Smoking is the largest single cause of preventable illness and death (
1 ), and it is predicted that by 2015 more than six million individuals will die from smoking-related diseases (
2 ). Proof that these morbidity and mortality rates are disproportionate among persons with a serious mental illness is now becoming evident. Rates of smoking are two to four times higher among persons with mental illness (
3 ), and it is estimated that persons with mental illness make up 44% of the U.S. tobacco market (
3,
4 ). One study reported that 68% of persons with schizophrenia who smoke consume 25 or more cigarettes per day, compared with 11% of the general smoking population (
5 ), suggesting a higher level of addiction for these individuals.
Because of a requirement from the Joint Commission (
6 ), coupled with the elevated health risks for persons with mental illnesses who smoke, many U.S. psychiatric hospitals prohibit smoking for staff and patients (
4,
7 ). However, there remains considerable resistance from staff to implementing smoking restrictions in psychiatric hospitals. A survey of staff attitudes toward implementing a smoking ban found that although only one in ten staff in general hospital settings disagreed with the ban, one in three staff in psychiatric settings were opposed to such restrictions (
8 ). Other studies showed that staff from psychiatric hospitals often expressed concerns that such a policy would have a negative impact on the hospital's treatment milieu (
9,
10 ). Staff often cite smoking as a means to establish a therapeutic relationship with patients or to reward desired behavior (
11 ). Yet studies show that smoking bans do not increase aggression, use of seclusion, discharge against medical advice, or use of as-needed medication (
9 ) and that persons with mental illness can successfully quit smoking and benefit from smoking cessation interventions (
12,
13 ).
In the study presented here, we hypothesized that compared with hospitals that permit smoking, hospitals that have adopted a smoke-free policy would experience fewer adverse events (such as fires, elopements, threats among patients and staff, and smoking as a precursor to incidences that lead to seclusion or restraint), offer more smoking cessation treatments, and provide more specialty training for clinical staff on smoking-related issues.
Methods
In 2006 and 2008 the National Association of State Mental Health Program Directors Research Institute, Inc. (NRI), surveyed state psychiatric hospitals about their current smoking policies. For the 2006 survey 181 of 222 hospitals completed the survey (82% response rate), and 59% (N=107) permitted smoking. For the 2008 survey, 164 out of 219 hospitals completed the 2008 survey (75% response rate), and 51% (N=84) permitted smoking. Results from each survey have been independently published (
14,
15 ). Each survey was distributed via e-mail, and a member of hospital clinical management staff completed and returned the survey. At least three follow-up e-mails were sent to nonrespondents over a three-month period.
The surveys were developed by a team of medical directors, quality improvement managers, and researchers. In 2006 a pretest of the instrument was completed by a small sample of psychiatric hospitals and resulted in minor revisions and a splitting of the instrument into two versions: one for hospitals that permit smoking by clients and one for those that do not permit smoking. In 2008 the survey was merged back into one tool with expanded questions related to current smoking policy, smoking cessation treatment options, and aftercare planning and referrals for smoking education. The surveys did not need approval from an institutional review board because the subjects were organizations; behavior of individual clinicians or patients was not a focus.
All respondents in the study presented here completed the same survey version in 2006, self-selecting that smoking was permitted. The 2008 survey version identified seven policy levels related to smoking, ranging from the most liberal to the most restrictive and aligned with the definitions used by the Joint Commission in a 2007 unpublished online survey of smoke-free policies of U.S. hospitals. Using the 2008 option list, NRI categorized a hospital as nonsmoking only if smoking was prohibited on all hospital premises (defined as building, balconies, patios, courtyards, areas adjacent to exit doors, parking areas, and lawns) and if there were no designated smoking areas on the campus. The policy must apply to patients, visitors, and staff members. This strict definition of a smoke-free campus was adopted because allowing patients, staff, or visitors to smoke in any area of the hospital or campus is inconsistent with promoting a healthy lifestyle.
