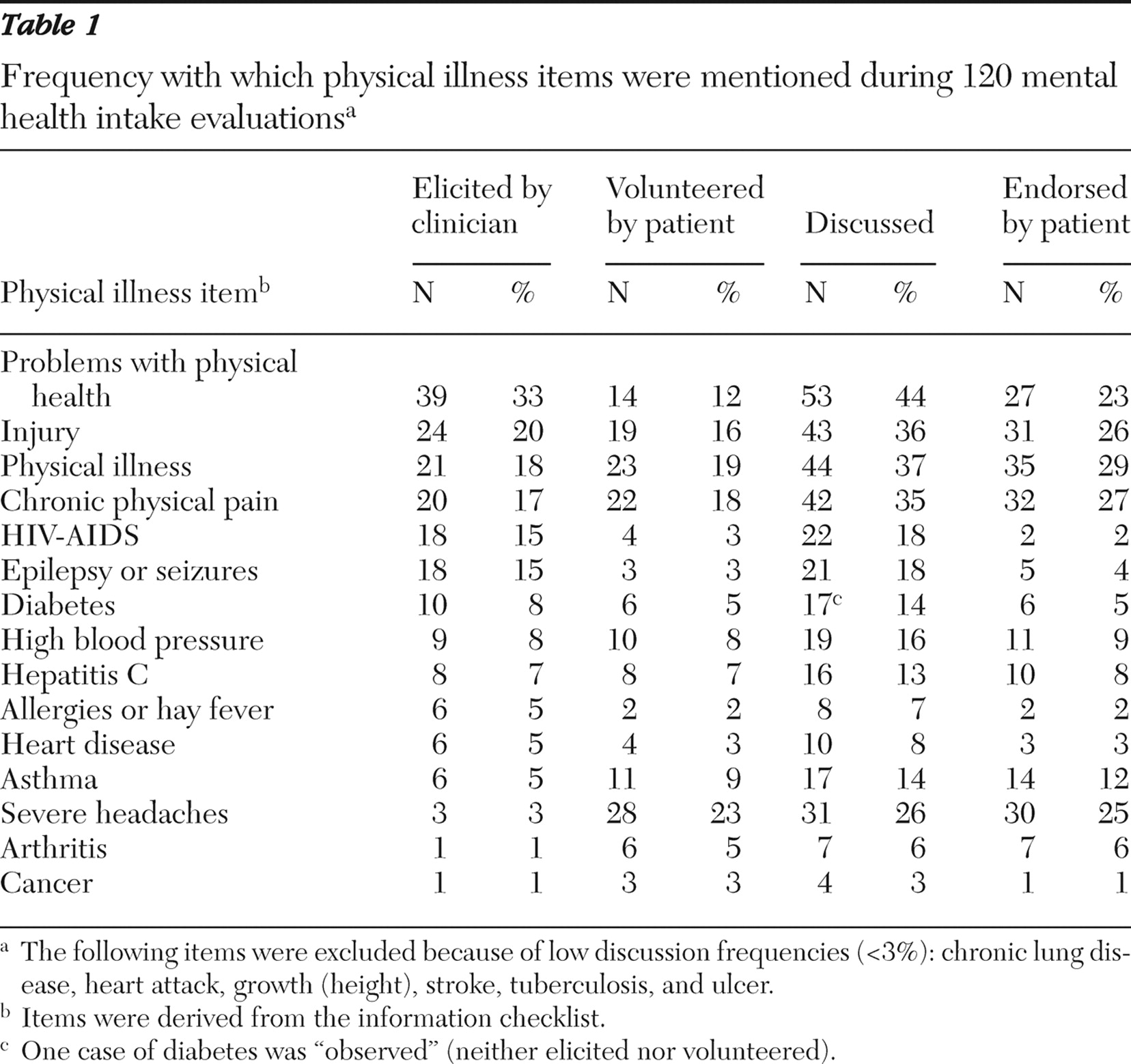
Table 1 summarizes information checklist frequencies for the total sample. Clinicians most often elicited the following five items: problems with physical health, injury, physical illness, chronic physical pain, and HIV-AIDS. Patients most frequently volunteered the items severe headaches, physical illness, and chronic physical pain, and they most commonly endorsed the items physical illness, chronic physical pain, injury, and severe headaches. The mean number of items discussed per intake was 3.0. Substantial discussions of physical health, in which three or more items were discussed, occurred in 67 intake visits (56%), while no items were discussed in 16 intake visits (13%). The frequencies of endorsed items and axis III diagnoses given by clinicians were similar (data not shown), suggesting the information checklist accurately reflects clinician diagnoses.
