In 2004 the U.S. Preventive Services Task Force presented recommendations on screening for alcohol misuse among primary care patients. They concluded that alcohol misuse, defined as "'risky/hazardous' and 'harmful' drinking that places individuals at risk for future problems," often leads to increased health problems, disability, violent behavior, poor social relationships, and accidental injury or even death (
1 ). Alcohol use disorders have also been strongly associated with military wartime duty and can have a negative impact on unit effectiveness (
2 ). Alcohol misuse has been associated with misconduct and separation from military service (
3,
4 ), and one study postulated that increased alcohol consumption was at the root of increased injury mortality for veterans of the first Gulf War (
5 ). Alcohol misuse can make it more difficult to treat traumatic brain injury and posttraumatic stress disorder (PTSD), two important conditions identified among veterans of the current wars in Iraq and Afghanistan (
6,
7,
8 ).
In 2005 the Department of Defense (DoD) initiated one of the largest population health screening programs for service members. The Post-Deployment Health Re-Assessment (PDHRA) assesses service members three to six months after they return from combat deployments to identify and facilitate treatment for deployment-related physical or mental health concerns. To screen for alcohol use disorders in the PDHRA, the DoD adapted the Two-Item Conjoint Screen (TICS), which was attractive because of its brevity and acceptable psychometric properties compared with the Composite International Diagnostic Interview-Substance Abuse Module. The TICS asks two questions: "In the past 4 weeks, have you used alcohol more than you meant to?" and "In the past 4 weeks, have you felt you wanted or needed to cut down on your drinking?"
The TICS was developed by Brown and colleagues (
9 ) in order to quickly screen young and middle-aged adults for alcohol and drug problems in civilian primary care settings. The version utilized by DoD focuses only on alcohol use and was validated in a military population against structured clinical interviews (
10 ). The decision to include the TICS questions on the PDHRA was further supported by a study showing that rates of alcohol misuse measured with the TICS were higher after deployment than before (
11 ).
After implementing the PDHRA, DoD conducted a program evaluation. Overall, in these nonanonymous questionnaires, 12% of active component soldiers and 15% of National Guard and reserve component soldiers were willing to answer yes to one or both of the TICS questions. Although these figures were similar to the rates of service members screening positive for PTSD, where 15% of active component soldiers and 36% of reserve component soldiers were referred for further mental health evaluation, the referral rates for alcohol services was only .2%–.6% (
12 ).
The DoD program evaluation raised questions about the utility of the military's populationwide postdeployment alcohol screening effort. Milliken and colleagues (
12 ) concluded that one likely reason for the lack of parity in referral rates between traditional mental health services and alcohol services is the lack of confidentiality of alcohol treatment in the U.S. military. Under current military policies, alcohol treatment triggers automatic involvement of a soldier's commander, in contrast to the various protections afforded service members who utilize other mental health services. Military programs to address alcohol and drug use disorders are separate from medical programs, and alcohol abuse and dependence are often treated as an administrative issue in the U.S. military. Service members can be discharged from the military if they fail to comply with orders for alcohol counseling and treatment.
What ultimately brings a service member to alcohol treatment and education services are the behaviors related to alcohol misuse, such as drunk driving or work-related impairment, rather than a clinical diagnosis from the medical community. However, there have been no data showing a correlation between the TICS employed in the PDHRA and the problem behaviors most affecting occupational functioning. It is possible that positive responses to these questions will not, in fact, be related to behaviors associated with alcohol misuse. They may, for example, measure alcohol use associated with seeking positive, supportive social interaction with others who share the same experiences in war (
13 ) or relate to normative beliefs about excessive drinking behavior in the military being potentially adaptive (
14 ).
The goal of this study was to assess the association of the two-question alcohol screening being used on a large scale in the military with alcohol-related behaviors that can seriously impair functioning or affect a service member's career. Such an association would have strong implications for current large-scale screening efforts.
