Clinical experience suggests that individuals with borderline personality disorder commonly report being in psychotherapy and taking standing psychotropic medications (that is, medications taken on a regular basis) over substantial periods of time. Patients with borderline personality disorder are also frequently rehospitalized. However, only two longitudinal studies have prospectively examined the long-term course of psychiatric treatment received by these patients.
In the first of these studies, treatment utilization by patients with borderline personality disorder and by a comparison group of patients with other axis II disorders was studied in a six-year prospective follow-up study, the McLean Study of Adult Development (MSAD) (
1 ). Prevalence rates of individual therapy, standing medication, and psychiatric hospitalization declined significantly in both groups but remained significantly higher among patients with borderline personality disorder. Perhaps most striking was the finding that 70% of patients with borderline personality disorder participated in individual therapy and 70% took standing medications in all three follow-up periods.
In the second longitudinal study—the Collaborative Longitudinal Personality Disorders Study—treatment use over three years by patients with borderline personality disorder was compared with that of patients who had major depressive disorder but no personality disorder (
2 ). Patients with borderline personality disorder were significantly more likely than those with major depressive disorder to be in individual therapy, to have had a medication consultation, and to have been hospitalized for psychiatric reasons.
The study reported here, which is an extension of MSAD, had two purposes. The first was to describe over ten years of prospective follow-up the rates of use of three key treatment modalities reported by a large and well-defined sample of patients with borderline personality disorder and by patients with axis II disorders in a comparison group. The second purpose was to determine time to cessation and time to resumption of the three forms of treatment among patients with borderline personality disorder.
Methods
Sample
The methodology of this study has been described in detail elsewhere (
3 ). The study was approved by the McLean Hospital Institutional Review Board. Written informed consent was obtained from each participant after careful explanation of what the study involved and before any study procedures were administered.
All participants were inpatients at McLean Hospital in Belmont, Massachusetts, who were admitted and interviewed between 1992 and 1995. Each patient was first screened to determine that he or she fulfilled several inclusion criteria. Participants had to be between the ages of 18 and 35; have a known or estimated IQ of 71 or higher; have no history or current symptoms of schizophrenia, schizoaffective disorder, bipolar I disorder, or an organic condition that could cause psychiatric symptoms; and be fluent in English.
Procedures
Each patient met with a master's-level interviewer blind to the patient's clinical diagnoses for a thorough diagnostic assessment. Three semistructured diagnostic interviews were administered—the Structured Clinical Interview for DSM-III-R Axis I Disorders (
4 ), the Revised Diagnostic Interview for Borderlines (DIB-R) (
5 ), and the Diagnostic Interview for DSM-III-R Personality Disorders (DIPD-R) (
6 ). The interrater and test-retest reliability of all three measures have been found to be good to excellent (
7,
8 ).
Treatment history was assessed with the Background Information Schedule (BIS), a semistructured interview designed to assess the psychosocial functioning and treatment history of patients with borderline personality disorder and patients with other axis II disorders. The interrater and test-retest reliability and the concurrent validity of the BIS have been found to be good to excellent (
9 ).
At each of five follow-up waves, separated by 24 months, use of psychiatric treatment was reassessed by staff members blind to baseline diagnoses using interview methods similar to the baseline procedures. After informed consent was obtained, the follow-up analog to the BIS was administered—the Revised Borderline Follow-Up Interview. Follow-up interrater reliability (within one generation of follow-up raters) and follow-up longitudinal reliability (from one generation of raters to the next) were also found to be good to excellent for this interview (
1 ).
Statistical methods
Generalized estimating equations, with diagnosis and time as main effects, were used in longitudinal analyses of prevalence data. Tests of diagnosis-by-time interactions were conducted. These analyses modeled the log prevalence, yielding an adjusted relative risk ratio (RRR) and 95% confidence interval for diagnosis and time. Gender was also included in these analyses as a covariate because patients in the group with borderline personality disorder were significantly more likely to be female than those in the comparison group. Alpha was set at .05, two-tailed.