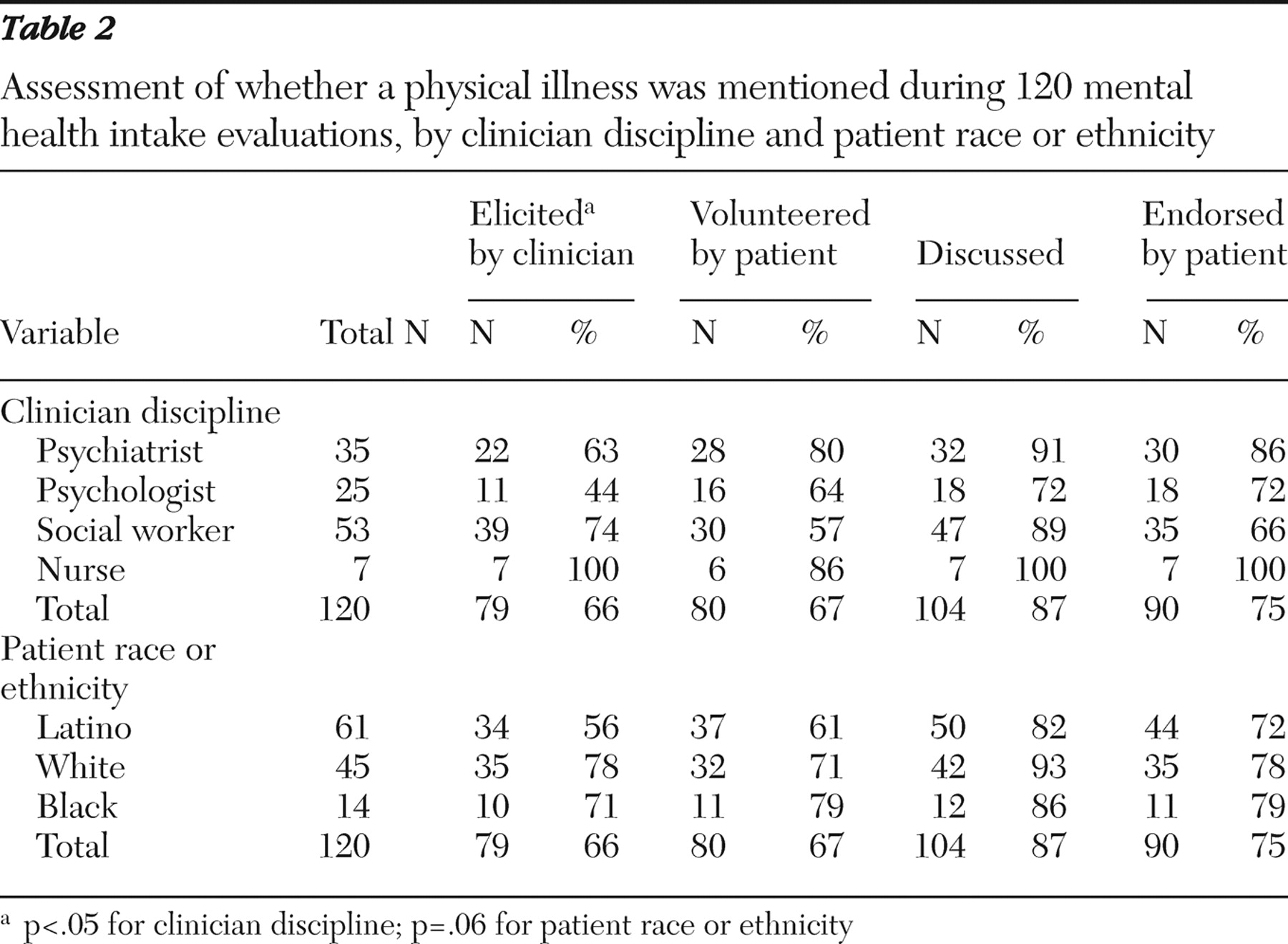
Table 2 shows overall differences for eliciting any physical illness item between the types of clinicians. At least one item was elicited by 100% of nurses, 74% of social workers, 63% of psychiatrists, and 44% of psychologists (p<.05). Paired comparisons suggest these differences were primarily between psychologists and nurses (p<.01) and psychiatrists and nurses (p=.05). There were also small differences in eliciting any physical illness item by patient race or ethnicity. At least one item was elicited among 78% of white patients, 71% of black patients, and 56% of Latino patients (p<.06). The only significantly different paired comparison was for elicited items among Latino patients and white patients (p<.05). The three patient groups volunteered and endorsed physical illness in similar proportions.