Methods
This research project analyzed data from the Land Combat Study (
11 ), which examined the relationship between combat and mental health among deployed troops using cross-sectional survey methods. The questionnaire used in the study covered demographic characteristics, combat experience, health problems, and health care utilization (
11 ). From December 2003 to October 2006, self-reported survey responses were collected from 6,527 soldiers in six U.S. Army brigades three to four months after they returned from deployments to Iraq. The recruitment and survey methods of the Land Combat Study have been described previously (
11 ) and are briefly summarized here. Under a protocol approved by the institutional review board of the Walter Reed Army Institute of Research, a complete description of the study and the survey was given to participants at their duty stations, and written informed consent was obtained. Participation was voluntary, and responses were anonymous. Overall, 50% to 60% of soldiers from the participating units were available during the survey administration, with the remainder away primarily because of duty obligations or training. Among those invited to participate, 98% signed the consent form and completed some portion of the survey.
An answer to at least one of these two modified TICS screening questions was considered a positive screen. Response rates to the TICS were correlated with response rates to the following questions regarding alcohol-related behaviors. Participants were asked whether in the past four weeks they drove after having several drinks, rode with a driver who had had too much to drink, were late or missed work because of a hangover, used any illegal drugs or substances, or had a problem with alcohol or drugs that resulted in counseling by the unit or referral to ASAP (Army Substance Abuse Program). Participants were also asked whether they were convicted of driving under the influence (DUI) in the past year.
Tests of independence were used to assess whether the proportion responding yes to at least one TICS question varied with responses to the alcohol-related behavior questions. Crude odds ratios (ORs) and chi square statistics with one degree of freedom were calculated.
Odds ratios adjusted for gender, race-ethnicity, rank, age, education level, and military component (active versus reserve) were calculated using logistic regression (
15 ). The determination of independent variables for inclusion was the result of analysis with stepwise regression, making judgments of the stability of the coefficients in the model and of multicollinearity among the independent variables. Multicollinearity was found among age, rank, and education level, and ultimately, age and education level were dropped in the final model, while rank was retained because of its consistent statistically significant coefficients and the potential for its application in a population-level intervention. On the basis of Hosmer-Lemeshow goodness-of-fit tests, there was no statistically significant deviance from fit. Adjusted and unadjusted odds ratios were very similar, suggesting that confounding was not a serious issue.
Combat exposure was examined with the 18-question Combat Experiences Scale; possible scores range from 0 to 18, with higher scores indicating higher levels of combat exposure (
11 ). The median score in this population was 9, with an interquartile range of 7 to 12. Four combat exposure levels were created: first quartile (score of 0–6, N=1,331), second quartile (score of 7–8, N=1,576), third quartile (score of 9–11, N=1,222), and fourth quartile (score of 12–18, N=1,603). Logistic regression was used to examine the relationship between increasing levels of combat experience and a TICS positive screen.
Chi square tests were used to analyze the association between a TICS positive screen and a positive screen for depression, anxiety, or PTSD. The survey utilized the Patient Health Questionnaire (PHQ) to screen for depression and generalized anxiety (
16 ) and the PTSD Checklist (PCL) to screen for PTSD (
17 ). A strict screening definition was utilized for both, requiring endorsement of symptoms meeting criteria of the
DSM-IV-TR and serious impairment in social or occupational functioning ("very difficult" or "extremely difficult" level on the PHQ) or high endorsement of PTSD symptoms (PCL score ≥50) (
11 ).
Statistical tests were conducted with SPSS, version 13.0, for Mac OS X, and significance levels were set at <.05.
