In the past 30 years, efforts have been made to improve access to care in the general practice setting for patients with common mental disorders (
1 ), to improve treatment in this setting, and to elucidate indications for referral of patients with common mental disorder to mental health care (
2 ). Clustering of common mental disorders and somatic disorders might influence access to mental health care for common mental disorders. Comorbidity has been defined by Feinstein (
3 ) as any other clinical entity that exists or occurs among patients during the clinical course of the index illness under study. In terms of the filter model of Goldberg and Huxley (
4 ), a comorbid somatic disorder might be a factor influencing the several filters for diagnosis and treatment of depression, anxiety disorders, or substance use disorders and thus may play a role in a patient's transitioning from general practice care to mental health care.
Clustering of mental and somatic disorders has been established among patients with depressive disorder, anxiety disorder, and alcohol dependence (
5,
6,
7 ). This can be an illness-specific association, but it might be a more generic factor. The presence of a comorbid somatic disorder may distract physicians from recognizing and treating depressive disorder (
8,
9 )—for example, among patients with fatigue and a somatic disorder, a physician may attribute the fatigue to the somatic disorder and not examine whether the patient has comorbid depression. This so-called attribution bias might lead to underdiagnosis and undertreatment of the depressive disorder (
10 ).
Also, attitude has been found to be an important barrier to mental health service utilization—for example, patients with comorbid depression and a somatic disease may assume along with their physicians that the symptoms are due to the somatic disease, not to the depression, and that symptoms will resolve once the somatic disease is treated (
11,
12 ).
In the Netherlands, the primary care setting is the original point of service entry. A patient cannot go to a mental health practitioner without referral by the primary care provider. Primary care physicians are gatekeepers for the secondary care tier, for mental health care and somatic health care (
1 ). In the Netherlands, common mental disorders can be treated in the primary care setting by psychologists, who provide short-term treatment, or by the primary care physician, who can consult a psychiatrist for advice (
13,
14 ). In the case of a chronic mental disorder, patients can be referred by the primary care provider to a specialist mental health treatment setting, where they will receive treatment from a psychiatrist or from a multidisciplinary team (
2 ). This referral requires recognition of the need for referral by the primary care provider. In other words, we might expect that mental disorders occurring with somatic disorder are less likely to be detected, because the focus of attention will be directed toward the somatic disorder and because symptoms of mental disorders, such as fatigue, may be attributed to the somatic disorder. Main factors affecting use of both mental health and primary care mental health services are therefore presentation of symptoms by the patient and recognition by the primary care physician.
However, evidence of the contrary is available as well (
15 ); mental illness is often severe and persistent, and therefore it might be more likely to be detected in the case of comorbid medical illness because of frequent attendance of the practice. Therefore, in this regard, we have conflicting hypotheses, and the aim of this study was to evaluate which one is true.
This study explored mental health care utilization patterns among patients with comorbid somatic disorders that occur in common mental disorders (mood disorder, anxiety disorder, or substance use disorder) and compared them to those of patients with the common mental disorder but no comorbid somatic disorder. The study examined whether patients with common mental disorders with comorbid somatic disorder are more or less likely to use mental health care in the primary or specialty care setting than those with common mental disorders alone. Our aim was to identify referral patterns in subgroups of patients with mental disorders whose comorbid somatic conditions may make detection of mental disorders by their primary care providers more or less likely. As a result, comorbidity clusters may be identified that need enhanced recognition and treatment strategies. The study specifically evaluated clusters involving pain symptoms, rheumatoid arthritis, or digestive disorders, because a relationship between those and depressive or anxiety disorders has been established in earlier studies (
16,
17,
18 ).
This study analyzed data from the large-scale Netherlands Mental Health Survey and Incidence Study (NEMESIS), with a focus on mood disorders, anxiety disorders, and substance use disorders.
Methods
A summary of the methods is provided below. [An extensive description of the methods is available as an online supplement at
ps.psychiatryonline.org .]
NEMESIS was a psychiatric epidemiologic study conducted in 1996 of a representative sample of 7,076 adults aged 18–64 years. We used data from the first wave of the NEMESIS (
19 ). NEMESIS used the Composite International Diagnostic Interview (CIDI) to identify psychiatric disorders present at any time in the 12 months before the interview.
