Ensuring access to needed health services is a public policy priority and a major objective for the U.S. Department of Veterans Affairs (VA) health system. Access is particularly important for patient subpopulations, such as individuals with bipolar disorder, who have complex ongoing treatment needs and are at increased risk of acute care episodes. Unfortunately, however, individuals with bipolar disorder are more likely than those without the disorder to report access barriers (
1,
2 ). For health systems, enhancing services delivery requires understanding patient access and utilization, including access to and receipt of services from out-of-system providers.
It is important to define access carefully. As discussed in McCarthy and Blow (
3 ), Donabedian and others have defined access as a general concept that refers to specific dimensions of the fit between characteristics of potential clients and providers. Penchansky and Thomas (
4 ) validated a taxonomy of these dimensions: affordability, availability, acceptability, accommodation, and geographic accessibility. However, analyses often consider access solely in terms of the affordability of services (for example, having insurance coverage). Access is not an all-or-nothing issue; individuals may differ in their degrees of access. Also, access should be understood at the individual's level and in relation to specific providers. However, few studies have examined the influence of multiple dimensions of access on receipt of services from out-of-system providers.
In response to access barriers, individuals may delay or forgo health service encounters. Studies have documented the impact of barriers on utilization measured in terms of contact with providers (receipt of any services), volume of services received, and continuity of care. Although contact indicates a level of access, individuals who receive some services may still experience access barriers (
3 ). For example, among VA patients with serious mental illnesses, access barriers are associated with having fewer outpatient encounters, less timely outpatient care after discharge, reduced likelihood of receiving mental health case management, and increased likelihood of long-term gaps in health system utilization (
5 ).
Another response to access barriers is to seek services from other providers, including out-of-system providers. However, cross-system services use may complicate provider efforts to ensure continuity and coordination of care and health system quality assessments (
6,
7 ). Research examining out-of-system utilization in relation to measures of access for health system and out-of-system providers may advance our understanding of utilization dynamics and inform efforts to enhance treatment retention and continuity of care.
There is a growing literature regarding out-of-system utilization among veterans who receive VA health services, and some studies have included access-related measures. For example, among respondents to a large national 1999 VA survey, 49% of veterans who reported having received VA services in the prior year also reported having received services from non-VA providers, and reliance on VA services was more common among veterans who did not have health care coverage outside the VA benefits (
7 ). Similar associations with measures of the affordability of non-VA services have been observed among VA primary care patients (
8 ). Satisfaction with VA care, which relates to the acceptability of VA care, is negatively associated with out-of-system utilization (
8,
9 ), and measures of the geographic accessibility of VA and of Medicare providers are associated with dual-system utilization, with some substitution of services across systems where accessibility is limited (
10 ). These findings suggest that system-specific health services utilization is influenced by access to both within-system and out-of-system providers.
However, most studies have focused on dual-system utilization only among VA patients who are eligible for Medicare on the basis of their age. In order to advance a comprehensive assessment of health care access and utilization, it is important to consider the entirety of non-VA services utilization among patients of all ages, to include multiple measures relating to access to VA and non-VA services, and to consider individuals' experiences related to access.
This study examined associations between access-related measures and out-of-system utilization among veterans receiving treatment for bipolar disorder at a VA medical center. Consistent with theory and prior research, we hypothesized that out-of-system utilization is more likely when there are fewer barriers to out-of-system services and when there are more barriers to within-system services.
Methods
We examined survey response data from participants in the Continuous Improvement for Veterans in Care—Mood Disorders study (
11 ), which assessed quality of care among patients with bipolar disorder who were receiving mental health services at an urban VA medical center in western Pennsylvania. This medical center had no shortage of mental health providers, and there were multiple out-of-system providers in the area. Between July 2004 and July 2006, individuals were recruited into the study, and written informed consent was obtained after they received a complete description of the study. The study excluded 14% of eligible patients (104 out of 720) because of acute psychiatric symptoms that precluded informed consent. Of the remaining 616 patients approached for the study, 148 refused, primarily because they lacked time to complete the survey before their outpatient appointment. A total of 468 patients enrolled in the study, and 435 (93%) completed the survey. Forty-four respondents (10%) were excluded because of incomplete data, leaving an analytic sample of 391. Among the 435 survey respondents, excluded patients did not differ significantly from retained patients on any of the study measures.
