Mental disorders are among the most common debilitating chronic diseases worldwide (
1 ). In 2004, 25% of Americans had a mental illness within the past year, and a quarter of those had a serious disorder that significantly disrupted their daily functioning (
2 ). The economic burden of serious mental illness is enormous: $317.6 billion in 2002 (61% for lost earnings, 32% for health care expenditures, and 8% for disability benefits) (
3 ).
Untreated mental disorders can cause much unnecessary personal distress, prolonged family burden, preventable disability, and even premature death and are more likely to persist, recur, and increase in severity (
4,
5 ). Prevention and cost-effective treatments are available for many mental disorders (
5,
6 ). However, among the 24.6 million adults with serious psychological distress in 2004, only 11.1 million (45%) received treatment for mental illnesses. Among those without health insurance, less than one-third received treatment (
7,
8 ).
Severity of the disorder, degree of social dysfunction, and sociodemographic factors such as sex, age, education, marital status, and employment status are known to be associated with and influence receipt of treatment (
9,
10 ). Andersen developed the Behavioral Model of Health Services Use to explain large observed disparities between need and the amount (frequency and duration) and quality of health care received (
11,
12 ). This model relates individuals' use of health services to their predisposition to use these services, factors enabling or impeding service use, and their perceived need for service.
This study used Andersen's Behavioral Model of Health Services Use to examine correlates and predictors of receipt of treatment for mental or emotional problems among community-dwelling adults surveyed by the Behavioral Risk Factor Surveillance System (BRFSS) in 2007.
Methods
BRFSS is an ongoing, state-based, random-digit-dialed telephone survey of the U.S. civilian, noninstitutionalized population aged 18 years and older, conducted in 50 states, the District of Columbia, and three U.S. territories. The median response rate among all states and territories, based on Council of American Survey and Research Organizations guidelines, was 51.4% (range=35.1%–66.0%) in 2006, 50.6% (range=26.9%–65.4%) in 2007, and 53.3% (range=35.8%–65.9%) in 2008. The median cooperation rate was 74.5% (range=56.9%–83.5%) in 2006, 72.1% (range=49.6%–84.6%) in 2007, and 75.0% (range=59.3%–87.8%) in 2008. Surveillance methodology, design, implementation, and response rates are available at
www.cdc.gov/brfss/technical_infodata/quality.htm and
www.cdc.gov/BRFSS/technical_infodata/index.htm .
Thirty-five states, the District of Columbia, and Puerto Rico collected data in 2007 on nonspecific psychological distress and other questions related to health and health-risk behaviors. A total of 169,546 community-dwelling respondents provided complete information on all variables of interest for this analysis.
The Kessler-6 scale (K6) asks respondents about the following six symptoms over the preceding 30 days (
13 ): "In the past 30 days, how often did you feel: nervous, hopeless, restless or fidgety, so depressed that nothing could cheer you up, that everything was an effort, worthless?" Respondents specified how often they experienced each of these items using a 5-point Likert scale ranging from 0, none of the time, to 4, all the time. The total K6 score sums these six values. Possible scores range from 0 to 24, with increasing scores reflecting increasing psychological distress. Previous validation studies classified persons scoring 13 or greater as having serious psychological distress in the past 30 days, persons scoring 8–12 as having probable mild to moderate psychological distress, and persons scoring 0–7 as having no probable psychological distress (
13 ).
Utilization of health professional services for treatment of mental or emotional problems, the dependent variable in this study, was based on an affirmative answer to the question "Are you now taking medicine or receiving treatment from a doctor or other health professional for any type of mental health condition or emotional problem?"
Predisposing factors of interest were age, sex, marital status, education, and race or ethnicity. Enabling or impeding factors for treatment were income, health insurance, and emotional support. Perceived need was assessed from answers to three questions: "Thinking about your physical health, which includes physical illness and injury, for how many days during the past 30days was your physical health not good?" (measuring the number of physically unhealthy days); "Thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?" (measuring the number of mentally unhealthy days); and "Would you say that in general your health is excellent, very good, good, fair, or poor?" (measuring self-rated health). Evaluated need was assessed from the K6 psychological distress severity level.
Consistent with Andersen's Behavioral Model of Health Services Use, four multivariate logistic regression models were used to compute odds ratios for using health professional services for the treatment of mental or emotional problems. These models progressively adjusted for predisposing factors, enabling and impeding factors, perceived need, and evaluated need (
11,
12 ). Model 1 included only the predisposing variables (age, gender, race-ethnicity, marital status, and education). Model 2 added enabling or impeding factors (annual household income level, having health insurance, and frequency of receipt of emotional support). Model 3 added perceived need (number of physically unhealthy and mentally unhealthy days and self-rated health status). Finally, Model 4 added evaluated need, the K6 psychological distress total score.