Results
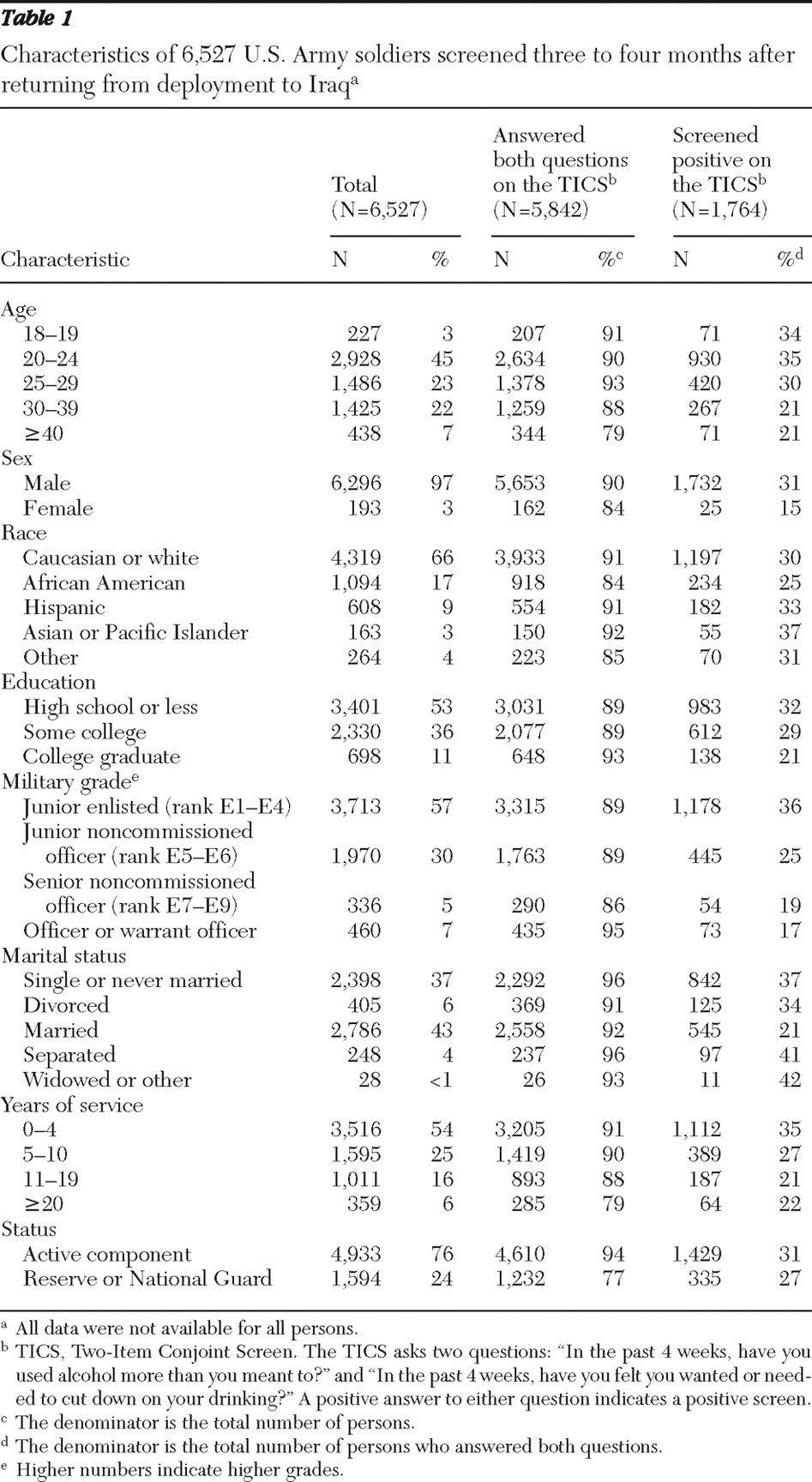
The sample of soldiers studied were representative of the reserve and active duty U.S. Army population (
18 ). Most respondents were junior enlisted (57% had a rank of E1–E4), male (97%), Caucasian (66%), and young (71% were younger than 30 years old).
