The New Freedom Commission on Mental Health stated that access to effective acute inpatient and other short-term 24-hour services is an essential component of a balanced system of mental health care, which is especially important for persons in crisis who need the safety and intensive treatment offered in these settings (
1 ). Community hospitals are the primary source of inpatient psychiatric treatment in the United States, based on number of admissions (
2,
3 ). Community hospital inpatient psychiatric care can be provided in a distinct part of the hospital in psychiatric units that are organized and staffed specifically to treat psychiatric disorders, or it can be scattered throughout in general medical beds, sometimes known as "scatter beds." Psychiatric care in scatter beds may occur even in hospitals with separate psychiatric units.
Current information is very limited on the extent to which scatter beds are used for patients with psychiatric disorders and if any characteristics of these patients are associated with the use of scatter beds. Studies that examine treatment in psychiatric units, compared with treatment in scatter beds, are often limited to a subset of discharges, such as Medicare patients, and most of these studies were done ten or more years ago. Several studies have found that patients treated in scatter beds have shorter lengths of stay than those treated in psychiatric units (
4,
5,
6,
7 ). Research also suggests that compared with patients treated in psychiatric units, patients with psychiatric disorders treated in scatter beds tend to be older and are more likely to be receiving Medicare, to present with somatic complaints, to have greater medical comorbidity, and to have a principal diagnosis other than schizophrenia, bipolar disorder, or major depressive disorder (
4,
5,
6,
7,
8 ).
Limited research has focused on how treatments provided in scatter beds differ from those provided in psychiatric units. Mechanic and Davis (
6 ) found that psychiatric patients in scatter beds were rarely attended by psychiatrists and that they had more CAT scans and electroencephalograms (EEGs) than patients in psychiatric unit beds. Olfson (
8 ) found that patients in a psychiatric unit were more likely than psychiatric patients treated in scatter beds to receive antidepressants. Norquist and colleagues (
9 ) concluded that the quality of care for the psychological aspects of depression treatment may be better in psychiatric units, whereas the quality of general medical care may be better in general medical beds.
In 2005 there were approximately 1,245 psychiatric units in the United States (author calculation based on Medicare Cost Reports). Approximately 25% to 30% of all community hospitals had distinct psychiatric units. In recent years, the number of psychiatric units has declined, from 1,458 in 1998 to 1,245 in 2005 (author calculation based on Medicare Cost Reports). The decline of psychiatric unit beds, in tandem with the decline in free-standing psychiatric hospital beds and a lack of outpatient alternatives, has resulted in a shortage of psychiatric beds, at least in some communities. A 2006 survey of state mental health agency directors revealed that 80% of the states reported shortages in psychiatric beds (
10 ). The shortage was also documented in the 2004 New Freedom Commission Subcommittee on Acute Care (
1 ). One potential consequence of the lack of psychiatric beds has been overcrowding and increased waiting time in community hospital emergency rooms, as reported by emergency room directors (
11,
12 ). Another consequence, about which few data exist, may be lack of access to any hospital treatment. To what extent and how scatter beds are being used to fill the void in psychiatric bed availability is unclear. The question of how many of the approximately 1.8 million community hospital discharges with a principal psychiatric diagnosis are from scatter beds has not been examined since the 1980s.
The goal of this study was to describe the extent to which scatter beds are being used across a sample of states. The study also compared the characteristics of patients with psychiatric diagnoses who were discharged from community hospital psychiatric units with those who were discharged from scatter beds. The aim is to inform policy makers about how scatter beds are currently being used and to stimulate consideration of their appropriate role in acute, inpatient psychiatric care.
Methods
The data were from the State Inpatient Databases (SID), part of the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ). The databases contain the universe of inpatient hospital discharge abstracts from participating states. SID data compose a core set of clinical and nonclinical information on all patients, regardless of payer, including persons covered by Medicare, Medicaid, and private insurance and those who are uninsured.
This project took advantage of the revenue codes found on the discharge abstracts from some of the participating SID states. Revenue codes were used to identify the type of room and board accommodations for each inpatient stay. Particular codes refer to charges for psychiatric unit room and board and thus can be used to identify patients who were treated in psychiatric units. Specifically, any patients who were discharged with the following revenue codes were identified as having been treated in a psychiatric unit: 0114, 0124, 0134, 0144, or 0154. The study focused on discharge records for patients who were given a principal psychiatric diagnosis ( ICD-9-CM codes 295–302, 306–314).