The Kaplan-Meier product-limit estimator (of the survival function) was used to assess the time to cessation of treatment and time to resumption of treatment for the three treatments studied: individual therapy, standing medication, and psychiatric hospitalization. For each modality, we defined time to cessation of treatment as the time until the interview at which cessation of the treatment was first reported. Possible values for this outcome were two, four, six, eight, or ten years. For example, time to cessation for a person who was in individual therapy at baseline and who first reported stopping therapy at the two-year interview was two years (even though the patient may have resumed and then stopped therapy during subsequent intervals). We defined time to resumption of treatment in a somewhat different manner—the number of years after a person had stopped a treatment that he or she resumed that treatment. Thus times for this outcome were two, four, six, or eight years after the first report of cessation of a given treatment.
Results
Baseline sample description
A total of 290 patients met both DIB-R and DSM-III-R criteria for borderline personality disorder; 72 met DSM-III-R criteria for at least one axis II disorder other than borderline personality disorder (and neither set of criteria for borderline personality disorder). Of these 72 comparison participants, three (4%) met DSM-III-R criteria for an odd cluster personality disorder, 24 (33%) met DSM-III-R criteria for an anxious cluster personality disorder, 13 (18%) met DSM-III-R criteria for a dramatic cluster personality disorder, and 38 (53%) met DSM-III-R criteria for personality disorder not otherwise specified (operationally defined in the DIPD-R as meeting all but one of the required number of criteria for at least two of the 13 axis II disorders described in DSM-III-R ).
Baseline demographic data have been reported elsewhere (3). Briefly, 279 participants (77%) were female, and 315 (87%) were white, 20 (6%) were African American, nine (3%) were Hispanic, eight (2%) were Asian, and ten (3%) were biracial or of other racial or ethnic backgrounds. The mean±SD age of the participants was 27.0±6.3 years, the mean socioeconomic status was 3.3±1.5) (range of 1 to 5, with 5 indicating the lowest status) (10), and the mean Global Assessment of Functioning score was 39.8±7.8 (indicating major impairment in several areas, such as work or school, family relations, judgment, thinking, or mood).