To account for the complex survey design, all analyses were performed with SPSS, version 14.0, with the Complex Samples add-on module that supports Taylor-series linearization estimation of sampling errors for weighted descriptive statistics, cross-tabulations, and logistic regression. Cross-tabulations estimated the percentage of respondents with predisposing factors, enabling or impeding factors, perceived need, and evaluated need. Logistic regressions estimated the adjusted odds ratios (ORs) and their 95% confidence intervals for receipt of treatment associated with the predisposing factors, enabling or impeding factors, perceived need, and evaluated need.
Results
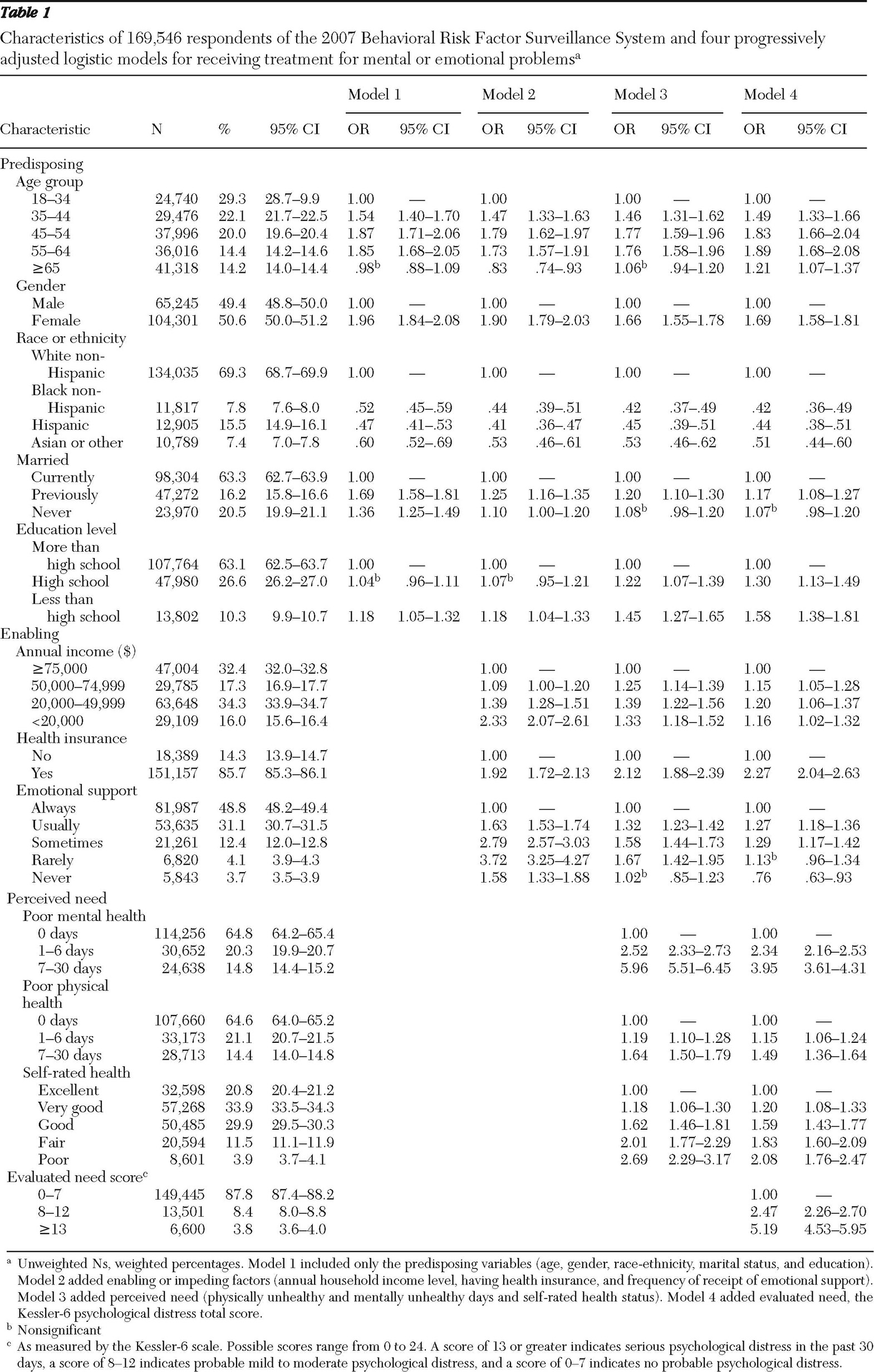
As shown in
Table 1, 29% of the weighted study population were younger than 35 years, and another 29% were older than 55 years. Just over half (51%) were female, approximately two-thirds (69%) were white non-Hispanics, 63% were currently married, and 63% had attended some college or were college graduates. The median annual income reported was approximately $50,000. Over 85% of the respondents had a health insurance plan, and 80% always or usually received emotional support. Sixty-five percent reported zero mentally unhealthy or zero physically unhealthy days. Only 4% rated their overall health as poor. Twelve percent reported either mild to moderate or serious psychological distress.