Two additional sources of information on the hospital psychiatric units were used to verify the identification of units based on SID revenue codes. The first source was the American Hospital Association's (AHA's) Annual Survey of Hospitals, which includes questions regarding the presence of a psychiatric unit. The second source was Medicare Cost Reports, which also indicate whether the hospital has a psychiatric unit and thus should be paid under the separate Medicare payment system for psychiatric units (in effect during the period of this analysis). For the uncommon cases where these sources conflicted, the Internet was searched to determine whether the hospital listed a psychiatric unit as one of its services.
Using 2003 data (
13 ) we identified 12 states that had revenue codes of sufficient completeness to be useful for the study: Kentucky, Maine, Massachusetts, Nebraska, Nevada, New York, North Carolina, Pennsylvania, Tennessee, Texas, Washington, and West Virginia. Because HCUP partner agreements prohibit disclosure of specific state names when reporting some data elements, state-specific data were reported by assigned alphabetical letters for identification rather than state name. Estimates of the prevalence of psychiatric unit discharges, psychiatric units, and psychiatric unit beds per capita were created with population estimates from the U.S. Census. We examined records for patients with a principal psychiatric diagnosis and compared those who were treated in hospital psychiatric units and those who were treated outside of a psychiatric unit in a medical-surgical bed, which we refer to as scatter beds. The factors compared included age; gender; length of stay; specific principal
ICD-9-CM psychiatric diagnoses (grouped by
ICD-9-CM diagnosis groups); existence of any secondary psychiatric, substance use disorder, or nonpsychiatric or nonsubstance abuse