The main outcome measure was self-reported non-VA health services utilization. This was assessed as the total number of reported nonemergency encounters with non-VA providers in the prior 12 months, including both outpatient visits and hospitalizations. These could include encounters for mental health or non-mental health treatment.
Independent variables included the following access-related measures: indicators of having Medicare, Medicaid, or private insurance coverage; of having military service-connected disability status; of residence more than 50 miles from the nearest VA hospital; of whether the individual drives to VA appointments; and a summary measure of mental health access, assessed by the question "During the last six months, did you ever need mental health care but could not get it?" Service connection indicates whether a veteran has been certified as disabled as a result of disorders incurred during military service. Many VA patients with bipolar disorder have service-connected disabilities and receive financial compensation and have priority eligibility for VA health services.
Also included were indicators of patient age, gender, race-ethnicity, marital status, homelessness in the prior four weeks, employment status, and mental and physical health status. Health status was assessed with scores from the mental and physical component summaries (MCS-12 and PCS-12, respectively) of the 12-Item Short Form Health Survey of the Medical Outcomes Study (SF-12), an abridged version of the SF-36. Summary scores can range from 0 to 100, with lower scores indicating poorer functioning, and they are normalized so that scores of 50±10 represent the mean±SD in the general population. The PCS-12 includes indicators of physical functioning, role limitations from physical problems, bodily pain, and general medical health. The MCS-12 consists of measures of vitality, social functioning, role limitations from emotional problems, and mental health.
We calculated descriptive statistics examining respondent characteristics overall and by out-of-system health services utilization status (having had any versus none). Using multivariable Tobit analysis of the latent variable "propensity to use non-VA services" (left-truncated for individuals who had not used services outside the VA), we assessed whether access-related measures were associated with non-VA services use. Tobit analysis enabled simultaneous examination of the decision to seek any non-VA services and the amount of non-VA services received.
All study analyses were completed with SAS, version 9.1. The study was approved by the institutional review board at the Pittsburgh VA medical center.
Results
Of the 391 study participants, 218 (56%) reported having received non-VA health services in the prior year. The 391 study participants included 334 men (85%) and 269 (69%) individuals who were unmarried. Ages ranged from 21 to 78 years (mean=49.0±10.7). Forty-four (11%) participants reported having experienced homelessness in the prior four weeks, 160 (41%) had service-connected disability status, 64 (16%) lived more than 50 miles from a VA hospital, 91 (23%) had Medicare coverage, 23 (6%) had Medicaid coverage, 89 (23%) had other insurance coverage, 108 (28%) were employed, and 196 (50%) drove themselves to VA appointments. The mean PCS-12 score was 37.9±7.6, and the mean MCS-12 score was 31.6±7.6, indicating poor functioning. Seventy participants (18%) reported having been unable to receive needed mental health care.
Among the 218 patients who reported non-VA services utilization, the mean number of non-VA encounters was 15.0±25.6, with most being outpatient visits (4.1±11.5 visits with non-VA mental health providers, 4.5±6.9 with non-VA doctors other than mental health providers, and 5.5±14.1 for counseling). On average, patients reported .5±1.4 non-VA hospitalizations for mental health problems and .4±1.0 non-VA hospitalizations for general medical problems.
Compared with the 173 individuals with no out-of-system utilization, the 218 individuals who reported non-VA services use were younger (mean age 48.1±10.9 versus 50.3±10.2; p<.05), more likely to be married (80 of 218, or 37%, versus 42 of 173, or 24%; p<.01), and more likely to report recent homelessness (31 of 218, or 14%, versus 13 of 173, or 8%; p<.05), Medicaid coverage (18 of 218, or 8%, versus five of 173, or 3%; p<.05), other non-Medicare health insurance coverage (72 of 218, or 33%, versus 17 of 173, or 10%; p<.001), and being employed (69 of 218, or 32%, versus 39 of 173, or 23%; p<.05). They were also more likely to report problems accessing mental health services (47 of 218, or 22%, versus 23 of 173, or 13%; p<.05).
