Measures
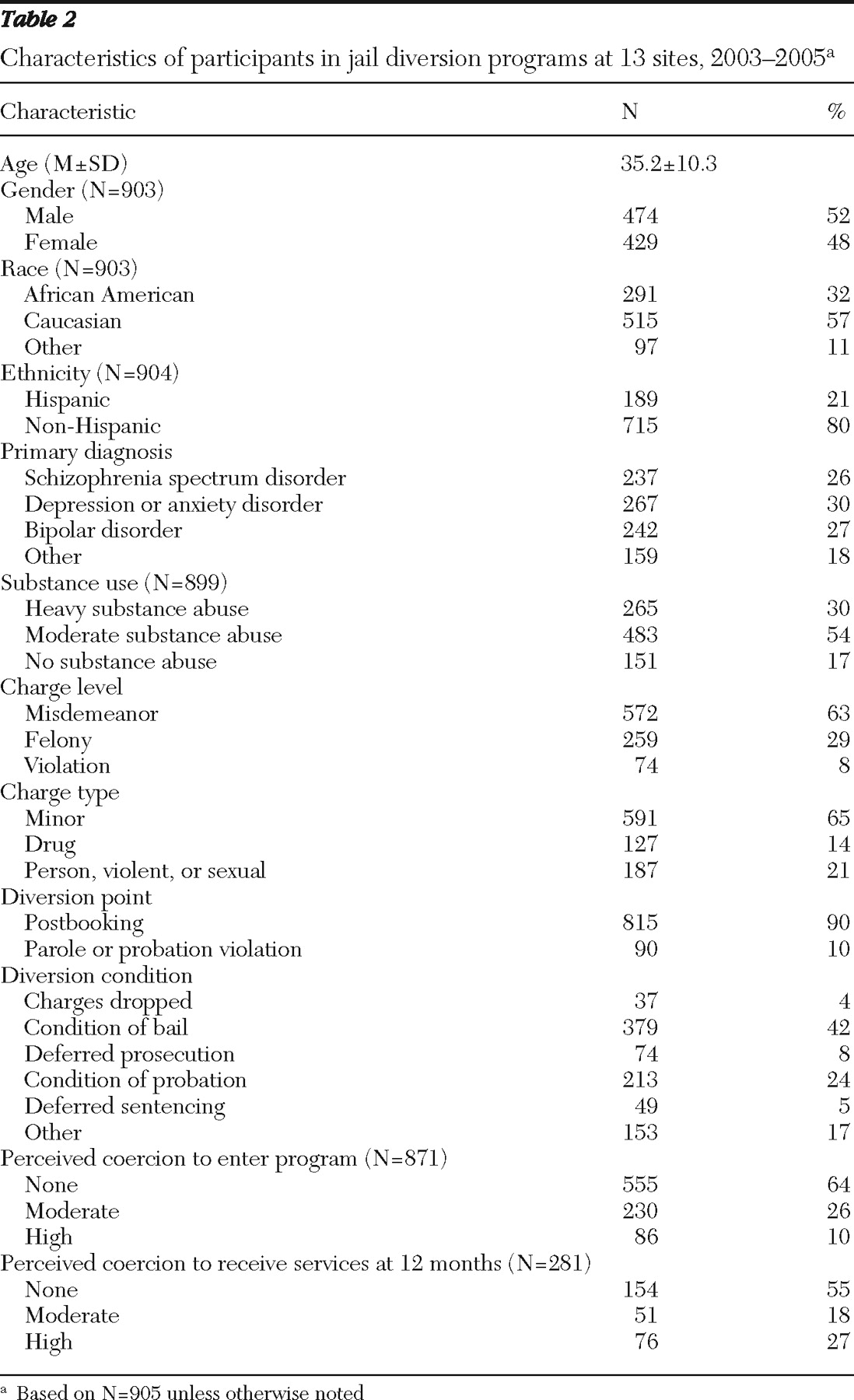
An interview protocol required by SAMHSA for purposes of program evaluation was administered to all participants. The interview included Government Performance Reporting Act questions on demographic characteristics (gender, race and ethnicity, date of birth, education level, employment, income, and housing status) and alcohol and drug use. Questions on substance use assessed days of use in the 30 days before arrest or jail detention. The number of reported days of drinking to intoxication and using illegal drugs was used to construct a substance abuse variable with three levels: none, moderate, and heavy.
Participants were asked dichotomous (yes-no) questions regarding the experience of a range of traumatic events. The questions assessed whether participants experienced physical assault ("has anyone choked, kicked, bit, or punched you?"), threat or use of a weapon ("has anyone threatened you with, or actually used, a knife, gun, or other weapon to scare or hurt you?"), sexual abuse ("has anyone forced you to have sex when you did not want to?"), and witnessing violence ("have you witnessed a physical or sexual assault against a family member, friend, or other significant person?") over their lifetime and in the past 12 months.
Perceived coercion was assessed with the MacArthur Perceived Coercion Scale (PCS). The PCS includes five true-false items from the MacArthur Admission Experience Survey and was originally developed to assess perceived coercion associated with the process of hospital admission (
14 ). The wording was modified for the baseline administration to reflect perceived coercion to enter the jail diversion program. Items included, "I felt free to do what I wanted about going to the diversion program," "I chose to go to the diversion program," "It was my idea to go to the diversion program," I had a lot of control over whether I went to the diversion program," and "I had more influence than anyone else on whether I went to the diversion program." At the 12-month interview, participants who received any mental health or substance abuse services responded to PCS items in regard to perceived coercion to receive outpatient services. Cronbach's alpha was .69.