ICD-9-CM diagnoses (grouped by the Clinical Classification Software [14]); expected primary source of payment; mean total charges; admission source; and discharge type. Chi square and t tests were used to compare differences between the characteristics of discharges from psychiatric units and scatter beds. Because the study used deidentified administrative data that were compliant with the Health Insurance Portability and Accountability Act, institutional review board approval was not needed.
Results
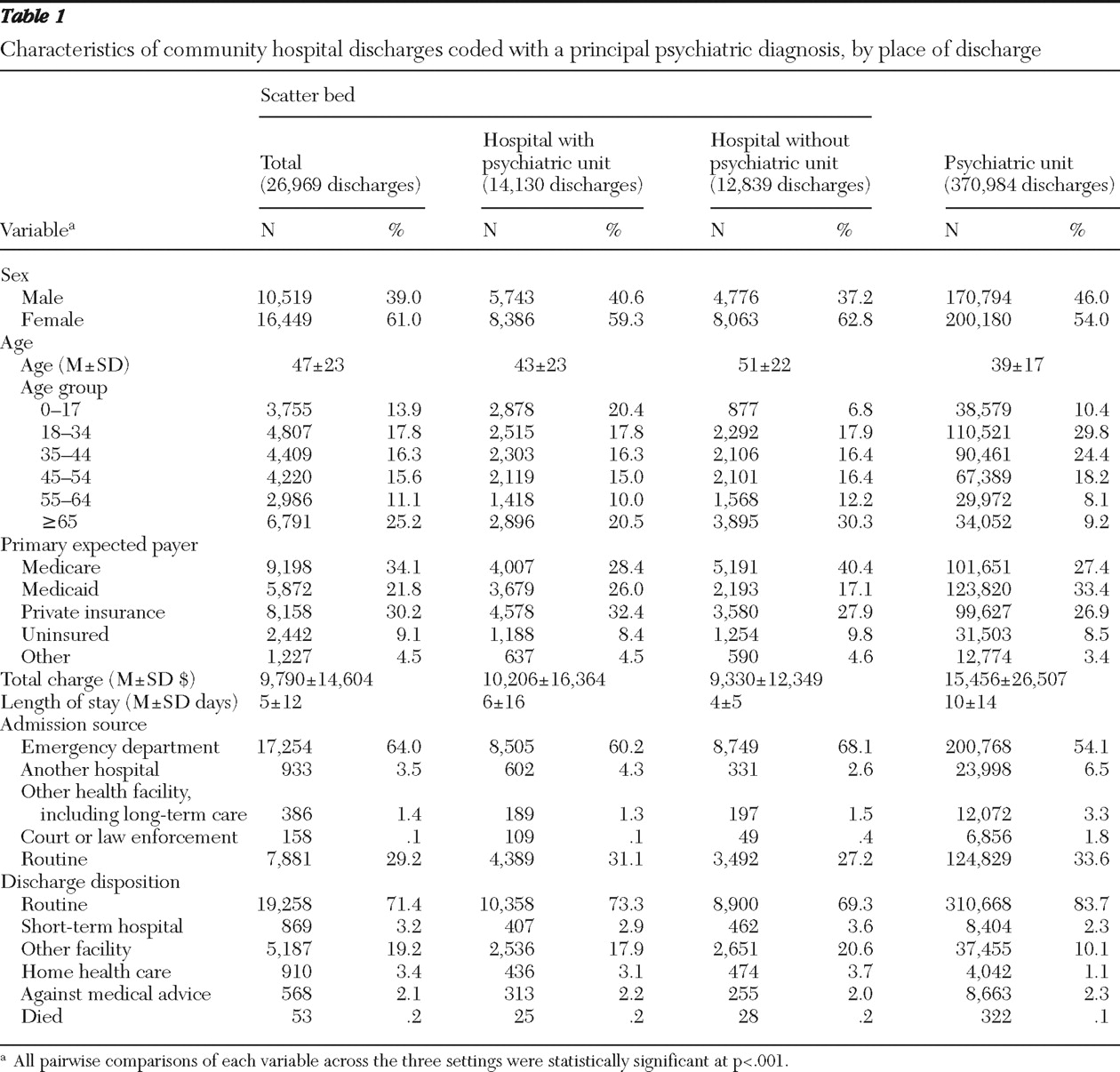
Thirty-nine percent (N=496) of the 1,274 hospitals in the 12 states had a psychiatric unit (data not shown). Overall, of the 397,953 discharges in 2003 that were examined, 93.2% were from a psychiatric unit and 6.8% were from a scatter bed (
Table 1 ). The percentage of scatter bed discharges was about equally divided between hospitals that had a psychiatric unit (3.6%) and those that did not (3.2%) (
Table 1 ).
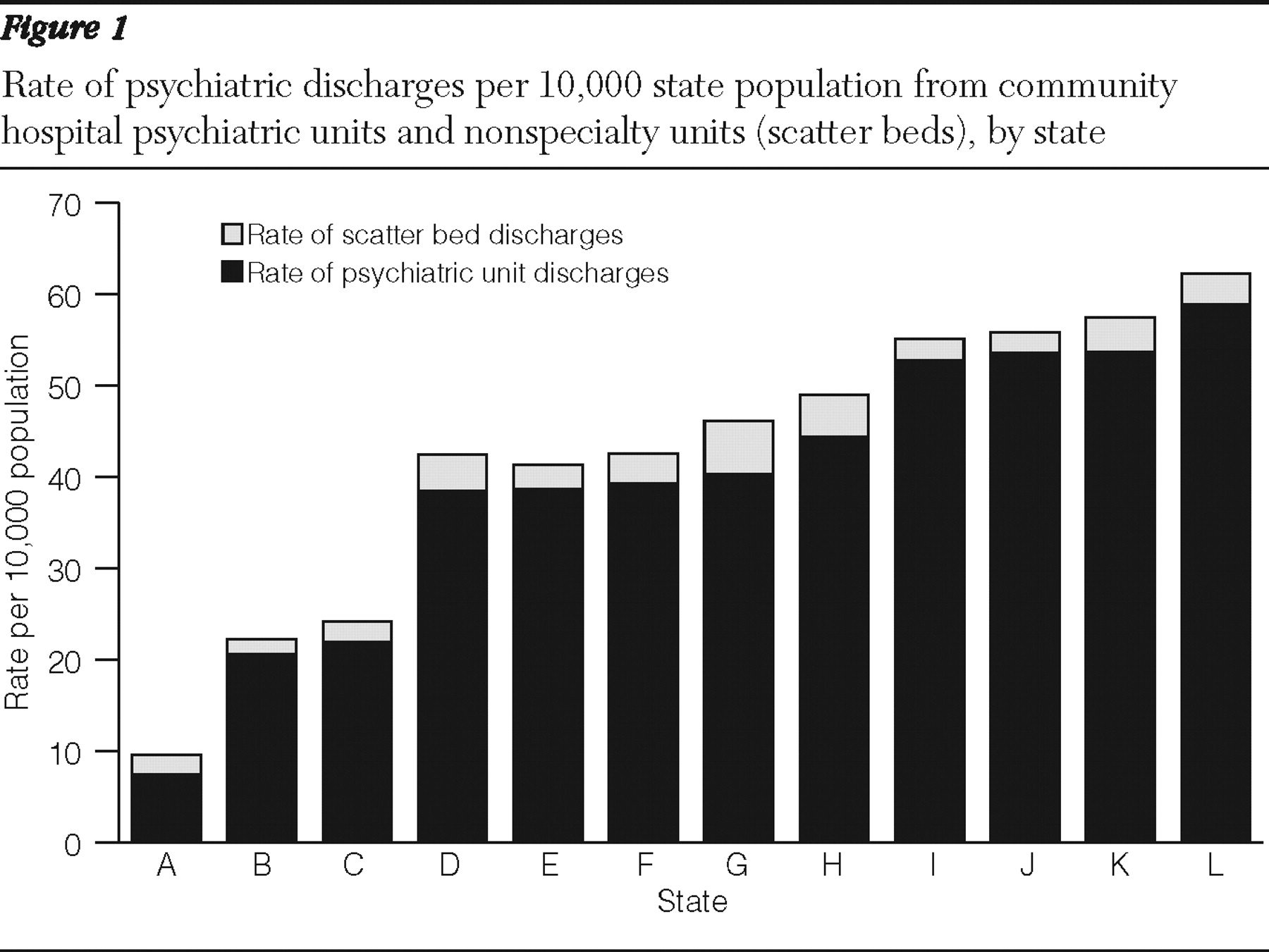
The rate of total community hospital psychiatric discharges per 10,000 total state population ranged from 9.6 to 62.3 (
Figure 1 ). The average rate of scatter bed discharges was 2.8 per 10,000, with a minimum of 1.6 and a maximum of 5.8. The average rate of psychiatric unit discharges per 10,000 was 40.3, with the rate ranging from 7.4 to 58.9.
Table 1 describes the characteristics of discharges from psychiatric units, scatter beds in hospitals with psychiatric units, and scatter beds in hospitals without psychiatric units. Results are presented for all states combined. All pairwise comparisons of each variable across the three settings were statistically significant at p<.001.