A total of 309 of the surviving patients (90%) were reinterviewed at all five follow-up waves. More specifically, 249 (92%) of the 271 surviving patients with borderline personality disorder and 60 (85%) of the 71 surviving patients in the comparison group were evaluated six times (baseline and five follow-ups).
Mental health service use
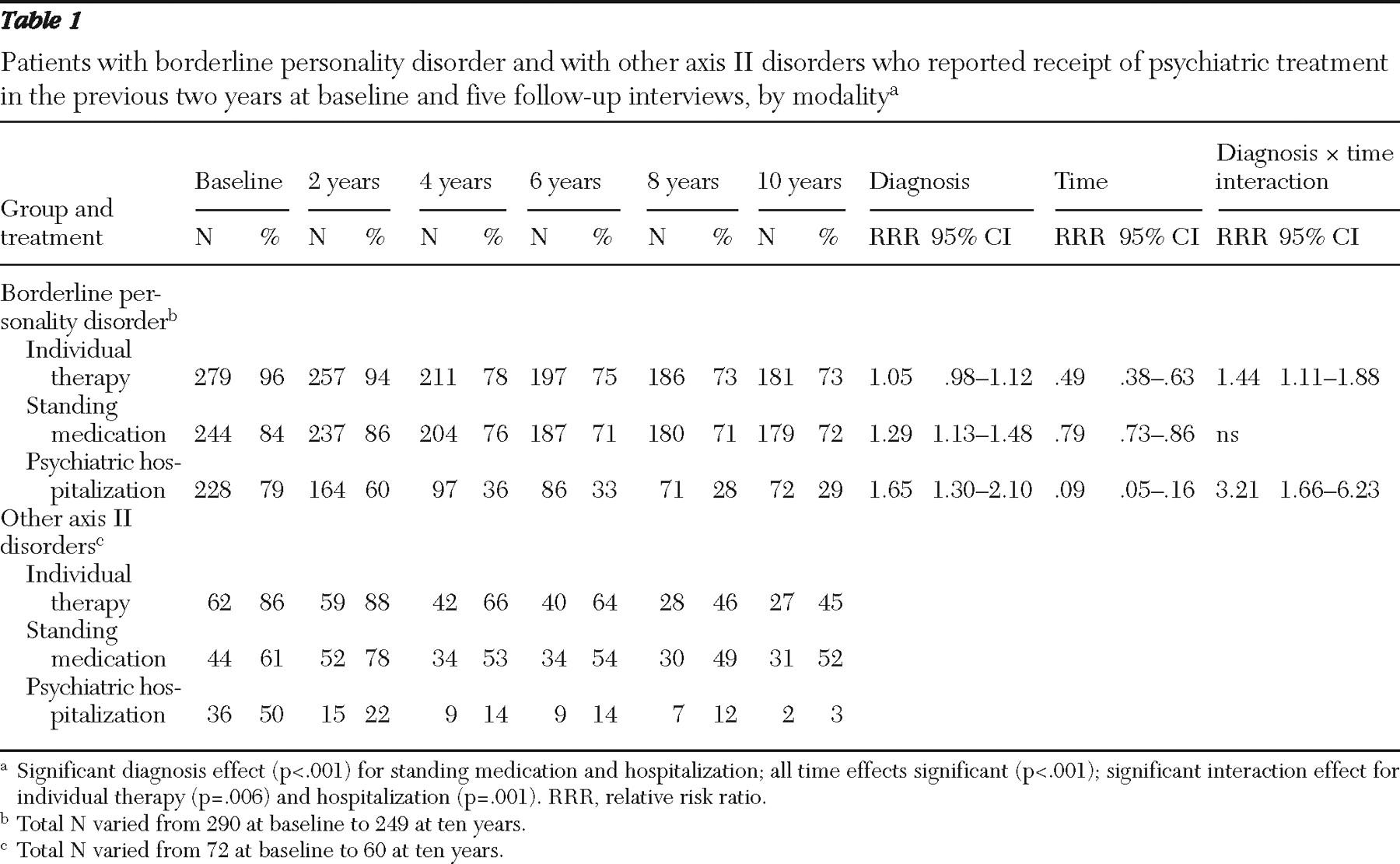
Table 1 presents prevalence data on use of the three treatment modalities by the two patient groups over ten years. A significantly higher percentage of patients with borderline personality disorder reported taking standing medications over the ten-year period (relative risk ratio [RRR]=1.29, or 29% higher). When all patients were considered together, the proportion of patients taking psychotropic medications declined significantly over time, with a relative decrease from baseline of 21% ([1–.79]×100=21).
However, significant interactions between diagnosis and time were found for individual therapy and psychiatric hospitalization, and the explanation of these results is more complicated. At baseline 96% of patients with borderline personality disorder and 86% of those in the comparison group reported that they were in individual therapy. At the ten-year follow-up, rates had declined to 73% and 45%, respectively. For patients in the comparison group, the likelihood of participating in individual therapy decreased by 51% from baseline to ten years (RRR for diagnosis=.49; [1–.49]×100=51). The significant interaction between diagnosis and time indicates that the decline over ten years for patients with borderline personality disorder was 29% ([1–.49×1.44]×100=29). Thus the rate of decline was significantly smaller for patients with borderline personality disorder than for those in the comparison group (29% compared with 51%).
Among patients with borderline personality disorder, 79% reported having been hospitalized before the baseline interview, compared with 50% of those in the comparison group. At the ten-year follow-up, 29% and 3%, respectively, of the groups reported hospitalization in the prior two years. At baseline patients with borderline personality disorder were 65% more likely to report prior hospitalization (RRR=1.65). For patients in the comparison group, the likelihood of being hospitalized over the ten-year period decreased by 91% (RRR=.09). The significant interaction between diagnosis and time indicates that the ten-year decline for patients with borderline personality disorder was 71% ([1–.09×3.21)×100%=71). Thus the rate of decline was significantly smaller for patients with borderline personality disorder than for those in the comparison group (71% compared with 91%).
