Emergency department utilization has risen considerably. According to the National Hospital Ambulatory Medical Care Survey (NHAMCS), from 1996 to 2006 the total number of emergency department visits increased by 32% and the population-based emergency department use rate increased by 18% (
1 ). The number of emergency department visits for psychiatric reasons has also been growing and constitutes 5.4% of all emergency department visits by adults (
2 ).
Emergency departments provide essential and unique services. However, high emergency department use may in part reflect crises that could be averted or better addressed with effective outpatient treatment and coordination. Interventions to improve medication adherence, for example, can reduce emergency department use (
3 ). It is important to give attention to both psychiatric and general medical emergency department use for persons with major mental disorders, who are likely to have high need in both domains. In prior research on emergency department use in a treatment sample with serious mental illness, 37% reported emergency department utilization for somatic problems (
4 ). There is evidence that persons with serious mental illness may have more difficulty with access to or quality of medical care (
5,
6 ). They may, therefore, be more likely to use the emergency department as their de facto medical care point of contact. Furthermore, the high prevalence of co-occurring substance use disorders and unmet need among persons with serious mental illness (
7 ) suggests the possibility of higher emergency department use.
Within Medicare, the two major eligibility groups—persons younger than 65 years who were Medicare eligible because of a disability (disabled beneficiaries) and persons who are aged 65 years or older (aged beneficiaries)—present high levels of general health and mental health needs. Among aged Medicare beneficiaries with chronic medical illness, a depression diagnosis doubles the likelihood of emergency department use (
8 ). Yet nationally representative studies of emergency department use among Medicare beneficiaries with major mental health disorders are lacking.
In this descriptive study, nationally representative Medicare claims data from 2004 were used to examine emergency department utilization for beneficiaries with serious mental disorders. Two primary research questions were examined. First, among Medicare beneficiaries with serious mental disorders, does emergency department utilization vary by mental health diagnostic category? Second, among Medicare beneficiaries with serious mental disorders, is the presence of a claim related to substance use disorder (substance-related claim) during the year associated with greater emergency department utilization?
The findings from this retrospective analysis of secondary data will inform our understanding of treatment patterns for this population and will point to where further attention may be warranted in terms of additional research and treatment system improvements.
Methods
The study used claims and eligibility data (Standard Analytic Files) from a random 5% sample of the 2004 national survey of disabled and aged Medicare beneficiaries. The sample consisted of 129,805 fee-for-service beneficiaries whose most frequent primary psychiatric diagnosis during the year was in one of four mutually exclusive categories: schizophrenia ( ICD-9 code 295), major depressive disorder ( ICD-9 codes 296.2 and 296.3), other affective psychoses (largely bipolar disorder; ICD-9 codes 296.0, 296.1, and 296.4–296.99), or selected other psychoses in the ICD-9 rubric ( ICD-9 codes 293, 294, and 297–299, including conditions such as paranoid states and some organic psychoses but excluding 290-series codes for primary dementia).
Emergency department visits were identified by place of service, revenue codes, and Current Procedural Terminology (CPT) codes. Measures included dichotomous variables indicating any emergency department visit or any emergency department visit with a primary psychiatric diagnosis ( ICD-9 codes 293–302, 306–314, and 316), as well as mean number of emergency department visits. For emergency department visits resulting in hospitalization, inpatient primary diagnosis was used to assign a primary diagnosis. Chi square tests and F tests were used to compare utilization by other mental health diagnostic category and presence of primary substance abuse diagnosis or selected substance-related codes on any claim during the year ( ICD-9 codes 291, 292, and 303–305, plus selected substance-related codes—for example, ICD-9 code 648.3, drug dependence in pregnancy). We also examined the percentage of emergency department visits that were identified through inpatient claims, indicating that the visit was followed by a hospital admission.
Human subject protections were ensured by the federal funding agency and its primary contractor through which these analyses were conducted. The study was considered exempt from institutional review board review.