Females accounted for a higher percentage of scatter bed discharges than psychiatric unit discharges (61.0% versus 54.0%). Patients with the youngest mean age (39 years) were discharged from psychiatric units, followed by scatter beds in hospitals with psychiatric units (43 years) and scatter beds in hospitals without psychiatric units (51 years). Only 9.2% of the psychiatric unit discharges were for persons older than 65 years, compared with 20.5% for scatter beds in hospitals with psychiatric units and 30.3% for scatter beds in hospitals without psychiatric units.
For all payers, at least 90% of discharges were from a psychiatric unit (data not shown in Tables). Consistent with the age findings, the percentage of discharges billed to Medicare was highest among scatter beds in hospitals without psychiatric units (40.4%) and lower for discharges from scatter beds in hospitals with psychiatric units (28.4%) and from psychiatric units (27.4%). Psychiatric units tended to have a higher percentage of Medicaid patients discharged than the other two settings (33.4% versus 26.0% in scatter beds in hospitals with a psychiatric unit and 17.1% in scatter beds in hospitals without a psychiatric unit). Uninsured status was most common in scatter beds in hospitals without psychiatric units (9.8%) and somewhat less common in psychiatric units (8.5%).
Average total charges per discharge were highest in psychiatric units ($15,456), followed by discharges from scatter beds in hospitals with psychiatric units ($10,206) and those from scatter beds in hospitals without psychiatric units ($9,330). Consistent with the findings for total charges, average length of stay was highest among the discharges from psychiatric units (ten days), followed by those from scatter beds in hospitals with psychiatric units (six days) and those from scatter beds in hospitals without psychiatric units (four days).
