Depression has a profound impact on an individual's ability to work. There appear, however, to be social class factors that influence how much a person's depression will affect his or her work functioning. Specifically, depression has a larger effect on work functioning among individuals in lower social classes, specifically individuals in sales, service, or support occupations; individuals with lower levels of education (
1 ); and blue-collar workers (
2 ). In addition, depression has a larger effect on employability or job retention among less educated individuals (
3 ).
In this context, efforts to understand how treatment for depression affects work functioning across the social class spectrum become critically important. Unfortunately, few clinical trials for depression report work functioning outcomes (
4 ). Studies that report treatment effects on work functioning find that depression treatments have a positive impact on work functioning (
5 ). However, it is unknown whether this holds true across the social class spectrum.
A small body of literature that examines the effects of social class on outcomes in the treatment of depression shows some evidence for a positive relationship between social class and improvement in depressive symptoms (
6 ). However, none of this literature reports on work functioning. Because it is unclear how work functioning outcomes may be related to improvement in depressive symptoms, it is unknown how social class may relate to improvement in work functioning.
The study presented here assessed the role of social class as a predictor of work functioning outcomes in the treatment of depression. It also examined social class as a moderator of the relationship between improvement in depressive symptoms and improvement in work functioning.
An additional question examined here is the role of different measures of social class. There have been recent calls for renewed attention to the role of social class in treatment research (
7 ), but little work has been done to examine potential differences between various measures of social class. This issue of the measures used may be important, because there is evidence that relationships between social class and treatment outcome may differ depending on the measures used (
8 ).
There may also be different outcomes for different treatment modalities with lower social class groups. In the literature reviewed on depression clinical trials, the only two studies (
9,
10 ) to show a positive relationship between social class and outcome contained a medication condition; no evidence was found for a relationship between social class and outcome in psychotherapy conditions, except for when the trial included both psychotherapy and pharmacotherapy conditions.
In summary, the literature lacks clarity on four issues, which the study presented here attempted to address: Is social class associated with work functioning outcome in a clinical trial for major depression? Does social class moderate the relationship between depressive symptoms and work functioning? Does the relationship between social class and outcome differ by treatment modality? Do results vary for different measures of social class?
Methods
The source of data for this study is the National Institute of Mental Health (NIMH) Treatment of Depression Collaborative Research Program (TDCRP) (
11 ). This multisite collaborative study, conducted in the early 1980s, has several features that are useful for the study presented here. It included two psychotherapy conditions and a pharmacotherapy condition, along with a placebo clinical management condition, thus allowing for a comparison between treatments. It also had an adequate sample size, and it assessed all patients on a battery of instruments before treatment, at several points during treatment (four, eight, and 12 weeks), and at termination, facilitating the analyses used in the study presented here. Finally, the range of socioeconomic status among respondents was somewhat greater than in some other clinical depression trials.
The TDCRP randomly assigned 250 patients with major depressive disorder from three research sites to one of four 16-week treatment conditions: interpersonal psychotherapy; cognitive-behavioral therapy; imipramine hydrochloride plus clinical management, which was used as a standard reference treatment; and placebo plus clinical management, which was used as a control condition. A total of 239 actually participated in treatment. Patients in this clinical trial were seen for treatment from 1982 to 1986. Possible implications of the age of these data are addressed in the discussion section. Informed consent was obtained from all participants. Approval was obtained from the institutional review boards of each of the participating sites as well as from the relevant NIMH committees. Additional details regarding patients, including inclusion and exclusion criteria, therapists, and treatments are detailed in previous publications (
11 ).
The primary independent variable in the analyses presented here was social class. Social class was measured using two indicators of social class available in the TDCRP database, the Hollingshead Two-Factor Index of Social Position (ISP) (
12 ) and family income. These two measures are commonly used indicators of social class in psychotherapy research (
8 ) and allow for comparison with this literature. In particular, after reviewing treatment research articles that included social class, Liu and colleagues (
7 ) found that the ISP was the most commonly used measure of social class. Using both indicators in this study served the purpose of attempting to address discrepancies in the literature on social class and treatment outcome, because most studies have used only one of these indicators, with varying results.
The ISP categorizes individuals into five social classes. The major focus of this brief report is on the comparison of class IV and V patients (working class and poor) with class II and III patients (middle class). This grouping of categories follows what has generally been used in the psychotherapy literature. The sample in this study also included a small number (N=17) of class I patients (upper class); however, class I patients are not a major focus of this brief report, in part because of the small sample.
The dependent variable in this analysis was change in work functioning. A modified version of the work functioning domain on the Social Adjustment Scale (SAS) (
13 ), which has been used in previous analyses with TDCRP data, was used in this study. The modified work functioning domain on the SAS used previously established scores for functioning at work combined across all three domains assessed by the instrument: work outside the home, work inside the home, and academic work as a student. The modification to include work outside the home and academic work as a student was made to reduce the gender bias in earlier versions of the instrument. Cross-site reliabilities in the TDCRP ranged from .89 to .92. Reliability checks were performed on several occasions by having all clinical evaluators rate videotapes of the same group of patient interviews collected across the three sites.