When only predisposing factors were included (model 1), persons aged 45 to 64 years, women, persons previously married or never married, and those with less than a high school education were more likely to have received treatment than those aged 18 to 34 years, men, persons currently married, and those with at least some college education, respectively. Black non-Hispanics, Hispanics, and Asians or other racial ethnic groups were significantly less likely than white non-Hispanics to receive treatment (
Table 1 ).
After enabling factors were added (model 2), persons with annual household incomes less than $50,000, those with health insurance, and those usually, sometimes, rarely, or never receiving emotional support were more likely to receive treatment than those with incomes of $75,000 or higher, those without health insurance, and those always receiving emotional support, respectively. The association between receiving treatment and never having married disappeared (
Table 1 ).
Those with more mentally and physically unhealthy days and less than excellent self-rated health were more likely to receive treatment than those with fewer mentally and physically unhealthy days and excellent self-rated health, respectively (model 3). Adding these perceived need variables attenuated the associations between receiving treatment and the following groups: women, persons having an annual household income of <$20,000, and persons not always receiving emotional support.
When all variables were entered simultaneously (model 4), the highest level of the evaluated need, serious psychological distress, was the factor most strongly associated with treatment (OR=5.19). Evaluated need attenuated the association between treatment and the following groups: persons receiving emotional support only sometimes or rarely and those reporting seven to 30 mentally unhealthy days.
Discussion
The associations between each of the predisposing factors, enabling or impeding factors, perceived need, evaluated need, and treatment generally agree with the associations reported in the literature (
14 ). Although evaluated need played a strong and significant role for receipt of treatment for mental or emotional problems, predisposing, enabling, and impeding factors were significantly correlated with receipt of treatment, even after adjustment for perceived and evaluated need.
Studies based on BRFSS data have two overarching limitations. First, only households with land-line telephones are included in the survey sample; households with only cell phones and households without telephones are excluded. Response rates continue to decline because of changes in telecommunication usage (for example, increases in the number of households with only cell phones and telephone number portability). The Centers for Disease Control and Prevention is monitoring the effect of changes in telecommunication usage by conducting research on sampling cell-phone numbers, sending pre-notification letters, reaching respondents who speak languages other than English and Spanish, and multiple-mode data-collection techniques. Second, BRFSS data are self-reported and are subject to recall bias and social desirability effects. Despite these limitations, BRFSS data have been demonstrated to provide valid and reliable estimates when compared with national household surveys in the United States (
15 ). BRFSS is a cost-effective and timely method for collecting state and local data, and often it is the only data source available to communities to assess local health conditions and track progress.
The main limitations of this study are that it included only self-reported data and it was unable to determine cause-and-effect relationships because of BRFSS's cross-sectional design. BRFSS did not ask about the medication or the treatment (type, frequency, and duration), so we could not determine whether the medication and the treatment accounted for the observed associations. Because BRFSS did not ask about the characteristics of the mental or emotional problems (age of onset, lifetime diagnoses, and number of episodes), it is impossible to classify respondents by their state of remission, recovery, relapse, or recurrence, all known to influence utilization of health professional services for receipt of medication or treatment. Despite these limitations, these results suggest that treatment for mental or emotional problems may not be equitably distributed among community-dwelling adults but instead may reflect social and cultural determinants that include but are not limited to the predisposing, enabling, impeding, and perceived need factors analyzed here.
Conclusions
The public mental health system should seriously consider that health services utilization is socially patterned and not just an individual behavior. Although predisposing, enabling, and impeding factors are necessary to determine whether a person receives professional care for mental or emotional problems, these factors alone are not sufficient. A person must also perceive that he or she has an illness before receiving care. Because perception of illness severity is the strongest and most direct cause of health service use and because perceived need appears to affect treatment independent of evaluated need, questions about perceived need should be included in health assessments. Moreover, additional questions relating to age of onset, family history, lifetime diagnoses, and treatment status may help better explain the inequitable distribution and need for treatment among disparate populations.
Acknowledgments and disclosures
The authors report no competing interests.