Emergency room admissions were most common among patients treated in scatter beds in hospitals without psychiatric units (68.1%), followed by patients treated in scatter beds in hospitals with psychiatric units (60.2%) and patients from psychiatric units (54.1%). As would be expected, discharges from psychiatric units were more likely to have patients were admitted through a transfer from another hospital (6.5%), and scatter beds in hospitals without psychiatric units were the least likely to have patients admitted in such a manner (2.6%). Discharges from scatter beds in hospitals without psychiatric units were more likely result in a patient being transferred to another facility (20.6%), and discharges from hospitals with psychiatric units were least likely to result in transfer to another facility (10.1%).
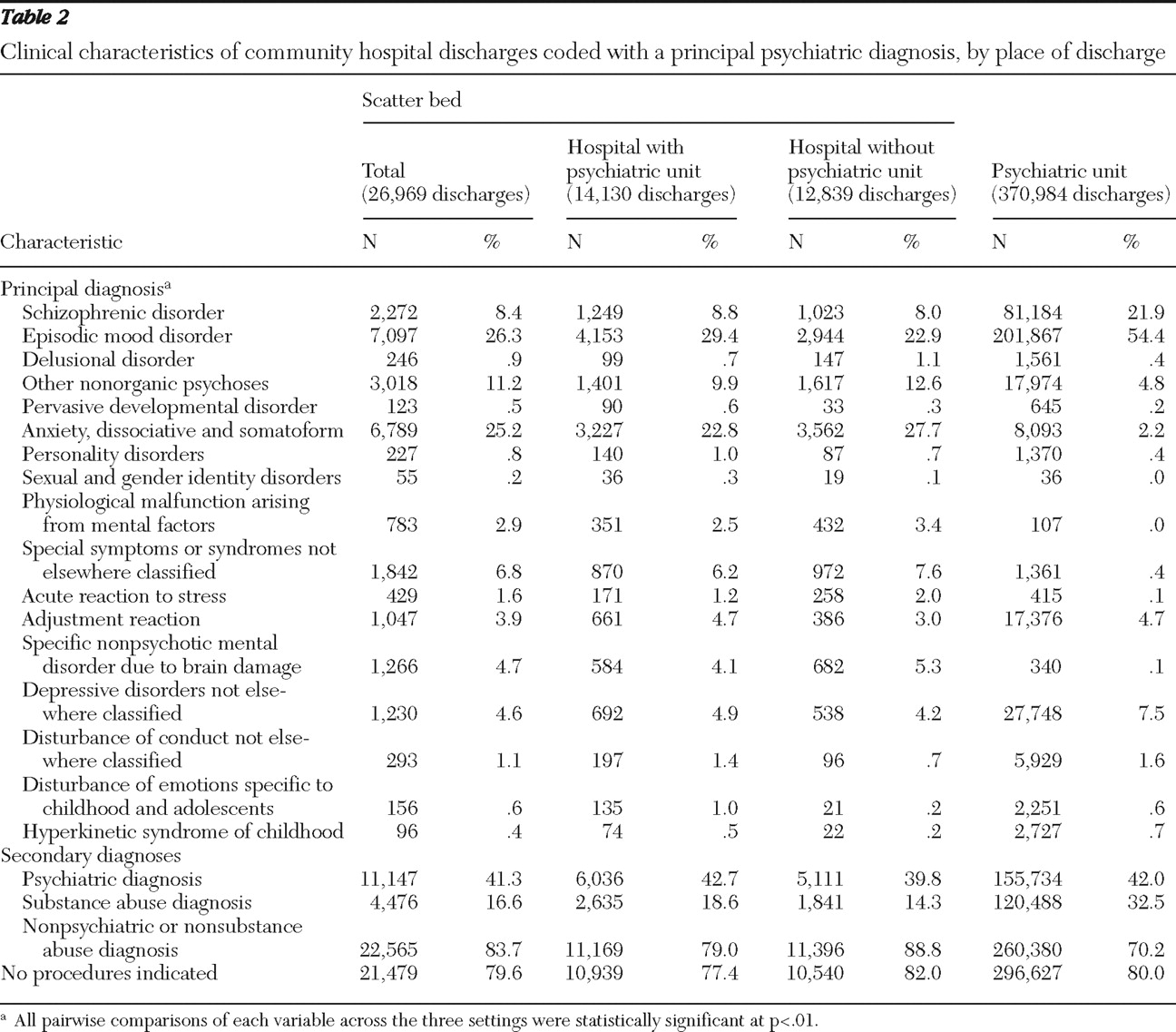
As shown in
Table 2, schizophrenia disorders (
ICD-9-CM code 295) were much more common in psychiatric units than in scatter beds (21.9% in psychiatric units versus 8.8% in scatter beds in hospitals with psychiatric units and 8.0% in scatter beds in hospitals without psychiatric units). Similarly, episodic mood disorders (
ICD-9-CM code 296) were much more common in psychiatric units than in scatter beds. In fact, episodic mood disorders made up more than half of all psychiatric unit discharges (54.4% in psychiatric units versus 29.4% in scatter beds in hospitals with psychiatric units and 22.9% in scatter beds in hospitals without psychiatric units). In total, about 84% of psychiatric unit discharges were coded with a principal diagnosis of schizophrenia, episodic mood disorder, or depressive disorder (
ICD-9-CM code 311), whereas less than half of scatter bed discharges were coded with these diagnoses (35.1% of scatter beds in hospitals without psychiatric units and 43.1% of scatter beds in hospitals with psychiatric units). The most common diagnosis in scatter beds was anxiety, dissociative, and somatoform disorders (
ICD-9-CM code 300) (25.2%). Anxiety disorders made up only 2.2% of discharges from psychiatric units compared with 22.8% of discharges from scatter beds in hospitals with psychiatric units and 27.7% of discharges from scatter beds in hospitals without psychiatric units. Discharges coded with a principal diagnosis of other nonorganic psychosis (