Variables that have been shown in previous analyses of TDCRP data to predict outcome and that were also correlated with social class were included as covariates in this study to partial out variance caused by these known predictors. The covariates at the patient level included four measures of initial severity (scores on the work and social domains on the SAS, the Beck Depression Inventory, and the Global Assessment Scale), scores on the Dysfunctional Attitude Scale, expectation of improvement, endogenous depression, double depression, duration of current episode, and age. Minority status was also included as a covariate because of its potential relationship with social class. All patients were categorized as persons from racial-ethnic groups or white persons, instead of breaking out racial and ethnic groups separately, because there were only five patients who were nonwhite and nonblack. Treatment modality was included to control for treatment effects.
Depression severity measured by the Hamilton Rating Scale for Depression (HRSD) was included as a time-dependent covariate to control for the effect of change in depressive symptoms over the course of treatment on work functioning. This measure was chosen because it is the symptom measure that has been consistently used in analyses with TDCRP data (
11 ).
Two moderators were also included. The interaction between treatment modality and social class was included to test the possibility that treatment modality might moderate the relationship between social class and outcome. The interaction between the time-dependent symptom measure, the HRSD, and each time-invariant social class measure was also included to test the hypothesis that social class moderates the relationship between symptoms and functioning.
Study analyses were based on hierarchical linear modeling (
14 ) to test the role of social class as a predictor of work functioning over the course of treatment. Multilevel modeling has been used previously with the TDCRP data and has several benefits for the analyses presented here. Most important, it allows all participants to be included in the analyses, regardless of whether they complete treatment, and it does not require the use of end-point analyses. This is particularly important in analyses focusing on the relationship between social class and treatment outcome, because social class has frequently been correlated with attrition. Using all available time points—pretreatment, four, eight, and 12 weeks, and termination—hierarchical linear modeling estimated person-specific time trends based on the individual's data and the population from which the individual was drawn. This allows for examination not simply of differences for all patients at the end of treatment, but rather differences in the course of improvement over time.
Nested models were compared to determine whether random effects should be included in the final model. A random effect on the change rate significantly improved the model (
χ 2 =40.22, df=4, p<.001), so it was included in the final model. The reliability of the random coefficient on the HRSD score was too low (.08) to include it in subsequent analysis. A simple error structure (independent errors with constant variance) was assumed for these analyses, following the recommendation of Bryk and Raudenbush (
14 ) for short time series.
Results
Of the 239 patients who actually entered treatment, 168 (70%) were women, and 212 (89%) were white. The range of social class in ISP categories represented in the patient sample included 17 (7%) upper-class patients, 154 (64%) middle-class patients, and 68 (28%) working-class or poor patients, as rated by the ISP. Annual family incomes ranged from $1,200 to $175,000, with an average of $27,000 (which would be the equivalent of $53,000 in 2010 dollars). There were no significant differences in the distribution of social class groups or family income across treatment conditions.
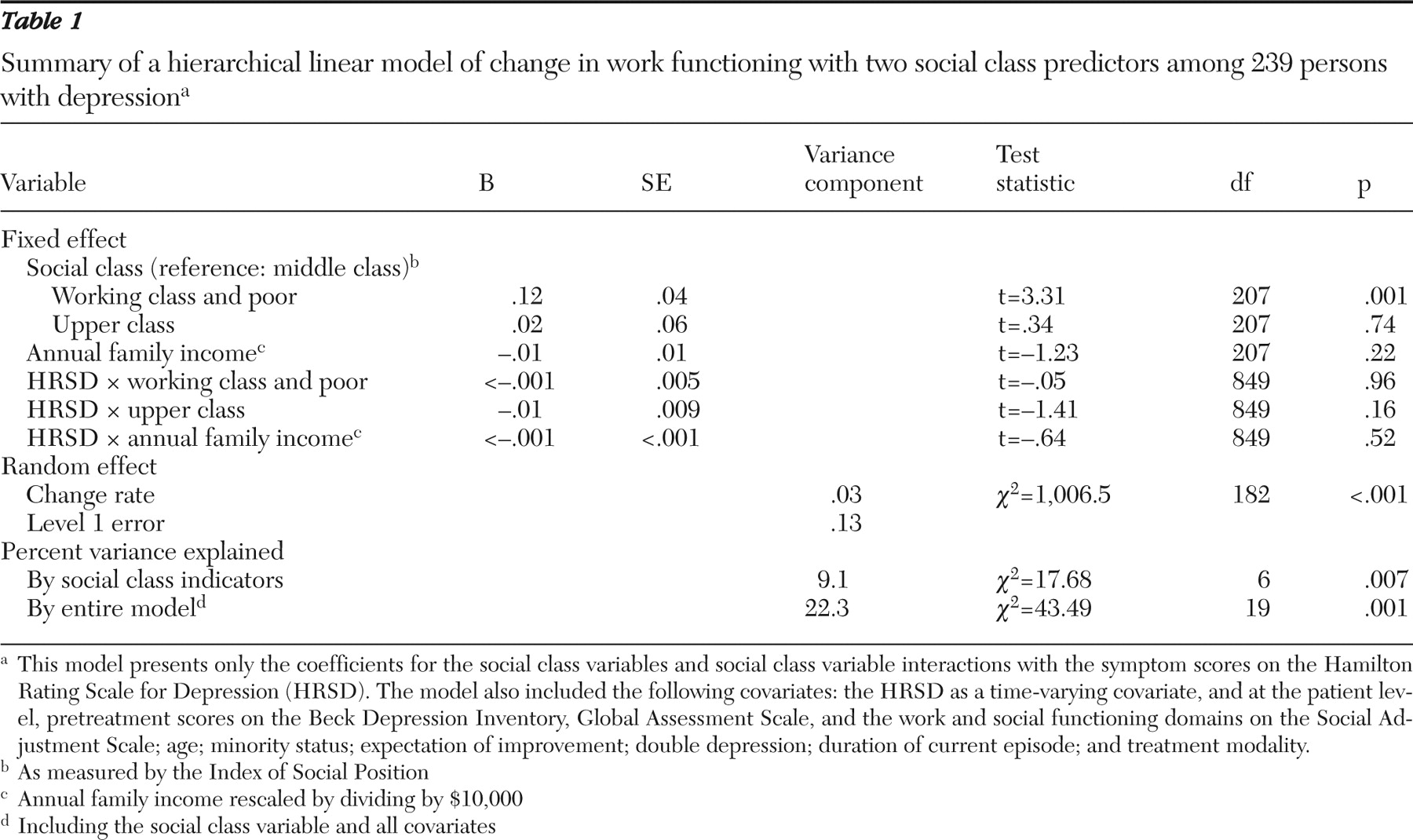
As
Table 1 indicates, the ISP was related to outcome in work functioning. Specifically, patients from classes IV and V (working-class and poor patients) had lower rates of improvement in work functioning than patients from classes II and III (middle-class patients). Family income was not related to improvement in work functioning.
Social class did not appear to moderate the relationship between depressive symptoms and work functioning. None of the interactions between depressive symptoms and the ISP or family income were significantly associated with improvement in work functioning.