Results
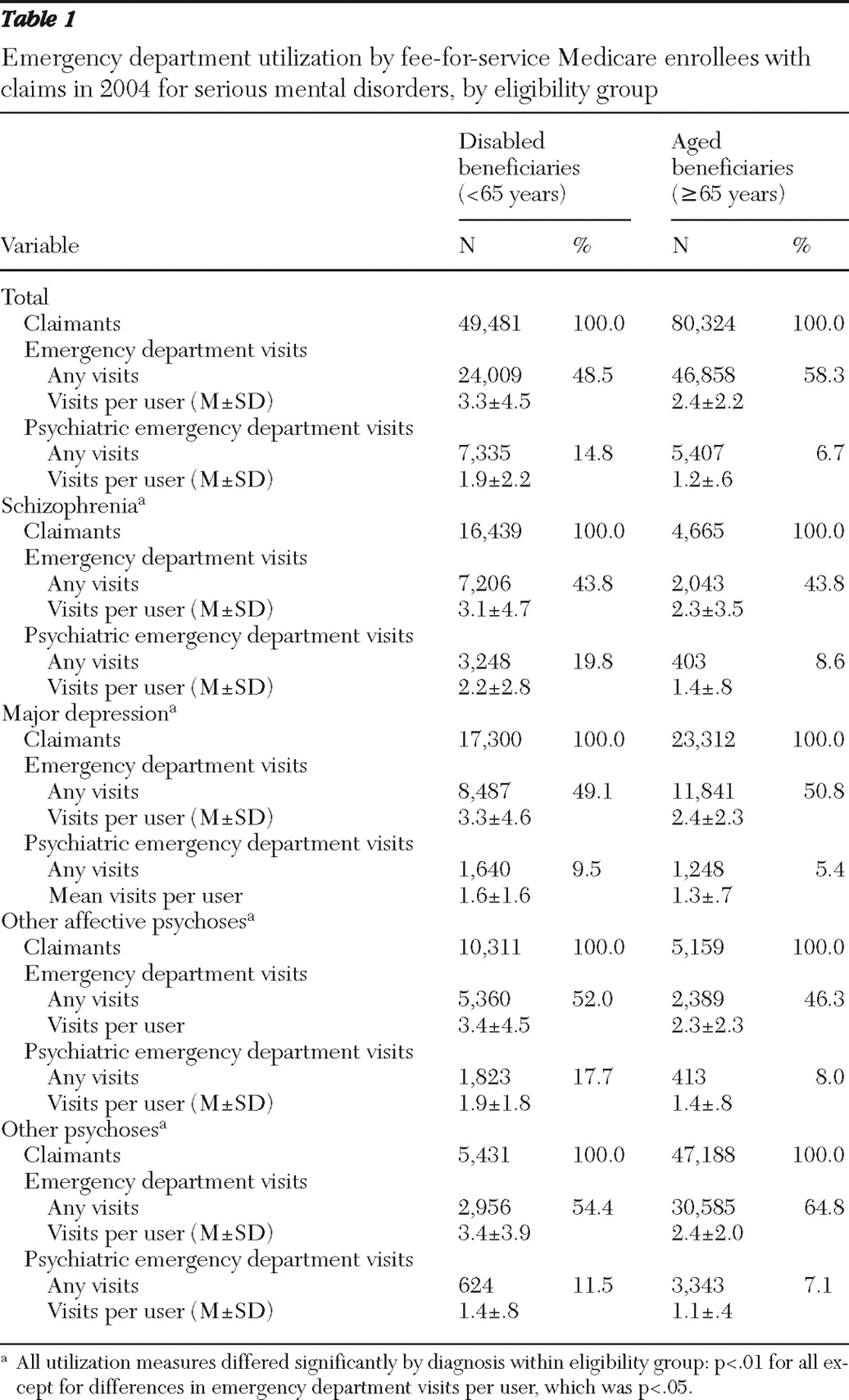
The subsample of disabled beneficiaries (N=129,805) had a mean±SD age of 46.7±9.9 years, and 50.8% (N=25,114 of 49,481) were women. Women accounted for 67.6% (N=54,297 of 80,324) of the aged beneficiaries, who had a mean age of 78.7±8.4 years. The proportion of the sample in each diagnostic category varied for disabled and aged beneficiaries (
Table 1 ).