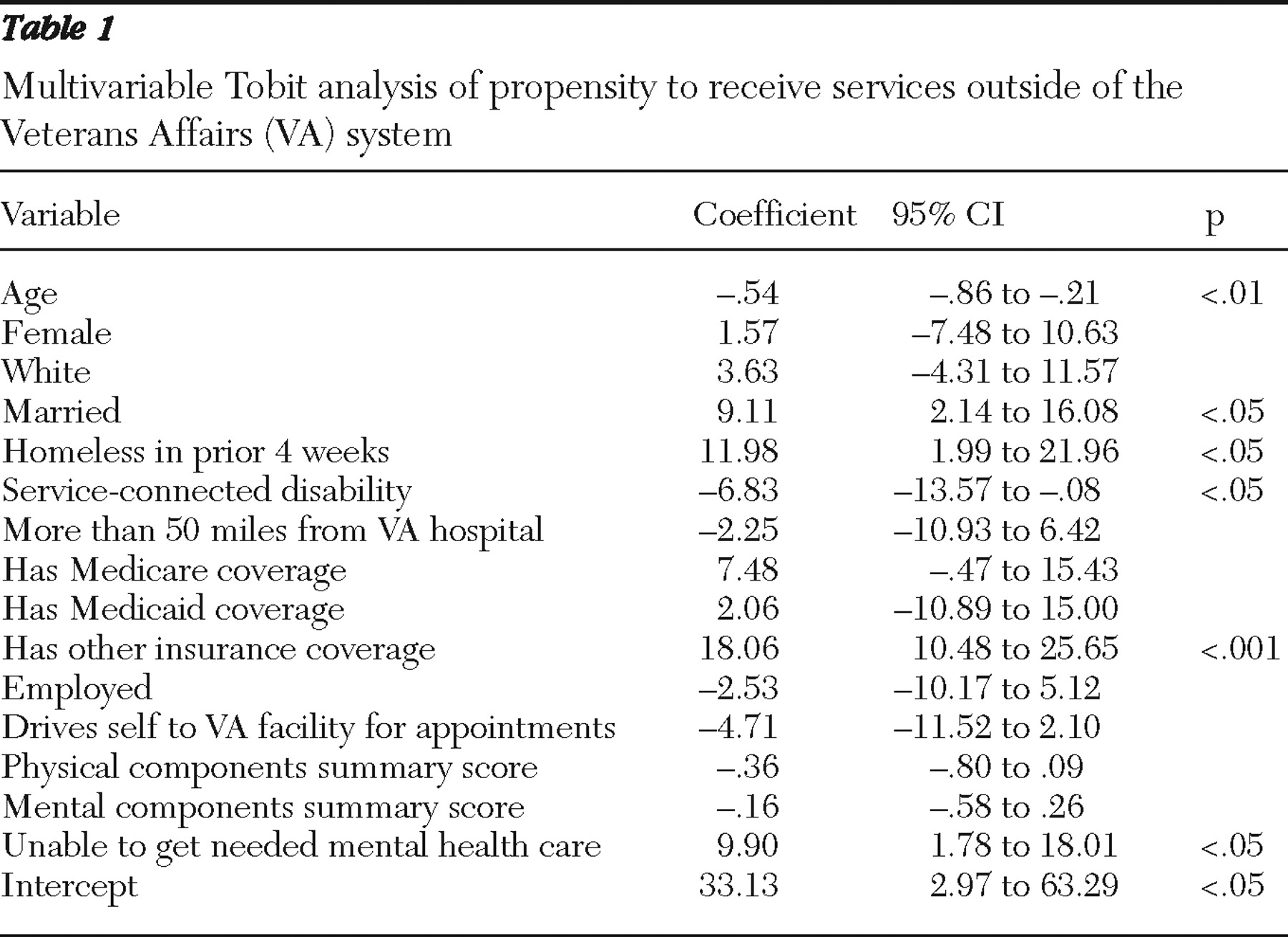
In multivariable Tobit analyses (
Table 1 ), individuals had a greater propensity to receive health services from out-of-system providers if they had other insurance coverage, if they did not have VA service-connected disabilities, or if they reported having been unable to receive needed mental health services in the prior six months. Being younger, married, or homeless was each positively associated with non-VA use (p<.05). Proximity of VA care, having Medicare and Medicaid coverage, employment and driving status, and PCS-12 and MCS-12 scores were not significant predictors of receipt of non-VA system services.
Discussion
Out-of-system utilization by VA patients with serious mental illness has been regarded as relatively uncommon (
12 ), based largely on research conducted in the early and mid-1990s (
13 ). For example, during the years 1988 to 1993, 16%–17% of VA patients in Philadelphia with behavioral health issues received services from non-VA providers (
14 ). More recent national survey data indicate substantial out-of-system services utilization among patients with bipolar disorder (49%), considerably more than among patients with schizophrenia (38%) (
2 ). In our study of patients with bipolar disorder, out-of-system utilization was also common, with 218 of 391 (56%) participants reporting non-VA services utilization in the prior year for general medical or mental health reasons. However, findings may not be typical of all VA patients with bipolar disorder, in that participants were identified from a single VA medical center and it was not possible to include individuals with acute psychiatric symptoms that precluded informed consent.