None of the interactions between ISP and treatment modality were significant, so these interaction terms were dropped from the final model.
The percentage of variance in work functioning explained by the social class indicators was 9.1%.
Discussion
These findings show preliminary support for a relationship between social class and change in work functioning; when the ISP was used to measure social class, patients from a lower social class experienced significantly fewer gains in work functioning over the course of treatment, compared with middle-class patients. The ISP was more sensitive to social class differences in improvement in work functioning than was family income.
No previous work has documented the relationship between social class and work functioning outcomes in depression trials. However, few depression studies have published outcome results based on work functioning, and none has examined patient predictors of work functioning.
One route to improved outcomes might be to adapt current therapies to include a greater focus on the daily work and economic stressors that low-income individuals face. It also seems likely that these findings speak to the importance of addressing factors that might prevent an individual from achieving satisfactory work functioning, such as lack of transportation or child care, difficulties that may be more likely to occur for individuals from a lower social class. It seems possible that case-management services, such as those provided in a depression treatment study specifically targeting low-income patients of color (
15 ), might increase access to supports, which would further address these issues and improve work functioning. Notably, however, therapy cannot address additional issues related to work functioning, such as lack of education or work experience, or structural differences in the workplace related to the social class of the worker. Additional research is needed to understand how lower social class might limit patient gains in work functioning and how to best improve work functioning among depressed patients from a lower social class.
These results provide no evidence for differences between cognitive-behavioral therapy, interpersonal psychotherapy, or pharmacotherapy in their ability to effectively treat depression among clients with lower socioeconomic status. This may suggest that common factors, not treatment-specific factors, are implicated in the differences in change in work functioning by social class.
A possible limitation of this study is that the TDCRP data used in this study are somewhat dated, because they were collected in the 1980s. This may limit the generalizability of the findings. In particular, the study used DSM-III diagnostic criteria for major depression and a somewhat dated measure of work functioning, the SAS. In addition, the results in the pharmacotherapy condition, which used imipramine, cannot be generalized to more current treatments with selective serotonin reuptake inhibitors or serotonin-norepinephrine reuptake inhibitors.
The patient sample in this study limits the generalizability of the findings. The sample was skewed toward being highly educated and contained a very small number of patients of color. Unfortunately, many clinical trials lack such patients. Future research needs to examine this question regarding social class and work functioning in studies with larger samples of working-class and poor patients and patients from racial-ethnic minority groups.
Conclusions
Despite the study's limitations, it offers several important findings. The first points to the important role that lower social class can play as a negative predictor of improvement in work functioning when cognitive-behavioral therapy, interpersonal psychotherapy, or pharmacotherapy is used to treat depression. These findings highlight the importance of a renewed focus on social class in the treatment literature and suggest that work functioning may be an especially important area to pursue in further research with lower social class populations. Differences in findings that depend on the social class indicator used suggest that additional work is needed to better conceptualize social class to focus on aspects most relevant to depression and work functioning.
Acknowledgments and disclosures
The author reports no competing interests.