Table 1 shows the demographic characteristics of the soldiers surveyed, as well as the response rates to the TICS questions and the rates of TICS positive screens. Of the 6,527 respondents, 5,842 (90%) answered both TICS questions. Response rates for the alcohol behavior questions ranged from 90% to 94%, with 95% of participants responding to at least one of the questions. Rates of yes responses ranged from 1% (DUI) to 16% (drinking and driving) (
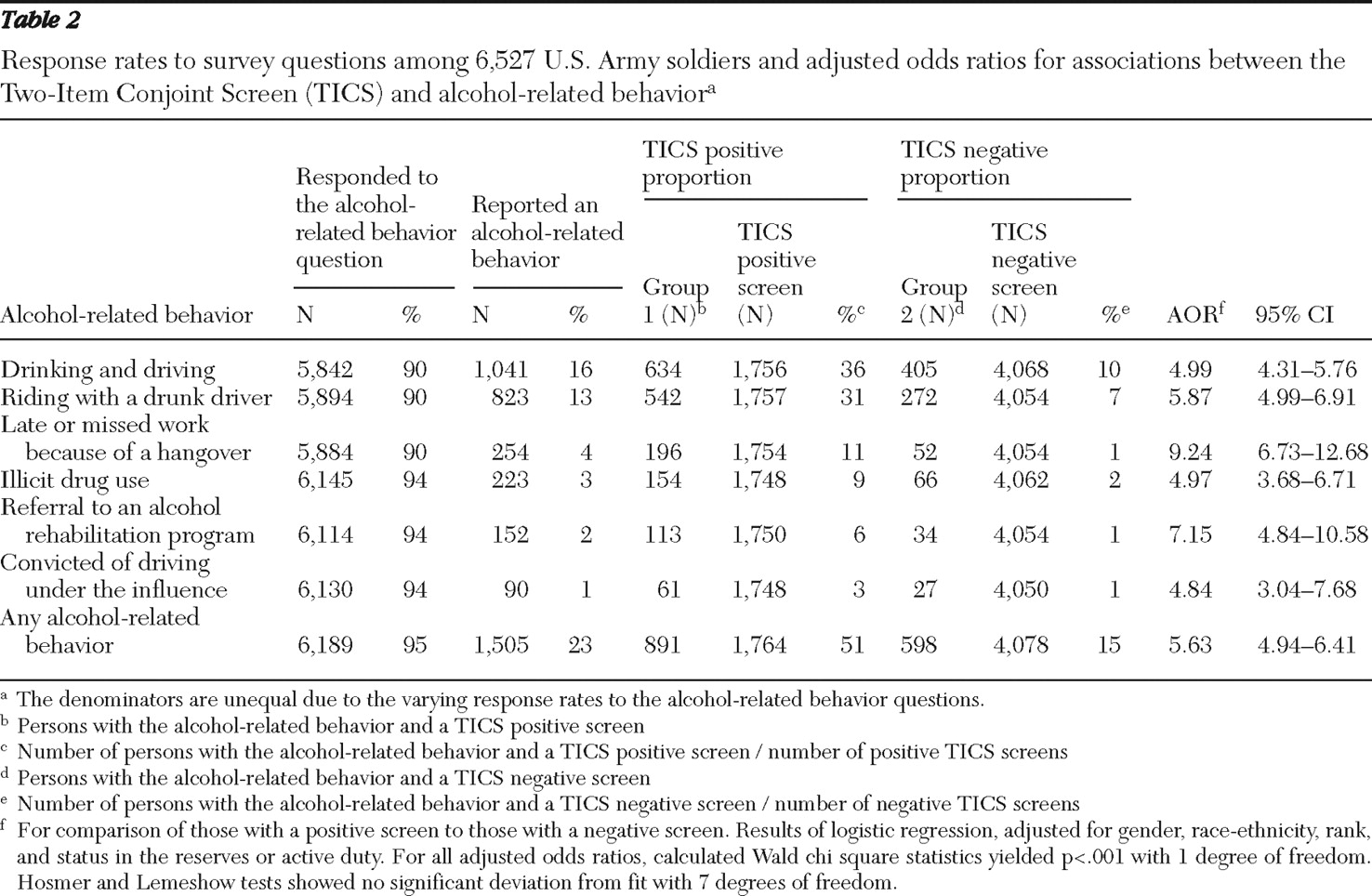
Table 2 ).