As shown in
Table 1, 48.5% of disabled beneficiaries had at least one emergency department visit during the year, with an average of 3.3 visits per user; 14.8% had a psychiatric emergency department visit, averaging 1.9 visits per user. Among aged beneficiaries, 58.3% had at least one emergency department visit during the year, averaging 2.4 visits per user. Among these aged beneficiaries, 6.7% had a psychiatric emergency department visit, averaging 1.2 visits per user. Emergency department visits per 100 beneficiaries—a population-level calculation that incorporates both the proportion of beneficiaries with any emergency department visits and the number of visits per user—totaled 158 for disabled beneficiaries and 138 for aged beneficiaries (data not shown).
Among disabled beneficiaries, all utilization measures (percentage with any emergency department visits, percentage with any psychiatric emergency department visits, mean number of emergency department visits per user, and mean number of psychiatric emergency department visits per user) varied significantly by psychiatric diagnosis (p<.01 for all utilization measures, except for the mean number of psychiatric emergency department visits per user, which was p<.05.). The percentage of disabled beneficiaries with a psychiatric emergency department visit ranged from 9.5% (major depression) to 19.8% (schizophrenia). The patterns among aged beneficiaries were similar, although utilization was lower overall. All utilization measures varied significantly by mental health diagnosis for aged beneficiaries (p<.01 for all utilization measures, except for the mean number of psychiatric emergency department visits per user, which was p<.05). The percentage of aged beneficiaries with any psychiatric emergency department use ranged from 5.4% (major depression) to 8.6% (schizophrenia).
Disabled beneficiaries were more likely than aged beneficiaries to have a substance-related claim during the year (N=4,335, 8.8%, versus N=1,904, 2.4%) (data not shown in table). In both groups, persons with substance-related claims were far more likely to have any emergency department and psychiatric emergency department visits. Among disabled beneficiaries, 82.4% (N=3,574 of 4,335) of those with a substance-related claim had an emergency department visit, compared with 45.3% (N=20,435 of 45,146) of those without a substance-related claim (p<.01). Thirty-seven percent (N=1,602) of disabled beneficiaries with a substance-related claim had a psychiatric emergency department visit, compared with 12.7% (N=5,734) of those without (p<.01). For aged beneficiaries, somewhat smaller but still major increases in emergency department use occurred for those with a substance-related claim (N=1,591 of 1,904, or 83.6%, versus N=45,264 of 78,420, or 57.7%, for any emergency department visits and N=263 of 1,904, or 13.8%, versus N=5,144 of 78,420, or 6.6%, for psychiatric emergency department visits; p<.01 for both).
For disabled beneficiaries, 26.5% of all emergency department visits (N=20,710 of 78,146) and 46.9% of psychiatric emergency department visits (N=6,575 of 14,033) were identified from inpatient claims, indicating that the visit resulted in admission (data not shown in table). This pattern was consistent across schizophrenia (N=5,929 of 22,529, or 26.3%, for all emergency department visits and N=3,387 of 7,108, or 47.7% for psychiatric department visits), major depression (N=7,225 of 27,646, 26.1%, and N=1,338 of 2,701, 49.5%), and other affective psychoses (N=3,905 of 17,956, 21.7%, and N=1,552 of 3,380, 45.9%). For the selected other psychoses category, about one-third of any emergency department visits (N=3,651 of 10,015, 36.5%) and psychiatric emergency department visits (N=298 of 844, 35.3%) resulted in inpatient admission. For aged beneficiaries, 50.5% (N=55,962 of 110,841) of all emergency department visits and 44.6% (N=2,836 of 6,363) of psychiatric emergency department visits were identified from inpatient claims, indicating admission. Rates of inpatient admission for all emergency department visits ranged from 41.9% (N=1,946 of 4,645) (schizophrenia) to 52.0% (N=37,854 of 72,769) (selected other psychoses), and rates of inpatient admission for psychiatric emergency department visits ranged from 35.6% (N=1,303 of 3,655) (selected other psychoses) to 58.9% (N=337 of 572) (other affective psychoses).
Discussion
The results show that total emergency department use—for general medical and psychiatric reasons—is very common for Medicare beneficiaries with serious mental disorders. Compared with NHAMCS estimates of 48 visits per 100 persons with Medicare (
1 ), in our Medicare sample total emergency department use was much higher for both disabled and aged beneficiaries (158 and 138, respectively). There are important differences between the NHAMCS and our analysis, other than our focus on persons with serious mental illness. The NHAMCS, a national probability sample survey of nonfederal, general, and short-stay hospitals, has a four-stage sampling design that ultimately selects a sample of patient visits for which hospital staff complete a patient record form, including clinical data and type of insurance. However, this comparison may be contextually informative.