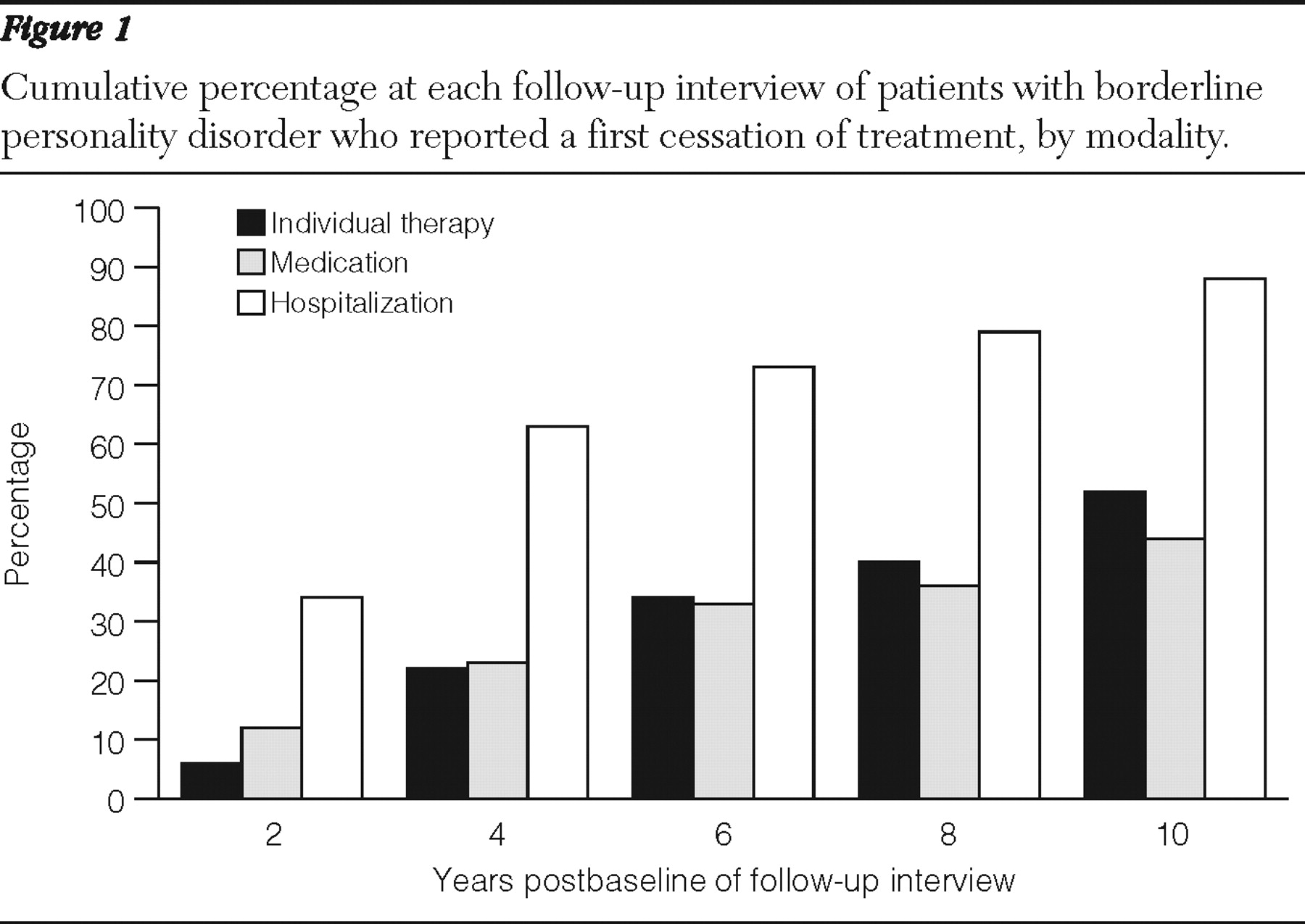
Figure 1 shows the cumulative percentage at each follow-up interview of patients with borderline personality disorder who reported a first cessation of treatment in each modality. Of those who reported receipt of individual therapy in the two years before baseline, 52% (N=84) had reported ceasing therapy at least once by ten years. Of those who were taking standing medication at baseline, 44% (N=89) had reported ceasing psychopharmacology at least once by ten years. All 290 patients with borderline personality disorder were hospitalized at baseline. At ten years, 88% (N=178) had experienced at least one two-year period without a psychiatric hospitalization. (Rates of treatment cessation cannot be determined using the numbers in this paragraph because of censoring—that is, participants lost to follow-up because of death or because they declined to participate.)