Answering yes to at least one of the TICS questions was strongly associated with answering yes to the alcohol-related behavior questions (
Table 2 ). Drinking and driving was the most frequently reported behavior. DUI convictions and referral to alcohol rehabilitation were the least frequently reported. Soldiers who scored positive on the TICS were five to nine times as likely to report alcohol-related behaviors, compared with those who screened negative.
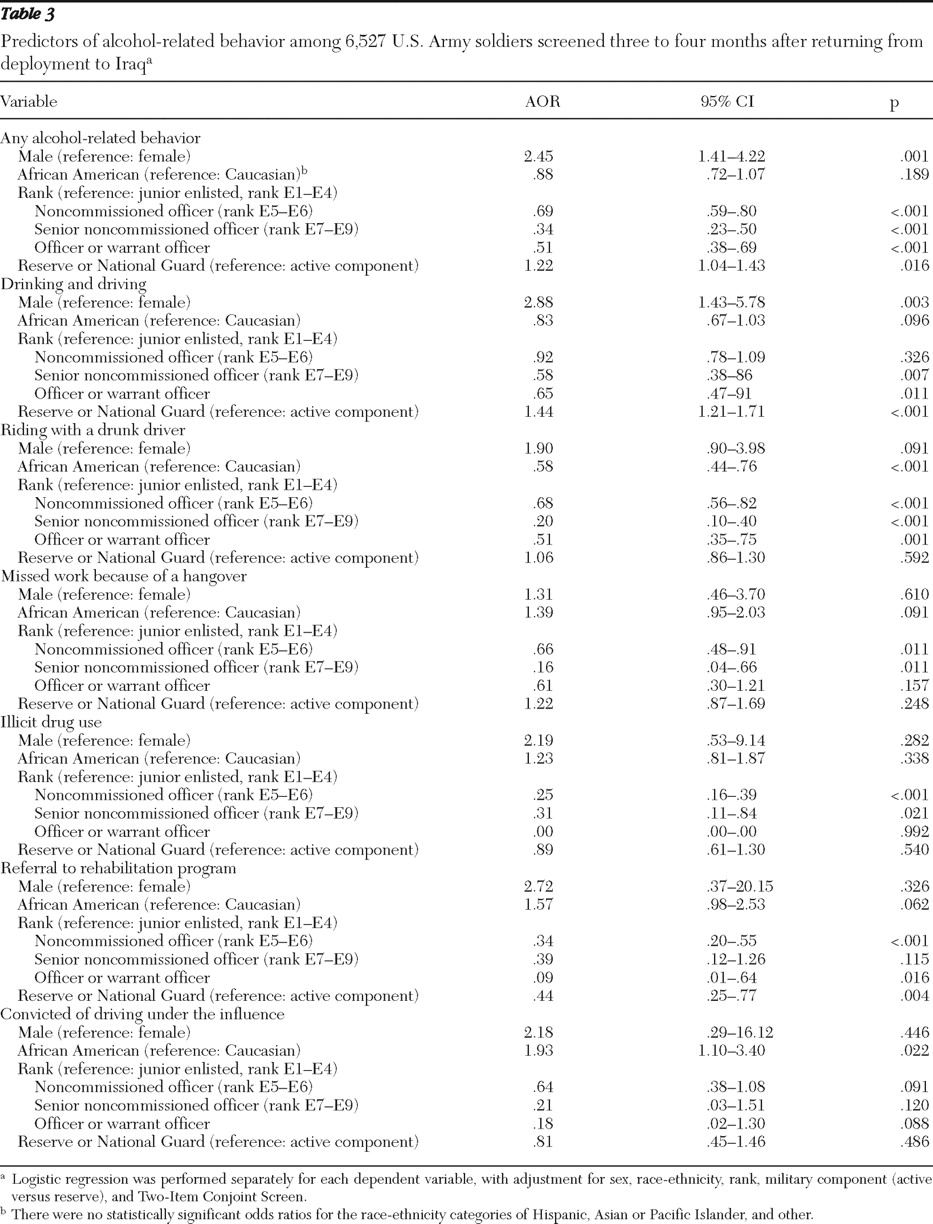
Other findings from the logistic regression are reported in
Table 3 . Compared with women, men were more than twice as likely to report at least one alcohol-related behavior (OR=2.45, p=.001) and to report drinking and driving (OR=2.88, p=.003). Compared with Caucasians, African Americans were almost half as likely to report riding with a driver who had been drinking (OR=.58, p<.001) but nearly twice as likely to report a DUI conviction in the previous year (OR=1.93, p=.022). Compared with junior enlisted service members (rank E1–E4), senior noncommissioned officers (rank E7–E9) and officers were less likely to report any alcohol-related behavior (OR=.34, and OR=.51, respectively, p<.001 for both). Compared with active duty soldiers, soldiers in the reserves or the National Guard had higher odds of drinking and driving (OR=1.44, p<.001) but lower odds of having entered a substance abuse treatment program (OR=.44, p=.004).