A strength of this local study was its inclusion of a range of important measures, including multiple measures related to access. These included indicators of the affordability of VA and non-VA health services (service-connected disability status and measures of non-VA health coverage, respectively), of the geographic accessibility of VA providers, and a summary indicator of mental health access—whether patients had been unable to receive needed mental health services.
Study findings demonstrate the importance of understanding access at the person-provider level by documenting associations between patients' access to VA and non-VA providers and their out-of-system services utilization. Out-of-system utilization was more likely among patients with private insurance coverage and less likely when patients had VA priority eligibility status (having service-connected disabilities). Also, it was more likely for patients who reported having recently been unable to receive needed mental health services, which suggests that individuals who experience access problems are more likely to seek services from alternative providers.
It is noteworthy that use of non-VA services was not associated with Medicare or Medicaid coverage, whereas private insurance coverage was a significant predictor of out-of-system utilization. This may reflect provider reluctance to treat patients with Medicaid and Medicare coverage, because these programs may reimburse providers at lower levels than private insurance sources. Other dimensions of access may also affect choice of non-VA providers. Differences in the perceived quality of care from Medicare and Medicaid providers may affect the acceptability of services for individuals. Private insurance providers may be more likely to market their services to enrollees, influencing treatment-seeking behavior. And having private insurance coverage may itself reflect patient preferences for receiving non-VA health services.
Neither the proximity of VA medical centers nor the mode of travel to VA appointments was associated with out-of-system utilization. This is not entirely surprising. The impact of geographic accessibility barriers on health system utilization among active patients is typically small, requiring large samples to ascertain (
3,
10 ). In the analysis we did not find evidence that the geographic accessibility of VA providers influenced out-of-system utilization among patients who had contact with VA providers.
Several patient factors were associated with non-VA utilization. Being married was associated with greater likelihood of receiving non-VA health services. Individuals who are married may be more likely to have non-VA health coverage and may have greater familiarity with non-VA providers. Being younger was associated with greater non-VA utilization, which may reflect cohort differences in preferences for services utilization. Also, participants who experienced homelessness in the four weeks before the survey were more likely to report out-of-system utilization. This finding may reflect greater need for urgent care services, greater residential mobility, and less established relationships with VA providers.
Although in bivariate analyses being employed was associated with greater likelihood of reporting out-of-system service use, in the multivariable analysis employment status was not a significant predictor. This may reflect the importance of private insurance coverage in the model. Out-of-system use was also not associated with gender, race-ethnicity, or physical and mental health status.
Health systems should strive to reduce access barriers that may cause patients to seek services from out-of-system providers, potentially disrupting care coordination for patients with complex chronic illnesses. Continuing efforts are needed to enhance access for individuals with bipolar disorder and to better understand the impact of out-of-system utilization on overall and health-system-specific quality of care.
Analysis of local survey data offers a useful avenue for understanding out-of-system utilization. Future studies should include measures of additional dimensions of access, and measures should be specific to health system and out-of-system providers. These could include, for example, indicators of the perceived acceptability of VA and of out-of-system providers, including the perceived quality of these services. It is important to consider system-specific measures of experiences of having been unable to receive needed services. Further, it is important to consider in- and out-of-system services utilization for specific services and in association with system-specific measures of quality. Finally, we note that the existing literature on cross-system utilization is based largely on VA patients, and future research should examine these issues in the context of other health delivery systems.
Conclusions
Out-of-system service utilization was common among study participants with bipolar disorder. Access to VA and non-VA providers affected out-of-system utilization, with greater non-VA use among individuals with private insurance coverage and less non-VA use among individuals with VA service-connected disability status. There was support for the idea that experience with mental health access barriers is associated with increased cross-system utilization. Poor mental health access may cause individuals to seek care from alternative providers, which may complicate continuity of care (
6 ). When possible, future studies of health system access and quality should include indicators regarding out-of-system services utilization.
Acknowledgments and disclosures
This study was supported by VA grant IIR 02-283.
The authors report no competing interests.