Qualitative analysis
No clinician completed a full formal review of organ systems. Rather, clinicians explored physical problems in relation to psychiatric complaints, as described below.
Formulating physical problems in the differential diagnosis
Twenty of the 28 cases in the qualitative analysis covered physical illnesses that could contribute to or exacerbate psychiatric illness, including cardiac disease, diabetes, hepatitis, HIV, obstructive sleep apnea, pain, and thyroid disease. Clinicians used this information in biopsychosocial formulations of the presenting psychiatric complaint. For example, in the postintake interview, a psychologist said, "She's dealing with a lot of different stressors like having HIV, her husband being incarcerated, and having to deal with [many] children by herself." This at times prompted changes in treatment recommendations (for example, dosage adjustments for liver disease).
Attentive clinicians used differential diagnosis in their formulations to assess the contribution of physical causes to psychiatric complaints. In the postintake interview, one psychiatrist commented that she wanted to "rule out general medical contributions to [a patient's] depression." She tried "a bit of psychoeducation … to tell him that sleep apnea can definitely cause many of the symptoms he was describing." Another psychiatrist, presented with a complaint of memory loss, said at the postintake interview, "You have to go through a whole tree of things that can cause memory loss." This "tree" included medical, psychiatric, and genetic history; memory testing; and review of medical records. The psychiatrist concluded, "He doesn't have a psychiatric problem. He's got a sleep problem, and he needs to go to a sleep lab and have a sleep study …. The psychiatric part of it was I had to rule out a bunch of typically neurological things."
Physical symptoms resulting from psychiatric treatment
Psychiatrists and nurses counseled patients about potential physical side effects of psychiatric medications. These warnings occurred in nine of 13 cases and focused on metabolic and neurological effects of antidepressants, antipsychotics, and stimulant medications. These clinicians used prior test results to calibrate risk of obesity, cardiac disease, liver toxicity, and neurological sequelae. For example, at the intake visit a psychiatrist said, "Because of your problem with your liver, this medication will probably last a little longer in you than it would in most people, so I'm recommending a pretty low dose."
Two psychiatrists referenced treatment guidelines in recommending an electrocardiogram before methylphenidate treatment and a lipid panel during antipsychotic treatment. Clinicians did not provide preventive medical services.
Confirming relationships with primary care providers
When confounding physical problems were identified, in 20 of 28 cases clinicians inquired about or encouraged referrals to primary care providers. Social workers encouraged referrals to primary care in eight of ten encounters. For example, at the postintake interview, a social worker said, "He doesn't have a PCP [primary care physician]. So, I took him downstairs personally to set up the appointment." At the postintake interview, a psychologist commented about checking on the record of a patient with HIV "to find out what her T cell count was and is she following up with meds."
Promoting physical health care
Clinicians attempted to increase patients' confidence in their ability to control physical symptoms and maintain function, which we characterized as encouraging physical health care (
28 ). In the intake session, a social worker told her patient, "It's good to see a doctor when you're healthy because if you get sick later on, the doctor already has data from when you were healthy … and I can tell you are very interested in taking care of yourself."
Clinicians promoted physical health care during the intake sessions by advocating safe practices. For example, a social worker said, "So, [do] you follow the typical protocol for cleaning a needle?" Some social workers encouraged laboratory testing relevant to psychiatric treatment. Comments by social workers that reflected this included, "Have you ever been tested for Hep C or HIV?" and "Have you gotten any recent liver values to see where you're at?" One clinician promoted his patient's overall health by noting, "You're doing yourself a favor by staying away from alcohol and drugs …. One day at a time and, you know, you put the pieces back together again."
Missed opportunities
In some intake visits, clinicians did not structure discussions around physical illness. Such histories were limited to a bare chronology of events. For example, one clinician asked, "When did you get treated for your liver?" In other cases, clinicians would simply neglect the physical complaint. A patient with obesity, sleep apnea, and poor concentration presented for gastric bypass evaluation. His clinician omitted the presurgical consultation and prescribed methylphenidate for presumed attention-deficit disorder.
There were missed opportunities for patient education in the intake sessions. One patient disclosed "a little tumor," hepatitis, and headaches. The clinician asked, "What do you take for headaches?" and was told, "With the liver thing, they don't want me to take nothing else but Tylenol." The clinician did not inquire further about the tumor, and the patient was not educated about potential problems with acetaminophen and liver disease.