To test whether a policy change affected the key factors under investigation, the McNemar statistical test was performed. The McNemar statistic is used to detect changes in survey responses for dichotomous variables following a policy change using a before-and-after design. A significant McNemar score indicates that more hospitals moved in one direction than the opposite direction—for example, more hospitals moved from a "yes" response in 2006 to a "no" response in 2008 than moved from a "no" response in 2006 to a "yes" response in 2008. The McNemar test was performed separately for hospitals that changed to a nonsmoking policy and those that maintained a smoking policy. If both groups had significant changes and the changes were in the same direction, one could conclude that the change was independent of policy.
Results
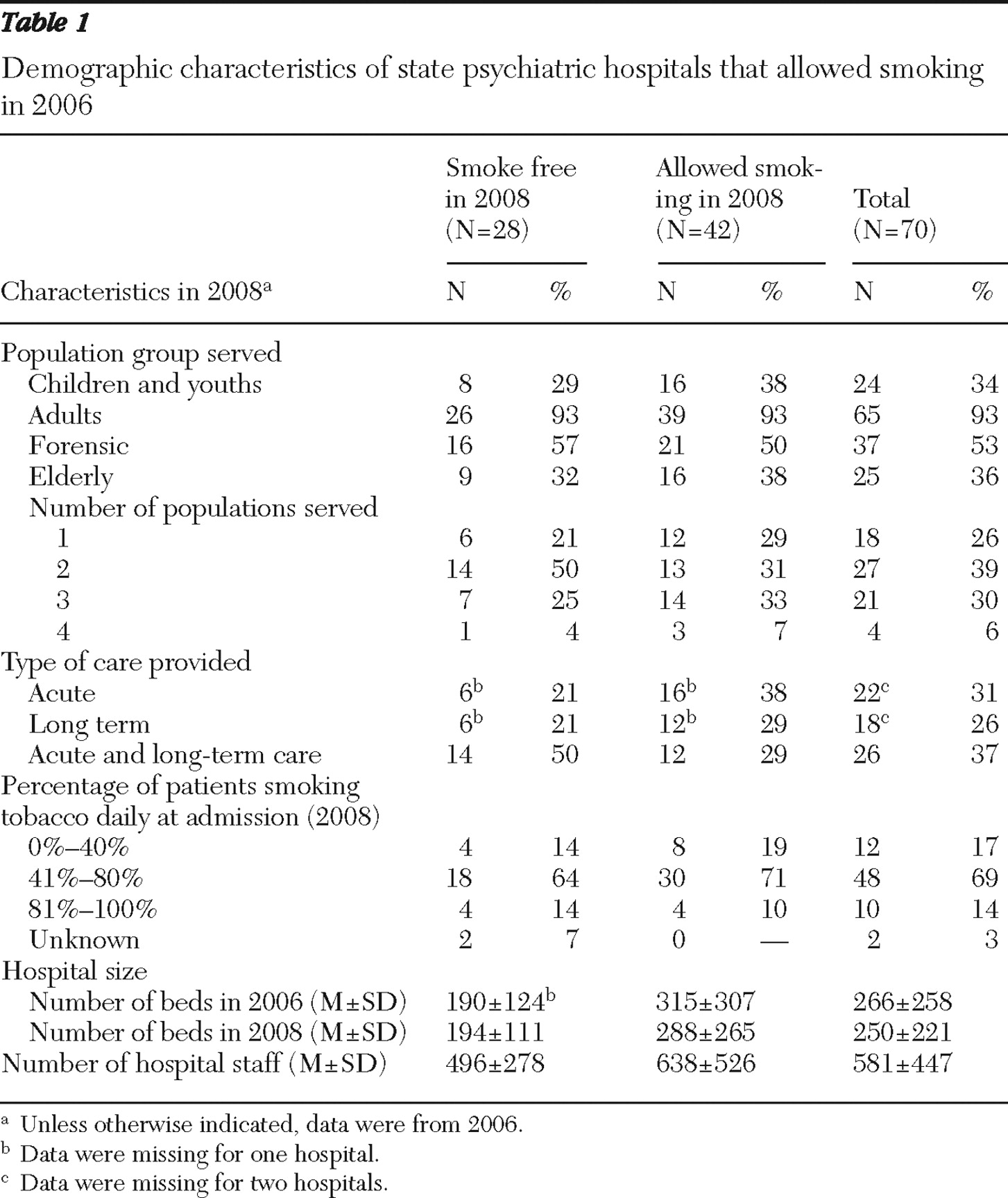
For the 2006 survey 107 hospitals reported that smoking was permitted. Of these hospitals, 70 also responded in 2008 (65%). Results of the study presented here are based on the 70 hospitals that responded in both 2006 and 2008. Forty-two hospitals (60%) were still categorized as permitting smoking, and 28 hospitals (40%) changed their policy and