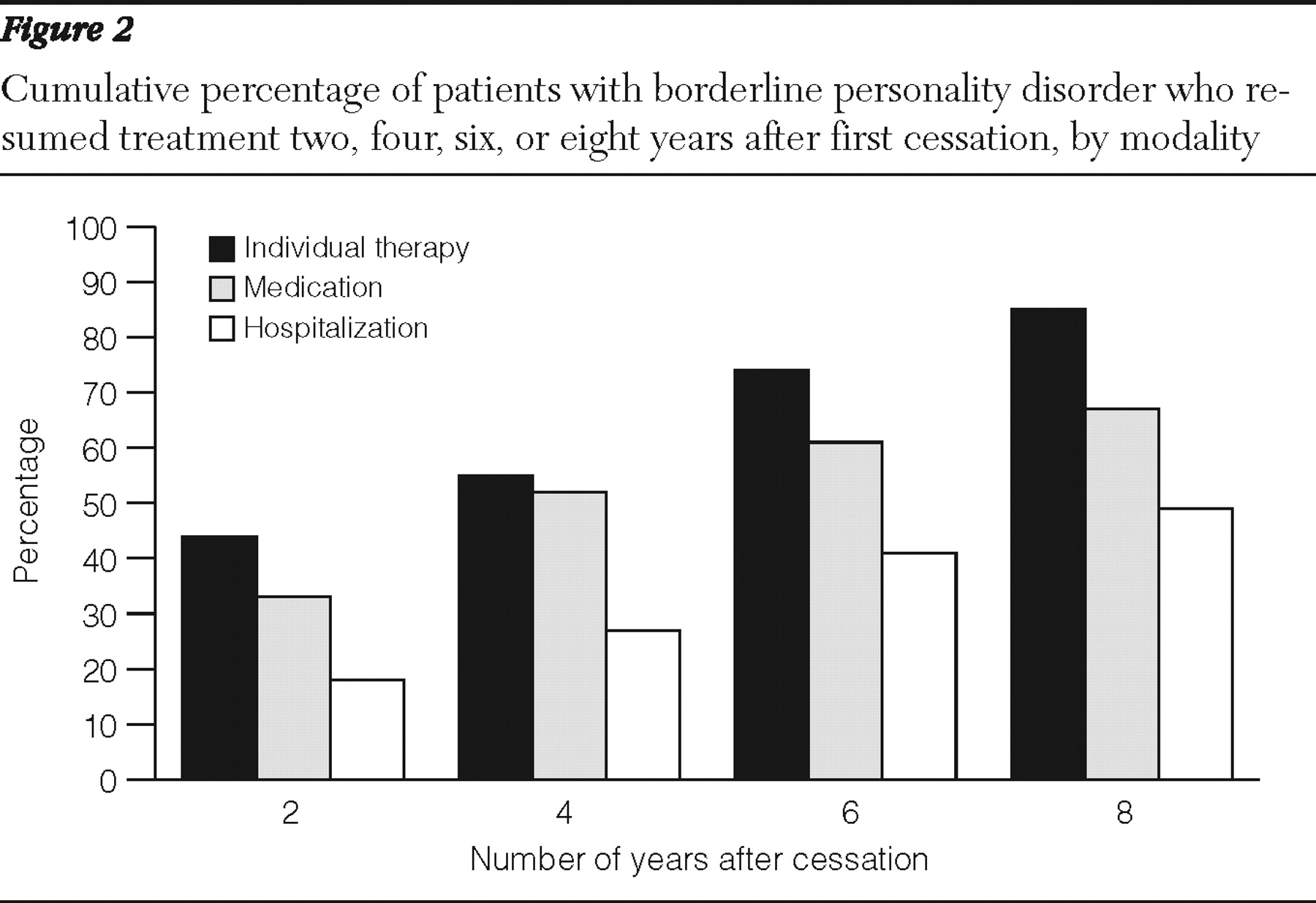
Figure 2 shows the time to resumption for each treatment among patients with borderline personality disorder after they reported a first cessation of that treatment. The ten-year data indicate that of those who reported cessation of individual therapy, 85% (N=62) resumed therapy during a subsequent follow-up period. Of those who reported having stopped taking standing medication, 67% (N=44) resumed during a subsequent follow-up period. In addition, 49% (N=59) of patients who had not been hospitalized for at least one of the two-year follow-up periods had been rehospitalized by the ten-year follow-up. (Rates of treatment resumption cannot be determined using the numbers in this paragraph because of censoring—that is, participants lost to follow-up because of death or because they declined to participate.)