Discussion
Physical health was raised in a majority of intake visits and discussed substantially in over half. These findings can be understood by examining to what extent each member of the patient-clinician dyad raised the issue. Patients volunteered physical problems frequently, particularly with psychiatrists and psychologists, who elicited them less often than nurses. Clinicians asked most about "problems with physical health," which could serve as a general invitation for detailed disclosure. Thus the results may reflect the time-honored tradition of "following the patient's lead." Psychologists and psychiatrists receive more psychodynamic training (
29 ) and may more readily employ such open-ended approaches to eliciting information about physical illness. These clinicians may therefore have waited for patient-initiated discussion of physical illnesses. The mental health clinician might best serve patients by using a more proactive assessment of physical problems during the intake. Clarifying these issues early in treatment may minimize the effect on the psychotherapeutic process.
Clinicians who do not inquire about physical illness may be missing it, at least until information is volunteered by the patient or discovered otherwise. Results from the parent study suggest that patients who are younger, Latino, or newer to psychiatric treatment volunteer less information (
30 ). Such patients may feel uncomfortable raising physical problems during mental health intake visits. This seems particularly relevant for Latino patients, who were less likely than other racial and ethnic groups in our study to elicit (p=.06) and volunteer (not significant) information on physical problems, despite comparable endorsement. Clinician-initiated discussions may thus uncover physical illness that might otherwise go unmentioned.
The illnesses endorsed by patients in this sample can negatively affect mental health (
5 ). Chronic pain and epilepsy increase the risk of suicide (
31,
32 ), as does asthma for depression, anxiety, and alcohol abuse (
33 ). Hypertension is a risk factor for dementia (
34 ). Both Hepatitis C and HIV and their treatments affect mood and cognition (
35,
36,
37 ). Obesity and diabetes are associated with second-generation antipsychotic treatment (
38 ). Our finding that clinicians often elicited the items HIV-AIDS and epilepsy or seizures, despite low patient endorsement, may reflect successful education efforts in these areas. Discussing more commonly endorsed items in intake sessions may be an effective and efficient use of mental health clinician time.
Qualitative analysis revealed how clinicians encourage exploration, planning, and coordination around physical illnesses. Medically trained clinicians integrated physical problems into differential diagnoses, formulations, and treatment recommendations. Although it is not recommended that psychologists and social workers diagnose or treat physical illnesses, these clinicians can review physical problems, encourage follow-up with primary care, and support patient efforts to maintain physical health. These efforts to structure the exchange of information and invite patient concerns seem appropriate and may improve continuity with primary care services.
Awareness of physical conditions that disproportionately affect psychiatric patients may facilitate prevention through appropriate referrals and support of patient self-care. These strategies reflect mechanisms of "trouble shooting" and "smoothing transitions" that Ware and colleagues (
39 ) have associated with maintaining continuity of care. Including more medical content in mental health curricula may require interdisciplinary collaborations in professional development. Psychiatrists score well on baseline knowledge of preventive medical services and are interested in providing such services, despite a relative lack of training (
40 ).
The clinics studied were all affiliated with primary care sites, which could raise the threshold for physical health assessments by mental health clinicians. Results should therefore not be taken as representative of nonurban settings. Rural mental health clinicians may indeed face a higher burden of responsibility for managing physical problems (
17 ). Also, patients with severe mental illness are known to have more serious physical health needs (
38,
41 ). Their exclusion may have lowered the physical illness burden of this sample. Finally, intake duration was not standardized in this naturalistic study. Shorter intake visits may have included less assessment of physical illness.
Conclusions
This study described the strategies used by mental health clinicians when assessing physical symptoms. Our results may support the efforts of mental health clinicians to discharge their responsibilities for the overall health of patients. Taken in the context of published recommendations, such as those available for psychiatrists (
17 ), our qualitative findings can further inform educational and policy efforts to improve quality of care for individuals with comorbid physical and mental disorders.
Acknowledgments and disclosures
This study was supported by grant 1P50 MH 073469, funded by the National Institute of Mental Health, and grant P60 MD 002261 (NCMHD), funded by the National Center for Minority Health and Health Disparities. The Patient Provider Encounter Study data used in this analysis were provided by the Advanced Center for Latino and Mental Health Systems Research of the Center for Multicultural Mental Health Research at the Cambridge Health Alliance.
The authors report no competing interests.