were smoke free in 2008. Of the 42 hospitals that did not entirely ban smoking, four (10%) permitted smoking in designated indoor areas, 20 (48%) prohibited smoking indoors but permitted it outside, and 18 (43%) prohibited smoking inside all facility buildings and on most facility property outdoors.
Across the study period, hospital size within each group remained constant. For the sample under study, there were one-third fewer beds in hospitals that converted to a nonsmoking policy than there were in hospitals that continued to allow smoking in 2008 (p<.05). There were no significant differences in hospital staffing capacity between the two groups.
Table 1 summarizes the demographic characteristics of patients in the two groups under study and of the total sample.
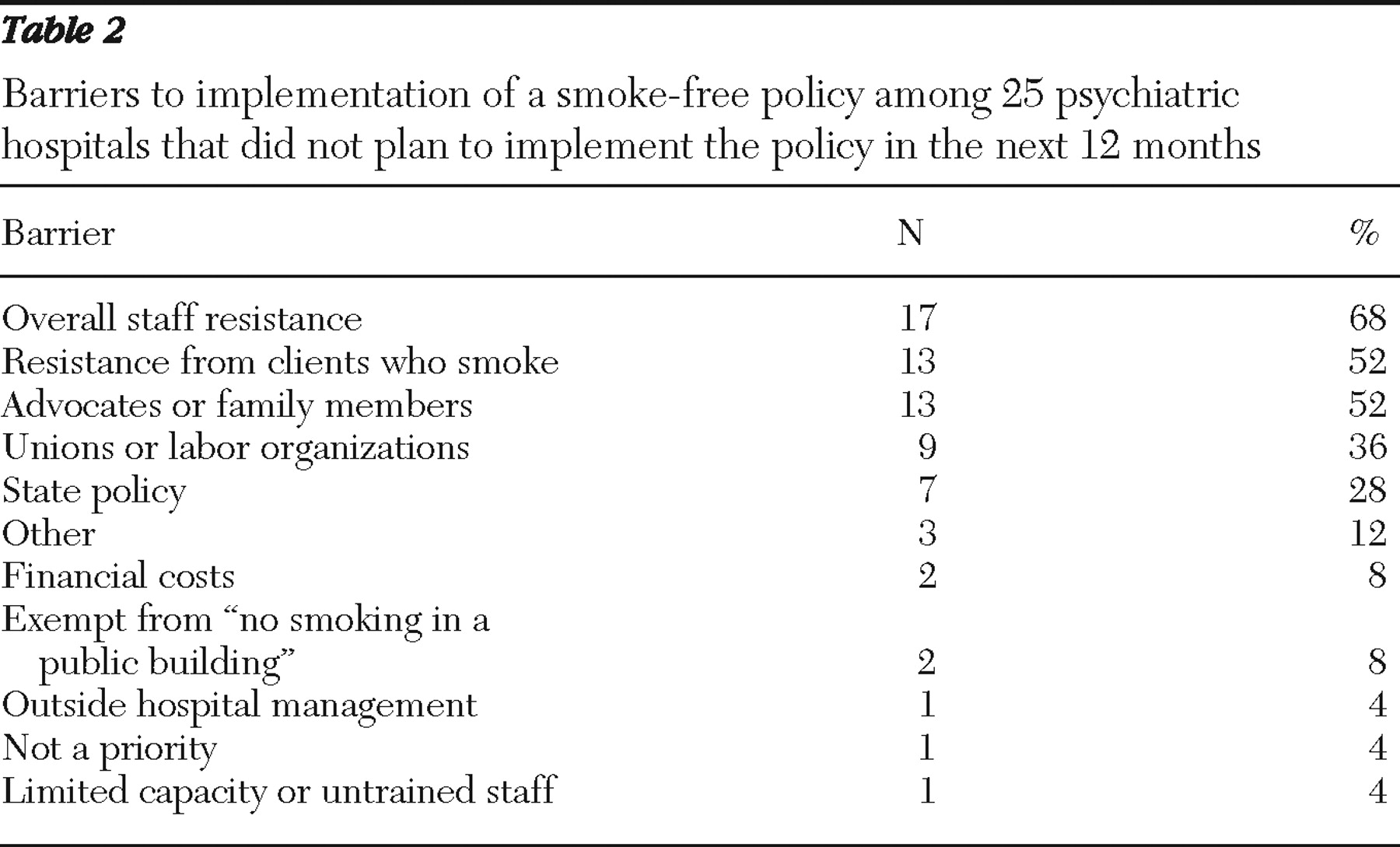
Barriers impeding a smoke-free policy
In the 2008 survey, hospitals that allowed smoking were asked to identify from a checklist the barriers that prevented them from converting to a nonsmoking hospital within the next 12 months. Twenty-five of the 42 hospitals (60%) that did not adopt a smoke-free policy reported that they were not planning to change smoking policies within the next 12 months. Hospitals