ICD-9-CM code 298) were more common in scatter beds (11.2%) than in psychiatric units (4.8%).
Approximately one-third of psychiatric unit discharges were coded with a secondary substance use disorder diagnosis, whereas less than 20% of scatter bed discharges were coded with such a diagnosis (18.6% from scatter beds in hospitals with psychiatric units and 14.3% from scatter beds in hospitals without psychiatric units). A code for a secondary nonpsychiatric or substance abuse diagnosis was the most common in discharges from scatter beds in hospitals without psychiatric units (88.8%), followed by those from scatter beds in hospitals with psychiatric units (79.0%) and those from psychiatric units (70.2%).
We also examined the most frequent secondary diagnoses across the three settings using AHRQ's Clinical Classifications Software (not shown in tables). Across the three settings, seven codes were common to the top ten most frequent codes (substance-related mental disorders, alcohol-related mental disorders, essential hypertension, diabetes, esophageal disorders, thyroid disorders, and hyperlipidemia). In psychiatric units, asthma and other nutritional, endocrine, and metabolic disorders were among the top nine. Coronary atherosclerosis and other heart disease as well as senility and organic mental disorder were among the ten most frequent diagnoses coded in discharges from scatter beds in hospitals without psychiatric units. Among those from scatter beds in hospitals with psychiatric units, coronary atherosclerosis and other heart disease and other nutritional, endocrine, and metabolic disorders were among the top nine. Secondary nonpsychiatric diagnoses were slightly more common in scatter beds.
Across all settings, approximately 80% of psychiatric discharges had no procedure code indicated. The percentage with no procedure code was relatively similar across settings (82.0% from scatter beds in hospitals without psychiatric units, 77.4% from scatter beds in hospitals with psychiatric units, and 80.0% in psychiatric units). Across all types of health conditions treated in hospitals, only about 36% of discharges have no procedure code (not shown in tables).