In NEMESIS, a total of 1,613 persons had a mental disorder. A total of 1,601 persons had common mental disorders at any point within the 12 months preceding the interview: 573 had a mood disorder, 912 had an anxiety disorder, and 533 had a substance use disorder. These categories of mental disorders were not exclusive: 1,234 had only one disorder, 317 had two disorders, and 50 had all three disorders. An additional 12 persons had another mental disorder (schizophrenia or eating disorder). Our sample focused on the 1,601 persons with the common mental disorders. The dependent variable, use of care for emotional or addiction problems, was defined as the use of mental health care in the primary care setting or use of specialty mental health care.
We considered three potential predictors of use of mental health care. First, we determined whether any of the 1,601 persons with mood, anxiety, or substance use disorders used mental health care in either setting—general practice or specialized care. The second predictor examined was the presence of one or more self-reported comorbid somatic conditions from a list of 31 chronic somatic disorders divided over nine somatic classes: asthma and emphysema, arthritis and rheumatoid arthritis, cardiovascular disease, digestive disease, sensory impairment, diabetes, chronic cystitis, thyroid gland disease, and other (
www.cbs.nl/en/figures/statline/index.htm ). The third predictor examined was the comorbid presence of a selection of the five most frequent somatic disorders in the total NEMESIS sample. In our analyses, we included only persons who indicated that they had received treatment or medication from a physician for a comorbid somatic disorder.
We performed bivariate and multivariate multinomial logistic regression analyses to investigate whether comorbidity (here defined as the presence of an index mental disorder and a concomitant chronic somatic disorder) was associated with use of mental health services in either setting. These analyses compared the two categories of service users (those using general practice care only and those using specialized mental health care regardless of whether they used general practice care) with the respondents reporting no use of either type of care for mental health problems in the past 12 months. First we looked at use of mental health care broadly, by the presence of any of the 31 somatic conditions in the groups with the three common mental disorders, and second, we looked at it more narrowly by the presence of any of the five somatic conditions. For all analyses, adjusted relative risk ratios (RRRs) were used to determine whether persons with the comorbid somatic disorder were more likely to use mental health care than those without the somatic disorder. We also determined whether there was a significant difference in the likelihood of mental health care use in either setting. We also performed separate analyses to determine whether the presence of other common mental disorders affected the results of the index mental disorder (results not tabulated).
Results
A general description of the NEMESIS sample has been previously reported (
20 ). In the sample of persons with the three common mental disorders (N=1,601), 807 (50%) had at least one of the 31 somatic disorders and 794 (50%) had none of the 31 somatic disorders. The five most common medical disorders in the entire sample were rheumatoid arthritis or arthritis, chronic backache, hypertension, chronic obstructive pulmonary disease, and inflammatory bowel disease or irritable bowel syndrome. In the sample with any of the common mental disorders (N=1,601), 163 (9%) had rheumatoid arthritis or arthritis, 184 (11%) had chronic backache, 147 (8%) had hypertension, 121 (8%) had chronic obstructive pulmonary disease, and 98 (6%) had inflammatory bowel disease or irritable bowel syndrome. An additional 287 (18%) had another somatic disorder. In our sample of persons with a common mental disorder (N=1,601), 529 (31%) received mental health care: 274 (16%) received mental health care in the primary care setting, and 255 (15%) received it in the specialty care setting. (Percentages are weighted throughout.)