that said they were not going to adopt a smoke-free policy reported a mean±SD of 3.1±1.6 barriers. The greatest resistance to a smoke-free policy arose from staff and patients who smoke. Advocates and family members were also frequently identified as opposing a policy change (
Table 2 ).
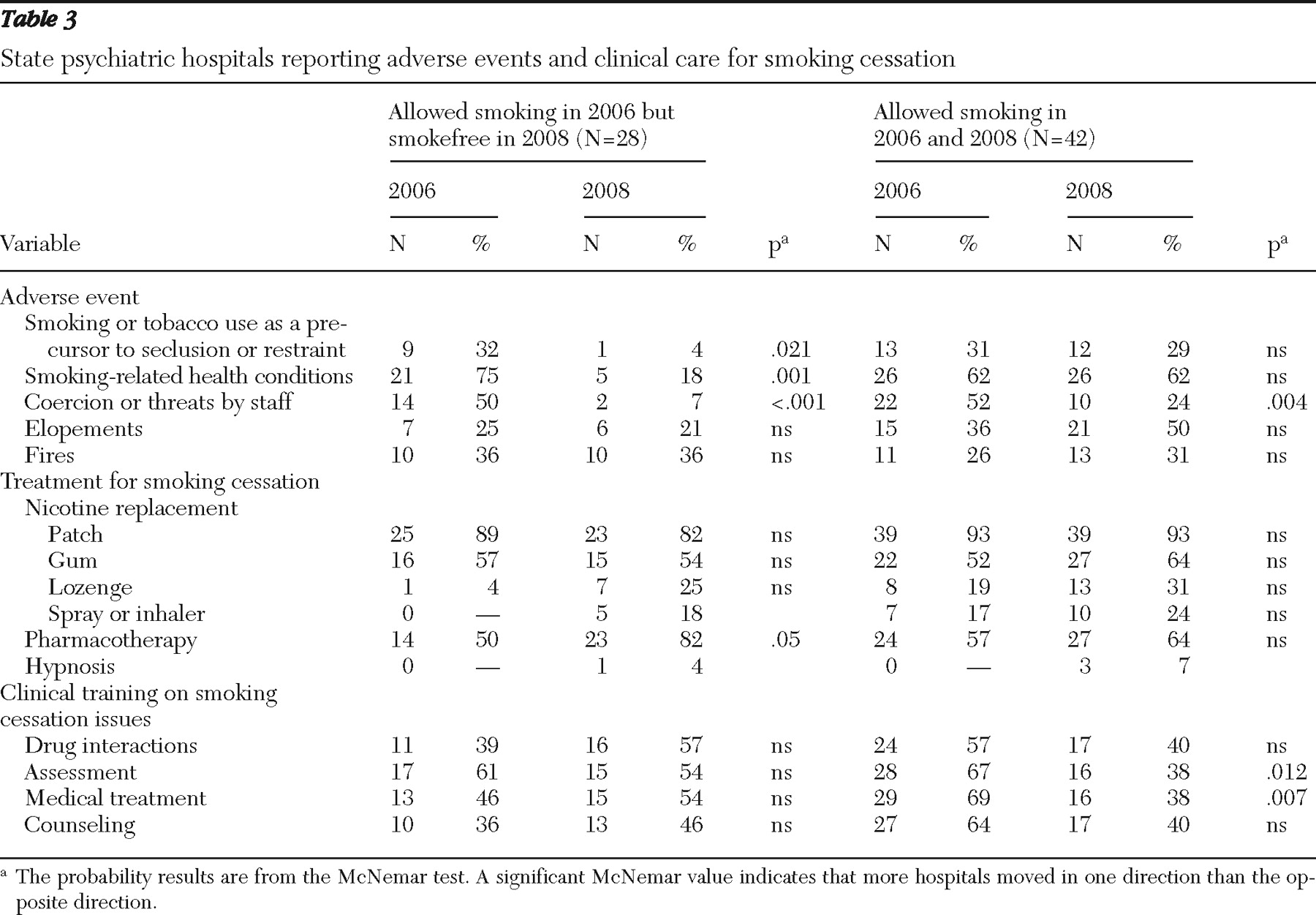
Concerns for adverse effects
Among hospitals that changed to a smoke-free policy, the proportion that reported adverse events decreased by 75% or more in three areas: smoking or tobacco use as a precursor to incidents that led to seclusion or restraint (32% in 2006, 4% in 2008), smoking-related health conditions (75% in 2006, 18% in 2008), and coercion or threats among patients and staff (50% in 2006, 7% in 2008) (
Table 3 ). The McNemar test showed a significant movement away from adverse events for hospitals that adopted nonsmoking environments.
Among hospitals that did not adopt a smoke-free policy, there was a 54% decrease in the proportion of hospitals that reported adverse events in the area of coercion or threats among patients and staff (52% in 2006, 24% in 2008). Elopements and fires related to smoking were experienced by a small number of hospitals (approximately 30% overall); however, the McNemar test was not significant for both types of hospitals for elopement and fire events related to smoking.
Smoking cessation treatment options
Among hospitals in the study, the smoking cessation treatments commonly available included nicotine replacement therapies (NRTs) (patch or gum) and pharmacotherapy; however, the number of hospitals offering these and other treatments changed between time periods. Overall, among the group of hospitals that changed to a smoke-free policy, the greatest change was in the number offering nicotine lozenges (4% in 2006, 25% in 2008) and spray or inhaler treatment options (0% in 2006, 18% in 2008). However, the number of nonsmoking hospitals that offered any type of NRTs did not change significantly throughout the study period (N=27, or 96%, in 2006 and N=24, or 86%, in 2008). The McNemar test showed that in hospitals that adopted a smoke-free policy, there was a significant increase in the number offering patients pharmacotherapy for cessation. Fifty percent offered pharmacotherapy for smoking cessation in 2006, compared with 82% in 2008. There was little change between 2006 and 2008 for hospitals that did not adopt a smoke-free policy (
Table 3 ).