Regression analyses also revealed that with higher combat exposure intensity, the odds of a TICS positive screen increased. Compared with soldiers in the lowest quartile of combat experience, those in the third quartile had 44% higher odds of having a TICS positive screen, (OR=1.44, 95% confidence interval [CI]=1.20–1.72, p<.001) and those in the fourth quartile had 93% higher odds of screening positive (OR=1.93, CI=1.63–2.29, p<.001). Finally, compared with those screening negative on the TICS, those screening positive were 2.5 times as likely to also screen positive for depression, generalized anxiety, or PTSD symptoms (OR=2.5, CI=2.15–2.83, p<.001).
Discussion
We examined the use of the modified TICS in postdeployment health screening and found that the TICS correlated strongly with high-risk drinking behaviors that have a significant negative impact not only on an individual's health and well-being but also on his or her occupational functioning. Behaviors such as missing work because of a hangover, going to work intoxicated, using illicit drugs, or receiving DUI convictions impede a person's ability to maintain a high level of functioning in any occupational setting, including the military.
Despite the negative stigma attached to alcohol abuse and dependence, 10% to 15% of soldiers were willing to endorse at least one of the TICS questions nonanonymously on a PDHRA screening after returning from combat duty in Iraq (
12 ). The anonymous study presented here shows approximately double that rate (27%). Despite this, referrals to alcohol rehabilitation programs as a direct result of the postdeployment screening appear to be very rare. Of 56,350 soldiers who received the PDHRA screening, 6,669 (12%) reported alcohol misuse, yet only 134 soldiers (.2%) were referred for treatment (
12 ). By confirming the utility of the DoD screening instrument in predicting high-risk alcohol-related behaviors, our study brings to light the need to increase such referral rates. In the military, the lack of confidentiality regarding alcohol treatment likely serves as a barrier to care, leading not only to low referral rates but also to reduced self-reporting of alcohol misuse.
The U.S. military has shown itself capable of reducing nicotine and illicit drug use and abuse in the past, while falling short in similarly reducing alcohol consumption (
19 ). Removing the potentially career-stigmatizing involvement of a soldier's commanding officer in early intervention will likely remove the main obstacle holding back any public health benefits that mass population screening may yield. Unit leaders could still be involved in ensuring that soldiers who have exhibited serious alcohol-related behaviors receive treatment. However, a parallel program should also be in place to ensure that soldiers identified through health screening processes can receive confidential referral and treatment for alcohol problems with the same level of protections afforded to those with other mental disorders.
It becomes clear from examining the results of the logistic regression more closely that efforts to address high-risk alcohol-related behavior may benefit from targeted interventions. Interventions may be different for men than for women and for junior enlisted than for noncommissioned officers or for officers. Military units that have engaged in high combat would benefit from more specific screening and education regarding alcohol use postdeployment.