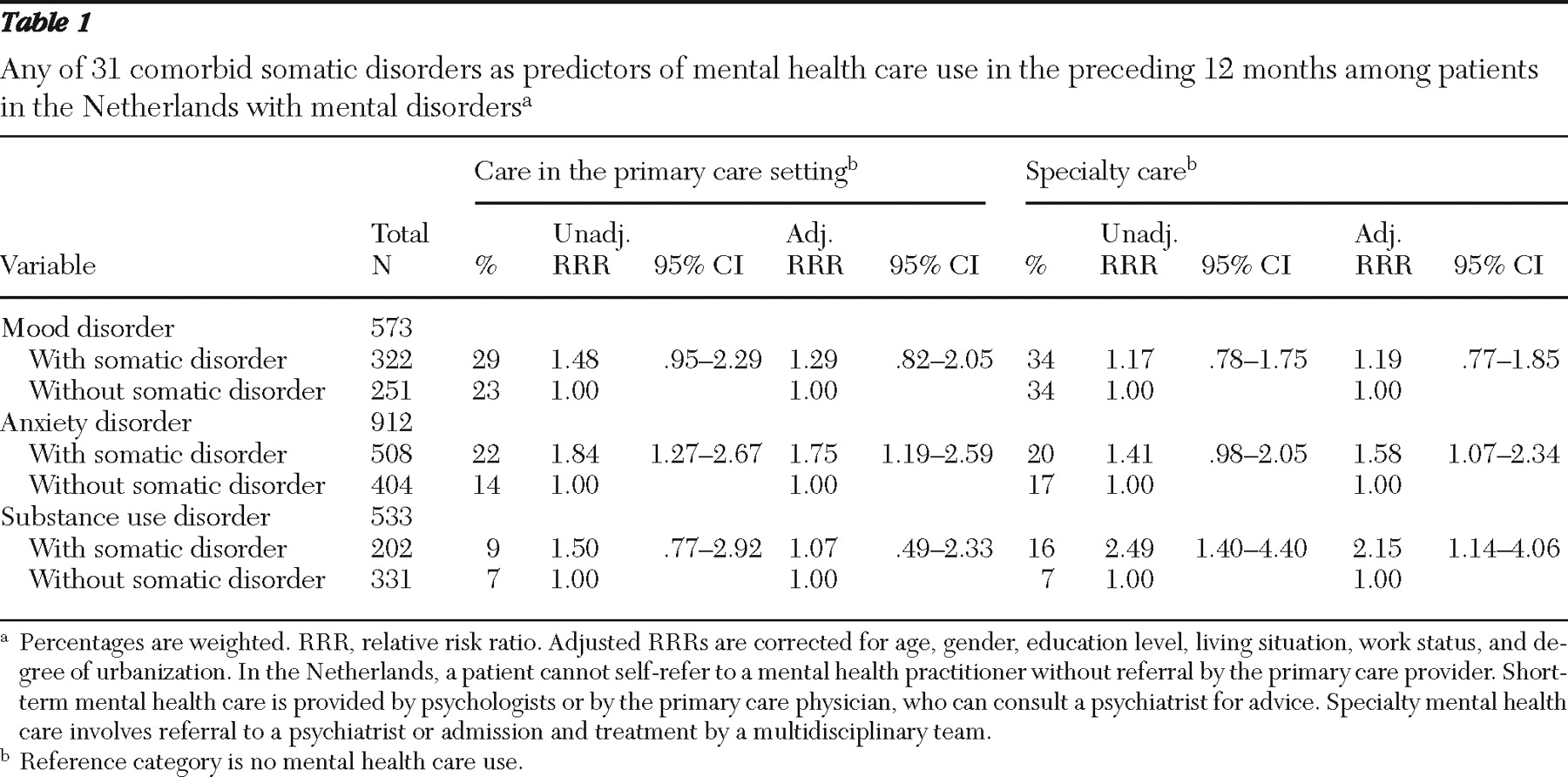
Analysis of 31 somatic conditions
Table 1 shows the analysis for the presence of any of the 31 comorbid somatic conditions. Among persons with mood disorders, those with a somatic condition were not significantly more likely than those without a comorbid condition to receive either type of mental health care. Among persons with anxiety disorders, the occurrence of a comorbid somatic disorder significantly increased the likelihood of mental health care use in the primary care setting (adjusted RRR=1.75) and use of specialty mental health care (adjusted RRR=1.58). In this group there was no significant difference in likelihood of mental health care use in either setting. Among persons with substance use disorders, the occurrence of a comorbid somatic disorder significantly increased the likelihood of specialty health care (adjusted RRR=2.15). No differences were found when these analyses controlled for the presence of common mental disorders other than the index common mental disorder (data not shown).
Among the 533 persons with a substance use disorder, 459 (86%) abused or were dependent on alcohol, 42 (7%) had a drug use disorder, and 32 (7%) had both an alcohol and a drug use disorder. Therefore, it can be assumed that our findings for the substance disorder group mainly reflect findings for persons with alcohol use disorders.