Discussion
Four main findings emerged from this study. The first is that the prevalence of use of each treatment modality declined significantly over time for patients with borderline personality disorder. Specifically, for patients with borderline personality disorder, use of individual therapy declined 29%, use of standing medication declined 21%, and use of psychiatric hospitalizations declined 71%. These findings are consistent with and extend the findings of our six-year follow-up study of this sample (
1 ).
The second finding is that both use of standing medication and psychiatric hospitalization (but not individual therapy) were significantly more common among patients with borderline personality disorder than among patients in the comparison group. More specifically, at baseline patients with borderline personality disorder were 29% more likely to be taking standing medication and 65% more likely to report a prior hospitalization for psychiatric reasons; however, they were only 5% more likely to be in individual therapy at baseline. These findings are also consistent with and extend the findings of our six-year follow-up study of this sample (
1 ).
The third finding is that about half the patients with borderline personality disorder who were in individual psychotherapy or taking standing medication at baseline reported having stopped these outpatient treatments at least once by the time of the ten-year follow-up. In addition, nearly 90% of patients with borderline personality disorder reported not having been rehospitalized for at least one two-year period. This is a new finding and seems to demonstrate a specific pattern in the long-term treatment of patients with borderline personality disorder: more continuous use of outpatient treatment and a decline in inpatient treatment. It is interesting that the major decline in the two outpatient treatments took place by the fourth year after the index hospitalization and then remained rather stable throughout the remaining six years of follow-up.
The fourth finding is that for each modality, resumption of treatment after termination was common among patients with borderline personality disorder. Specifically, 85% of the patients who terminated individual therapy later resumed it, and 67% of the patients who had stopped using standing medications later resumed psychopharmacological treatment. In addition, 49% of those who reported no hospitalization for a period of at least two years were later rehospitalized. This set of findings is also new and is consistent with the prior finding that outpatient treatment modalities are used more consistently than inpatient treatment. It is not clear why resumption of outpatient treatment is so common. It might be attributable to residual borderline symptoms, ongoing axis I disorders, psychosocial dysfunction, or some combination of these factors.
Almost none of the patients with borderline personality disorder in this study had ever received treatment specifically designed for individuals with this disorder. It is not possible to determine whether the results of the study would have been different if a substantial percentage of those with borderline personality disorder had participated in one of the psychotherapeutic approaches specifically developed for this disorder—dialectical behavioral treatment (
11 ), mentalization-based treatment (
12 ), transference-focused psychotherapy (
13 ), and schema-focused therapy (
14 ).
This study had two main limitations. All participants were seriously ill inpatients at the start of the study. Thus it is difficult to know whether the results would generalize to a less disturbed group of patients with borderline personality disorder. Also, most of the information on treatment history was based on self-report. However, we were able to use the hospital's electronic medical record system to validate the number and length of inpatient stays for patients hospitalized at McLean Hospital.
Conclusions
The results suggest that patients with borderline personality disorder tend to use outpatient treatment without interruption over prolonged periods. They also suggest that inpatient treatment is used far more intermittently and by a relatively small minority of patients with borderline personality disorder.
Acknowledgments and disclosures
This study was supported by the Fellowship Persönlichkeitsstörungen by the Gesellschaft zur Erforschung und Therapie von Persönlichkeitsstörungen e.V. and the Asklepios Kliniken Hamburg GmbH and by grants MH47588 and MH62169 from the National Institute of Mental Health.
The authors report no competing interests.