In 2008 a total of 29 hospitals (41%) in the sample reported not offering any smoking cessation classes (N=11, or 39%, for smoke-free hospitals, and N=18, or 43%, for the hospitals that allowed smoking). Among hospitals offering smoking cessation classes, there was an increase in the frequency of weekly offerings from 2006 to 2008 for all hospitals in the sample: 18 hospitals (26%) offered weekly sessions in 2006 compared with 37 (53%) in 2008, but the difference was not significant. There was no difference between hospitals that were smoke free and those that were not (smoke-free hospitals: N=7, or 25%, in 2006 and N=15, or 54%, in 2008; hospitals that allowed smoking: N=11, or 26%, in 2006 and N=22, or 52%, in 2008). Daily offerings of smoking cessation classes were rarely offered by hospitals at either time period (N=3 in both 2006 and 2008).
Specialty training
At least one-third of the 70 responding hospitals offered some type of specialty training in both 2006 and 2008. For hospitals that adopted a smoke-free policy, the number of hospitals that offered training to staff on smoking cessation issues remained nearly the same for the two time periods. There was a significant decrease between 2006 and 2008 in the number of hospitals that permitted smoking offering specialty training in the areas of assessment (p=.012) and medication treatments (p=.007) for smoking (
Table 3 ).
Discussion
The main purpose of this study was to investigate the effects of adopting a smoke-free policy in state psychiatric hospitals on key characteristics of the treatment environment. The hospital groups in the study did not differ on patient demographic characteristics or services; however, hospitals that adopted a smoke-free policy tended to have fewer beds.
Survey results indicated that state psychiatric hospitals are increasingly becoming smoke free, yet there are still impediments that hinder hospitals from enacting a nonsmoking policy. Responding hospitals cited three groups most often as the strongest resisters to a smoke-free campus: staff, patients who smoke, and advocates and family members. Various reasons are cited in the literature regarding why staff in psychiatric facilities may be less receptive to a smoke-free environment than staff in general medical hospitals, including the fear of aggressive behavior by patients, the impact of restrictions on staff who smoke, and the belief that smoking has a therapeutic role (
8,
16,
17,
18,
19 ). Smaller hospitals in our sample may have had more success changing policies because fewer patients and staff members would have been affected. This finding underscores the need to revisit the communication channels between hospital management and staff and to develop innovative strategies that take into consideration staff needs and concerns both before and after the implementation of a smoke-free policy.
Our finding on groups resisting change is consistent with the findings of Williams (
19 ), who reported that the use of civil rights-related arguments by advocates has been effective in maintaining permissive smoking policies in psychiatric hospitals. Hospitals must be proactive by involving advocates, families, and unions before, during, and after a smoking policy change and by providing information regarding the benefit of a smoke-free environment, including the need to protect the rights of nonsmokers from exposure to second-hand smoke. Any major policy change must also include a patient education component.
All of the 42 hospitals that permitted smoking in 2008 restricted it to designated areas; however, more than half of these hospitals (60%) were not planning to change their current smoking policy and reported an average of three barriers to going smoke free. This finding suggests that hospitals have not internalized the positive effects of a smoking cessation policy, even in the face of substantial research that documents the positive outcomes of becoming a completely smoke-free environment.
Results of this study contradict previously reported findings that adverse consequences, such as elopements, fires, and threats among patients and staff, may increase as a result of a smoking ban in psychiatric hospitals (
9,
20,
21 ). The survey results confirmed that there were fewer (or no) adverse effects following the implementation of a smoke-free hospital campus. In fact, our results reflect a reduction after the policy change in the number of hospitals reporting tobacco use as a precursor to incidents that led to seclusion and restraint. These findings suggest that the nonsmoking policy was associated with a positive effect on staff and their interactions with patients, as evidenced by a reduction in negative events.