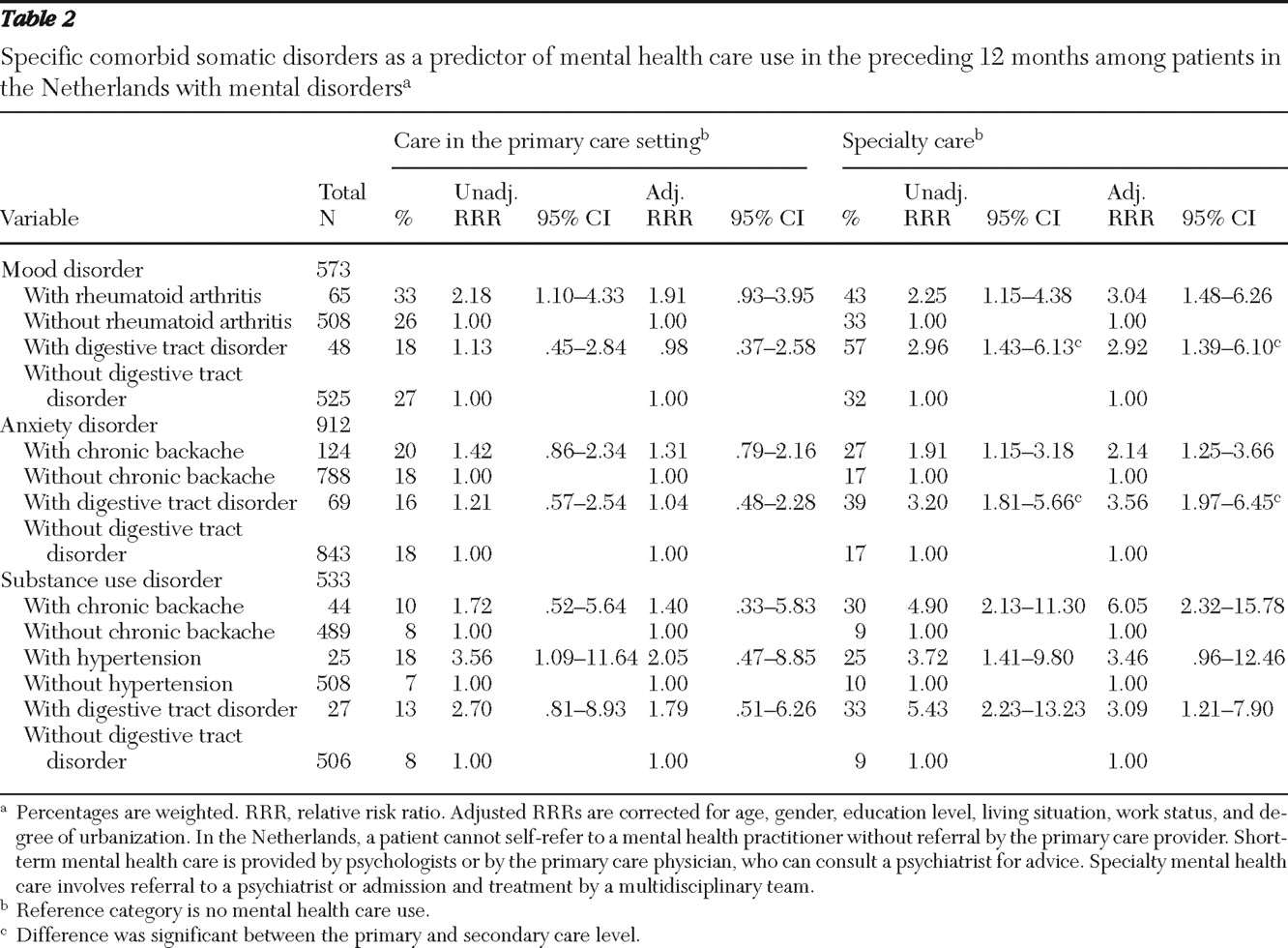
Analysis of five somatic conditions
Table 2 shows the likelihood of mental health care use in the past 12 months in either setting among persons in the three mental disorder groups by whether or not they also had one of the five somatic conditions noted above. Only significant findings are shown. In the group with mood disorders, the likelihood of use of specialty mental health care was three times as high among persons with comorbid rheumatoid arthritis (adjusted RRR=3.04) and among persons with a comorbid digestive disorder (adjusted RRR=2.92), compared with those who did not have these somatic disorders. Patients with mood disorders who had comorbid digestive disorder were significantly more likely to enter specialty care than to receive mental health care in the primary care sector.
Among persons with anxiety disorders, use of mental health care was significantly higher only among those with two of the comorbid somatic conditions. Those who had comorbid chronic backache were more than twice as likely as those without this comorbid condition to use specialty care (adjusted RRR=2.14), and those with an anxiety disorder who had comorbid digestive disorder were more than three times as likely as those without this comorbid condition to use specialty care (adjusted RRR=3.56). In addition, those with comorbid digestive disorder were significantly more likely to enter mental health care in the specialty setting than in the primary care setting.