Discussion
Data revealed that across the 12 states, only 6.8% of discharges with a principal psychiatric diagnosis code were for patients treated in scatter beds and the other 93.2 % were for patients treated in psychiatric units. The percentage of scatter bed discharges with a code for a principal psychiatric diagnosis was about equally divided between hospitals that had a psychiatric unit and those that did not. The number of psychiatric community hospital discharges per capita varied widely across the 12 states examined, overall and by setting. The rate of total community hospital psychiatric discharges per 10,000 individuals in the state ranged from 9.6 to 62.3. The average rate of scatter bed discharges was 2.8 per 10,000, with a minimum of 1.6 to a maximum of 5.8. The average rate of psychiatric unit discharges was 40.3, with a range of 7.4 to 58.9.
Compared with patients in a psychiatric unit, patients treated in scatter beds were more likely to be older and on Medicare. They were more likely to be admitted from the emergency room, have shorter lengths of stay, and be transferred to another facility. They were less likely to have schizophrenia, episodic mood disorders, or depressive disorders, although 35%–43% of patients treated in scatter beds in hospitals without units had these principal diagnoses. The most common diagnosis in scatter beds, making up about one-fourth of all discharges, was anxiety, dissociative, and somatoform disorders. Other nonorganic psychoses were also more common among discharges from scatter beds in hospitals without psychiatric units, compared with psychiatric units.
This study is subject to certain limitations. The data came from 12 states and are not nationally representative; in particular, the states vary in the number of available psychiatric unit beds. Second, the data were obtained from administrative records, which did not contain details about the types of providers treating patients within hospitals (such as the extent to which patients were treated by consulting psychiatrists or psychiatric nurses), about the particulars of the clinical services offered (such as what types of psychoactive medications patients were provided), or about the details of the reasons for the admissions (such as whether the patient was at risk of harming him- or herself or others). Third, chart review was not conducted to validate the diagnoses contained in the billing records, and it is possible that psychiatric diagnoses were undercoded in scatter beds. Fourth, by pooling data across states, we have presented data on the distribution of patient characteristics on average across the 12 states rather than within each state. Finally, the study focused on community hospitals, and an important extension is to marry the HCUP SID data with information on psychiatric hospital beds, as well as with information on the availability of outpatient services. Despite these caveats, the study is one of the few to provide a sense of the availability and use of hospital psychiatric units and scatter beds and the types of patients being served in different settings within community hospitals.
The estimate from this analysis that only 6.8% of mental health care discharges were from scatter beds in 2003 is much lower than prior estimates. In particular, Kiesler and Simpkins (
7 ) estimated that in 1980, 33% of psychiatric community hospital discharges were from scatter beds. Their estimates were based on a study that linked 1980 data on psychiatric units from the National Institute of Mental Health (NIMH) and the AHA with information on psychiatric discharges from the National Hospital Discharge Survey. In a recent analysis that linked Medicare Cost Reports data on psychiatric unit status to HCUP SID data from all states, we estimated that between 6% and 20% of discharges were from scatter beds, with the best estimate being 6% (
15 ). The high estimate of 20% assumed that the Medicare Cost Reports captured all psychiatric units. However, additional analysis based on hospital psychiatric discharge volume, hospital Web sites, and the AHA data indicated that the Medicare Cost Reports miss some hospitals and the best estimate is probably that 6% of discharges are from scatter beds. Thus, if we assume that the NIMH and AHA surveys used in Kiesler and Simpkins' study captured psychiatric units as well as the Medicare Cost Reports and that the other methodological differences are not great, it appears that the percentage of discharges from scatter beds has declined since the 1980s. This decline in scatter bed utilization may be due to the significant expansion in number of psychiatric units and beds that occurred after the implementation of Medicare PPS (prospective payment system) in 1983 (
16 ).
The relatively low use of scatter beds across the states has several implications. First, if scatter beds are not being used often for psychiatric treatment, the importance of psychiatric units may be magnified. This may be particularly true given the decline in public and private psychiatric free-standing hospital beds. In some regions of the country, the low supply of psychiatric beds appears to be limiting access to care and resulting in more patients staying longer in emergency rooms (
1,
10,
11,
12,
17,
18,
19 ). However, it is important to note that determining the appropriate supply of psychiatric beds is a complex problem and dependent, in part, on a community's outpatient infrastructure and the extent to which an individual's financial resources allow him or her to access alternative services.