It was hypothesized that when a hospital adopts a smoke-free policy, evidence-based smoking cessation interventions would increase. A large proportion of patients smoke (
4 ), and such patients will be more successful in adhering to the hospital's nonsmoking policy if they have access to smoking cessation resources. Our results showed a significant increase in the number of hospitals offering pharmacotherapy to counteract nicotine addiction when the hospital changed to a nonsmoking policy between 2006 and 2008 and a nonsignificant change in the number of hospitals offering NRTs. The increase may be because (unlike NRTs) the primary pharmacotherapy treatments for nicotine addiction (primarily bupropion) are already on the hospital's formulary and readily available. Bupropion is available in all psychiatric hospitals because of its wide use as an antidepressant and typically costs less than $50 per month.
Comprehensive tobacco cessation programs should include both NRTs and behavior therapy, such as smoking cessation counseling (
22,
23 ). Our results showed that nearly half of the hospitals in our sample, regardless of their smoking policy, offered smoking cessation group sessions on a weekly basis, while 41% offered no sessions. The frequency of group sessions was not affected by a hospital's smoking policy. Although the reason for not offering sessions may be related to time constraints on an already overburdened staff, Prochaska and colleagues (
7 ) posited that the staff time spent managing a patient's smoking behaviors could be more productively used to deliver cessation counseling services.
Both the 2006 and 2008 surveys inquired whether clinical staff received specialty training to address smoking cessation issues. It was hypothesized that staff training would increase following the implementation of a smoke-free campus; however, this result was not substantiated. Hospitals may not be focusing on specialty staff training because of fiscal constraints or because their administrations believe that clinicians have already received such training during their formal education. Prochaska and colleagues (
24 ) found that psychiatry residents reported receiving either no or inadequate training on smoking cessation in medical school or as part of on-the-job training, despite a high interest in the topic. Incorporating smoking cessation instruction as a component of ongoing in-service training for clinical staff offers the potential to reach a large number of smokers who may not otherwise be encouraged to quit.
The results of this study were based on hospital responses to surveys administered in 2006 and 2008. Because slightly different survey instruments were administered in each year and because the individuals responding were unidentified and may not have been consistent across the two years, a few limitations to the findings warrant mention. Although both surveys were sent to the hospital directors, the actual person completing the survey and their position at the hospital could not be determined. Because the surveys were completed by only one person at the hospital and not based on observational report, there is no way to know whether actual practices differed from the general report of the respondent.
For the 2006 survey, hospitals self-selected which tool to complete (smoking or nonsmoking) based on their own interpretation of their current smoking policies. In 2008 one survey instrument was administered and hospitals were categorized as smoking or nonsmoking post facto by the researchers on the basis of survey responses. It is possible that a hospital's self-selection of nonsmoking in 2006 would be inconsistent with the researchers' definition applied in 2008, resulting in a loss of hospitals from the study group. As expected with longitudinal studies, the response rates in the study presented here were affected by the loss of participating hospitals from one time point to the other. Of the 107 hospitals that responded to the 2006 survey and self-selected that smoking was permitted, 70 also responded in 2008 (65%). It is unknown how many nonresponses were due to closures and mergers.
Conclusions
State psychiatric hospitals serving all types of patient populations are adopting smoke-free policies; however, some significant barriers still exist that prevent many hospitals from converting to smoke-free environments. Adopting a smoke-free policy was not associated with an increase in adverse events, such as events related to smoking that lead to seclusions or restraints, coercion, elopements, or fires. Results show that adopting a smoke-free policy did not promote changes in NRTs offered, the availability of smoking cessation sessions, or specialty training for clinical staff on smoking-related issues. Continued research is warranted, particularly on factors that facilitate policy change and the role of the State Mental Health Authority in a hospital's adoption of a smoke-free environment.
Acknowledgments and disclosures
This work was partially supported by the University of San Francisco's Smoking Cessation Leadership Center.
The authors report no competing interests.