Comorbid chronic backache also increased the likelihood of mental health care use among persons with a substance use disorder. Persons with a substance use disorder who had comorbid chronic backache were six times as likely to use specialty care (adjusted RRR=6.05) as those without this comorbid condition. In addition, among persons with a substance use disorder, those with comorbid digestive disorder were significantly more likely to use specialty care (adjusted RRR=3.09) than those without this somatic condition.
The fifth most common comorbid somatic condition—chronic obstructive pulmonary disease—was not associated with a significantly greater likelihood of mental health care in either setting for any of the three common mental disorders.
We later checked which type of digestive tract disorders were comorbid with the common mental disorders. We found that irritable bowel syndrome was present among persons with mood and anxiety disorders and that irritable bowel syndrome and inflammatory bowel disease were present among persons with substance use disorder (the majority of whom had an alcohol use disorder).
Discussion
In this study, only a minority of individuals with CIDI diagnoses of common mental disorders received any treatment. This may indicate undertreatment of mental disorders that has also been reported in a cross-national European survey, the European Study of the Epidemiology of Mental Disorders (ESEMed) (
21 ). That survey reported that only about one in five participants with a mental disorder had consulted the health services in the prior year.
When the presence of any of 31 comorbid somatic disorders was examined, a comorbid somatic disorder did not significantly predict use of mental health care among persons with mood disorders, whereas the likelihood of mental health care use was increased among persons with anxiety disorders and substance use disorders. Therefore, in mood disorders with poor somatic health in general, our hypothesis that recognition and treatment might be hindered by attribution bias seems to have been confirmed. The relative lack of referral and treatment among those with mood disorders indicates that measures aimed at improving recognition of depressive disorders might be needed among those who have comorbid somatic disorders. Because the combination of depression and a comorbid somatic disorder is associated with worse outcomes than either condition alone, it is important to enhance recognition of depression in clinical and primary care settings.
Among persons with anxiety disorders and substance abuse or dependence, those with any of the 31 comorbid somatic conditions had a higher likelihood of receiving mental health care in the specialty mental health setting. Therefore, for persons with these mental disorders our hypothesis that recognition and treatment would be enhanced by the comorbidity was confirmed. The higher likelihood may be due to more serious symptoms as a result of the comorbidity or to more frequent medical visits and consequently a higher chance of recognition of the mental disorder by the general practitioner and a higher chance of referral to specialty mental health care. Among persons with anxiety disorders, more frequent attendance may be due to increased activation and vigilance, resulting in health anxiety of the patient.
Among patients with comorbid rheumatoid arthritis or arthritis, chronic backache, or digestive tract disorder, the higher likelihood of mental health care use might reflect that the knowledge base for evidence-based treatment of these comorbid conditions is quite extensive. Cochrane reviews exist for comorbid anxiety and depression in rheumatoid arthritis (
22 ) and for treatment of irritable bowel syndrome with a partial 5HT-4 agonist (
23 ) and selective serotonin reuptake inhibitors (
24 ). Several studies also found antidepressants to be effective, with or without additional cognitive-behavioral therapy, in comorbid depression and rheumatoid arthritis (
25,
26 ). Recently, the effectiveness of several treatment modalities has been evaluated with some positive results, such as a treatment model for cognitive-behavioral therapy for comorbid irritable bowel syndrome (
27 ).
Patterns of recognition may be enhanced as well by the existence of a knowledge base. Among persons with anxiety disorders, those with comorbid chronic backache were more than twice as likely (adjusted RRR=2.14) to obtain mental health care. In the
DSM-IV (
28 ), as well as in the Dutch general practice standard for anxiety disorders (
29 ), musculoskeletal pain is one of the symptoms in generalized anxiety disorder. This symptom pattern may therefore result in higher levels of referral to mental health care because such pain might be recognized as a symptom of generalized anxiety disorder and might cause sufficient dysfunction to warrant referral.