In populations with high levels of morbidity, emergent needs inevitably arise. The study findings do not identify whether emergency department utilization was necessary or appropriate. However, extensive emergency department use raises concern about potential issues regarding access to care and quality or continuity of care. Treatment system improvements, such as care coordination, may be helpful in averting some emergency department use by meeting patients' needs elsewhere.
Specific patterns can help point to where the predominant needs may exist. For example, greater emergency department use by beneficiaries who had a substance-related claim during the year underlines the particular needs and challenges for those with dual disorders. High rates of use for persons with schizophrenia and bipolar disorder, especially among disabled beneficiaries, suggest substantial needs there as well. About half of psychiatric emergency department visits for these groups plus those with other affective disorders resulted in inpatient admissions. This may partly reflect the use of the emergency department as the accepted point of entry when psychiatric hospitalization is recognized as necessary. A high rate of emergency department utilization was also noted for aged beneficiaries with selected other psychoses. This may reflect a subpopulation with especially complex diagnoses or clinical scenarios, possibly stemming from or intertwined with general medical issues.
At the same time, the large majority of utilization was not for primary psychiatric diagnoses. The fact that three-quarters of all emergency department visits for disabled beneficiaries did not result in admission (compared with half of all visits for aged beneficiaries) suggests the possibility that some disabled beneficiaries with serious mental illness may use the emergency department as a medical care point of contact because of barriers to other outpatient care. Our findings do not provide further insight into this possibility, but they suggest that further research would be useful. Probable high levels of comorbidity, the interconnectedness of psychiatric and general medical disorders, and the limits of claims data mean that these findings are simply a first step in understanding how to intervene.
The findings also suggest an opportunity for emergency departments to better promote linkage to both mental health and medical services. This will be a challenge for emergency departments beleaguered by high demand, funding constraints, and nursing shortages (
9 ). However, patients with serious mental illness can stress emergency department resources, and thus it may be viewed as worthwhile to effectively address this problem. Use of emergency department alternatives (for example, mobile assessment teams) when appropriate for psychiatric crises may also be a focus (
10 ).
The study has several limitations. Identification of diagnoses was limited to what providers recorded on claims. This descriptive analysis did not control for potentially confounding factors, such as health status, age (other than that associated with eligibility group), gender, race, or ethnicity. Future research utilizing multivariate methods would be a fruitful next step, building upon the descriptive analyses presented here. The findings do not allow determination of which visits were preventable or unnecessary. Emergency department primary diagnosis for visits that resulted in admission was inferred on the basis of inpatient primary diagnosis. Psychiatric emergency department utilization estimates may be conservative in that they were based on primary diagnosis only and excluded a primary diagnosis of substance use disorder and excluded suicide attempts unless a primary psychiatric diagnosis was listed. Finally, the study included only fee-for-service Medicare beneficiaries. Thus the study does not describe the 11% of beneficiaries who were enrolled in Medicare Advantage (managed care) plans in 2004 (
11 ).
Conclusions
Most emergency department utilization for Medicare beneficiaries with a serious mental disorder was for a nonpsychiatric primary diagnosis, but a substantial minority was for a psychiatric primary diagnosis. Emergency department utilization patterns varied significantly by psychiatric diagnostic category. Persons with substance-related claims during the year had higher utilization. Although the findings do not permit determination of which visits may have been preventable, the substantial emergency department utilization suggests the possible need to improve coordination and continuity of care in treatment systems for these high-morbidity populations. Building capacity in the emergency department setting to enhance linkage to needed services may assist in achieving optimal care.
Acknowledgments and disclosures
This study was funded by the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration. The authors thank Kay Miller, B.A., and Hong Chen, M.S., for statistical programming, and Alexander Cowell, Ph.D., Mary Jo Larson, Ph.D., Zhehui Luo, Ph.D., and Judith Teich, M.S.W., for helpful review of the manuscript.
The authors report no competing interests.