The findings from this study also suggest that there are unique issues with access to alcohol treatment for the National Guard and the reserve component. The findings showed that compared with active component soldiers, reserve component soldiers had a similar overall rate of alcohol misuse but 44% higher odds of drinking and driving, along with a 56% lower odds of entering treatment. These differences may be due to the fact that active component soldiers have better access to substance abuse rehabilitation programs on base, as well as a leadership structure that is trained to quickly intervene when a soldier is having difficulties in occupational functioning (
20 ). The findings suggest a need to evaluate the availability of alcohol treatment programs for reserve component soldiers and to ensure high-quality screening for alcohol misuse upon entering the VA health care system. Of note, the National Guard and reserve components, although frequently grouped together for analysis, are in fact distinct. This study was not powered to analyze the two separately, but one should be aware that these differences could have implications in public health interventions to address alcohol misuse. What they both have in common is that after overseas deployments, these soldiers return to their hometowns and do not have the kinds of services regularly available to active duty soldiers on base.
Increases in alcohol use after deployment represent only one part of the behavioral health issues that troops face after war, and an association between PTSD and increased alcohol use has been demonstrated (for example, in the National Comorbidity Study) (
21 ). Our study showed that service members who screened positive for alcohol misuse in this study had 2.5 times the odds of screening positive for depression, PTSD, or generalized anxiety. The high incidence of PTSD resulting from war zone exposures and the high comorbidity of PTSD and alcohol misuse highlight the urgent need to ensure parity of access to care.
The main limitation of this study is its basis on self-reported data. However, response rates were high, few respondents elected not to answer the alcohol questions, and availability for the study was largely a product of unit training schedules. It is likely that the study sample overrepresented healthy, working soldiers because the seriously wounded soldiers or those attending medical appointments on the days of the survey (including appointments in command-directed substance abuse programs) would not have been available to participate. Additionally, soldiers who were discharged from the Army in the three months after return from deployment because of medical problems, misconduct, illicit drug use, alcohol abuse, or other reasons were not included in this study. If these were the responses from the healthiest segment of the population, then the results reflect more conservative outcomes than would be observed in the entire population.
Self-report screening measures of alcohol misuse cannot be assumed to reflect alcohol abuse or dependence and should only be used to identify individuals in need of more comprehensive clinical evaluation. The cross-sectional study methods preclude drawing definitive conclusions about causality, and direct estimates of the risk of alcohol-related behaviors cannot be made using ORs. However, the consistency and strength of the associations support the conclusions and policy implications of this study.
Responses to the alcohol screening are likely affected by the context in which they are utilized, with evidence that anonymous assessments yield higher rates of positive screens than nonanonymous ones. In a setting where there is an expectation of medical confidentiality, there is likely to be more willingness to discuss alcohol-related behaviors, compared with screening processes that might result in the involvement of one's supervisor. Although it is not possible to generalize these results beyond this military population, the TICS was originally shown effective in a civilian setting, and it is likely that the questions would have relevance to other occupational settings.
Conclusions
The association of alcohol misuse with combat experiences provides a likely explanation for increased rates of alcohol use observed after deployment. However, further research is required to better understand which types of combat experiences confer greater risk and whether there are specific groups that can be targeted for intervention. Given the tremendous stigma of mental health problems, a simple screening for alcohol misuse reveals not only who would potentially benefit from early interventions to decrease these serious alcohol-related behaviors but also who might benefit from a less stigmatizing entry into mental health services for symptoms related to combat and operational stress responses. Screening for alcohol misuse is likely to enhance the overall effectiveness of screening for other mental health problems. Ultimately, however, the potential utility of screening hinges on providing a structure of care that facilitates access to confidential and nonstigmatizing forms of treatment.
Acknowledgments and disclosures
The authors are indebted to the soldiers for their participation and service; without these soldiers these analyses would not have been possible. The authors also thank the leadership of the units that were studied, Cara H. Olsen, M.S., Dr.P.H., at the Uniformed Services University of the Health Sciences for guidance on statistics concepts and software and Robert J. Ursano, M.D., for his support and insight. The views expressed in this article are those of the authors and do not reflect official policy or position of the Department of the Army, the Department of the Navy, the Department of Defense, the U.S. Government, or any of the institutional affiliations listed.
The authors report no competing interests.