Persons with substance dependence or abuse (the majority of whom had an alcohol use disorder) who had a comorbid digestive tract disorder were three times as likely (adjusted RRR=3.09) to use mental health care. These digestive tract problems occur frequently as complications of alcohol abuse or dependence. Alcohol abuse or dependence can go unnoticed for a long time and thus be underdiagnosed; however, co-occurrence with inflammatory bowel disease is a well-known example of comorbidity, which increases the need and likelihood of referral. A similar pattern was found among persons with substance dependence or abuse with comorbid chronic backache. Our study found that this group was six times as likely (adjusted RRR=6.05) to receive mental health care. Backache among persons with substance abuse is an alarm for serious medical complications of alcoholism—for example, pancreatic disease. We also found a weak association with substance use disorder in combination with hypertension (which is known to be a symptom of alcohol dependence). In the unadjusted analyses, our study found that among persons with a substance use disorder, persons with hypertension were more likely than those without hypertension to receive mental health care at the primary care level and at the specialty care setting. However, results did not remain significant when the multivariate analysis adjusted for several variables (
Table 2 ).
The fact that no association was found between use of mental health care and comorbid chronic obstructive pulmonary disease might reflect a problem of recognition of the mental disorder. Anxiety and depressive disorders have been shown to be highly prevalent but with an extremely low level of recognition (
30 ). Putman-Casdorph and McCrone (
30 ) stated that there are serious barriers to recognition and treatment of anxiety and depression when they co-occur with chronic obstructive pulmonary disease. Improvement of the knowledge base for recognition and treatment of comorbid anxiety and depressive disorders in chronic obstructive pulmonary disease is a point that warrants attention.
Another important aspect of the findings is that nearly all of the elevated use of mental health services associated with specific types of medical problems was seen in the specialty care setting. General practitioners may find it difficult to treat mental health problems or disorders when they co-occur with medical conditions. This is a highly relevant finding in the Netherlands, because of the country's ongoing discussion concerning whether patients with general medical and mental comorbidity should be treated in the primary care setting or should receive specialty care (
31 ).
In other words, this may be an illustration of the treatment and referral filter of the model of access to mental health care described by Goldberg and Huxley (
4 ). Treatment and referral may be influenced by knowledge concerning diagnosis as well as effective treatment modes in the comorbid conditions examined here. Also, aspects of organization of care might play a role in the referral patterns found in this study.
The study presented here has important advantages over other studies. Until recently, research in this field focused exclusively on the association between comorbid somatic disorders and depression. Our study had a much broader scope, because it focused on mood disorders, anxiety disorders, and substance use disorders. Also, a valid and reliable instrument (CIDI) was used to measure DSM-III-R axis I psychiatric disorders.
Limitations of this study are the ascertainment of comorbid somatic disorders by self-report, although in the statistical analyses we included only persons who indicated that they had received treatment or medication from a physician for a comorbid somatic disorder. Furthermore, we did not evaluate factors related to the general practitioners and the mental health care professionals who provided care in the primary care setting that might have influenced allocation of care or referral, because this was a sample from the general population. Therefore, we do not know what factors facilitated or inhibited referral to mental health care of patients with comorbidity. We also did not measure severity of the symptoms of mental disorders, thus making adjustment for severity of the disorder impossible. We do not know whether persons with somatic disorders had more severe mental disorders, which might enhance recognition and treatment. In the case of depression, Katon and Schulberg (
32 ) found that major depressive disorder occurs among 2%–4% of persons in the community, 5%–10% of primary care patients, and 10%–14% of medical inpatients. Another limitation of this study is that the data are quite old (1996). However, because the role of the general practitioner as gatekeeper has not changed since the NEMESIS survey was conducted, it can be postulated that the findings are of clinical and health services significance.
Conclusions
Mental health care utilization patterns among patients with comorbid mental and somatic disorders can be seen as an expression of the filter model of access to mental health care: combinations of disorders that enhance recognition or the need for treatment may lead to mental health care utilization. Among persons with anxiety disorders or substance use disorders who had any of 31 comorbid somatic conditions, recognition and treatment of the mental disorder was higher, possibly because of more severe symptoms from comorbidity or more frequent primary care visits. For persons with mood disorders who had any somatic comorbidity, the findings indicate that recognition of the mood disorder was relatively low. This may have resulted from a lack of vitality being attributed to the somatic disorder, even though a lack of vitality is a symptom in mood disorders (attribution bias). Research is needed to differentiate lack of vitality related to somatic diseases from that related to mood disorders among patients with comorbid conditions, and screening instruments should be developed and made available for this purpose.
Acknowledgments and disclosures
NEMESIS was funded by a grant of the Ministry of Health Welfare and Sports of the Netherlands.
The authors report no competing interests.