The trend in declining psychiatric unit beds may be further exacerbated if the new PPS for psychiatric care in community hospitals places additional financial pressure on community hospitals (
20 ). In 2005 Medicare began paying for inpatient psychiatric services on a prospective basis, ending a PPS exemption for psychiatric facilities that began in 1983. The PPS methodology sets a prospective per diem base payment rate with payments for each case adjusted by patient characteristics (for example, age, principal diagnosis, selected comorbidities, length of stay, and emergency room usage) and facility characteristics (for example, rural location, teaching status, geographic wage index, and geographic cost of living). Outlier payments were also established. The impact of PPS on community hospital psychiatric unit bed supply is uncertain and may depend on unmeasured patient mix, such as the extent to which a hospital admits patients who require one-on-one observation because of their risk of harming themselves, the cost structure of the hospital, and the generosity of Medicare payment relative to that of other insurers (
21 ).
These data suggest that when scatter beds are being used, they may often be employed as a short-term substitute for specialty psychiatric beds. Placing psychiatric patients in general medical-surgical beds may be an appropriate response to a lack of psychiatric beds for patients who are medically stable and need psychiatric treatment, particularly in rural areas. However, at this point little is known about the nature and quality of psychiatric care being provided in scatter beds. In evaluating the appropriate supply of psychiatric unit beds and the role of scatter beds, particularly in regions where psychiatric units are sparse, a number of issues must be addressed. These include the availability and training of staff to assess patient needs, the ability of staff to closely monitor patients who may be dangerous to themselves or others, the availability of consulting psychiatrists and other psychiatric specialists, the adequacy of reimbursement for psychiatric treatment, and the ability of hospitals to coordinate care with other behavioral health providers in the community.
In addition to identifying the important role that psychiatric units play in short-term inpatient treatment, this study highlights the wide variation in the supply of psychiatric beds across the states. This finding demonstrates the need to examine more closely the adequacy of mental health services across the continuum of service needs within particular communities. Localities with hospital alternatives, such as crisis residential programs, may require fewer hospital beds. Similarly, communities with a strong outpatient mental health system may be able to discharge patients sooner. Planning for an adequate supply of acute care psychiatric beds is hindered by the lack of clear guidelines for what level of acute care is appropriate for mental health consumers in crisis and a lack of consensus on standards for assessing the number of beds needed in a community and the ideal mix of services in a community-based system of care (
1 ). The planning process must also focus on how hospitals without psychiatric units should treat patients with psychiatric illness. As the AHA Task Force on Behavioral Health recently noted, "Every hospital treats patients with behavioral health disorders, even when an acute care, community hospital has no organized behavioral health services or psychiatric clinical specialists," and all hospitals should give more attention to planning for the needs of patients with principal or secondary psychiatric disorders (
22 ). Because community hospitals are now a major component of psychiatric care, it is important to have more deliberate policies and treatment strategies regarding psychiatric treatment in community hospitals.
Conclusions
The study illustrates that scatter beds are used in a limited way to supplement psychiatric units. The variation in psychiatric hospitalization across communities highlights the need for research to understand the appropriate supply of psychiatric unit beds and the appropriate way to deliver psychiatric care in regions of the country with limited access to psychiatric units. Additional research and policy making are particularly urgent because of recent changes in how psychiatric units are reimbursed.
Acknowledgments and disclosures
This work was jointly funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Agency for Healthcare Research and Quality (AHRQ) under contract number HHSA-290-2006-00009-C. The authors acknowledge the state data organizations that participated in the 2003 Healthcare Cost and Utilization Project State Inpatient Databases. Partners for the 12 states that provided data for this analysis were as follows: Kentucky Cabinet for Health and Family Services, Maine Health Data Organization, Massachusetts Division of Health Care Finance and Policy, Nebraska Hospital Association, Nevada Department of Health and Human Services, New York State Department of Health, North Carolina Department of Health and Human Services, Pennsylvania Health Care Cost Containment Council, Tennessee Hospital Association, Texas Department of State Health Services, Washington State Department of Health, and West Virginia Health Care Authority. The authors also acknowledge the programming support of Daniel Whalen, B.A., and the editorial support of Cheryl Kassed, Ph.D. This article does not necessarily reflect the views or policies of SAMHSA, AHRQ, or the Department of Health and Human Services, and the authors are solely responsible for its content.
The authors report no competing interests.