Mental health symptoms were assessed with the Colorado Symptom Index (CSI) (
15 ), which consists of 14 self-reported mental health symptom items rated on a 5-point frequency scale. Higher scores are associated with greater symptom severity. Cronbach's alpha was .90.
Arrest data 12 months before the target arrest or incident date and 12 months after the release date associated with the target arrest were collected by each of the 13 jail diversion programs and submitted to the coordinating center. Data on mental health and substance abuse service use were available for six of the 13 jail diversion sites. These data were collected by the diversion program for six months postbaseline for outpatient services and 12 months postbaseline for hospitalizations and emergency department use.
Statistical analyses
Simple two-way associations between each predictor variable and the dependent variables were conducted. The five items regarding perceived coercion to enter the jail diversion program were summed, with a mean score of 1.4±1.4 and a possible range of 0 to 5 points. Higher scores indicate greater perceived coercion. Because the scores on the PCS were not normally distributed, an ordinal variable was created with three levels: highly coerced, moderately coerced, and not coerced. Participants were categorized as highly coerced if they answered "false" to four or five of the five items, moderately coerced if they answered "false" to two or three of the items, and not coerced if they indicated that four or five of the items were true.
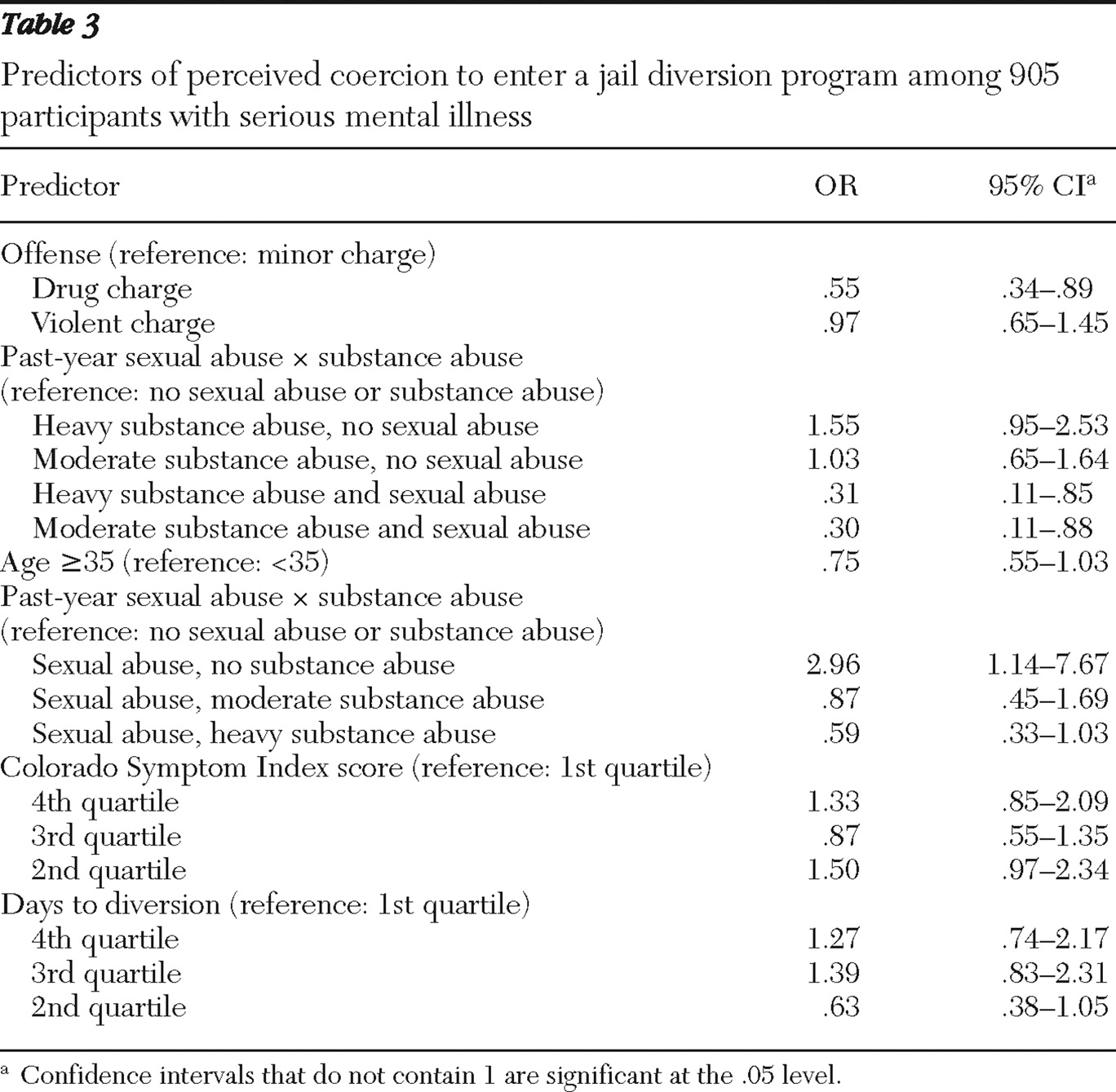
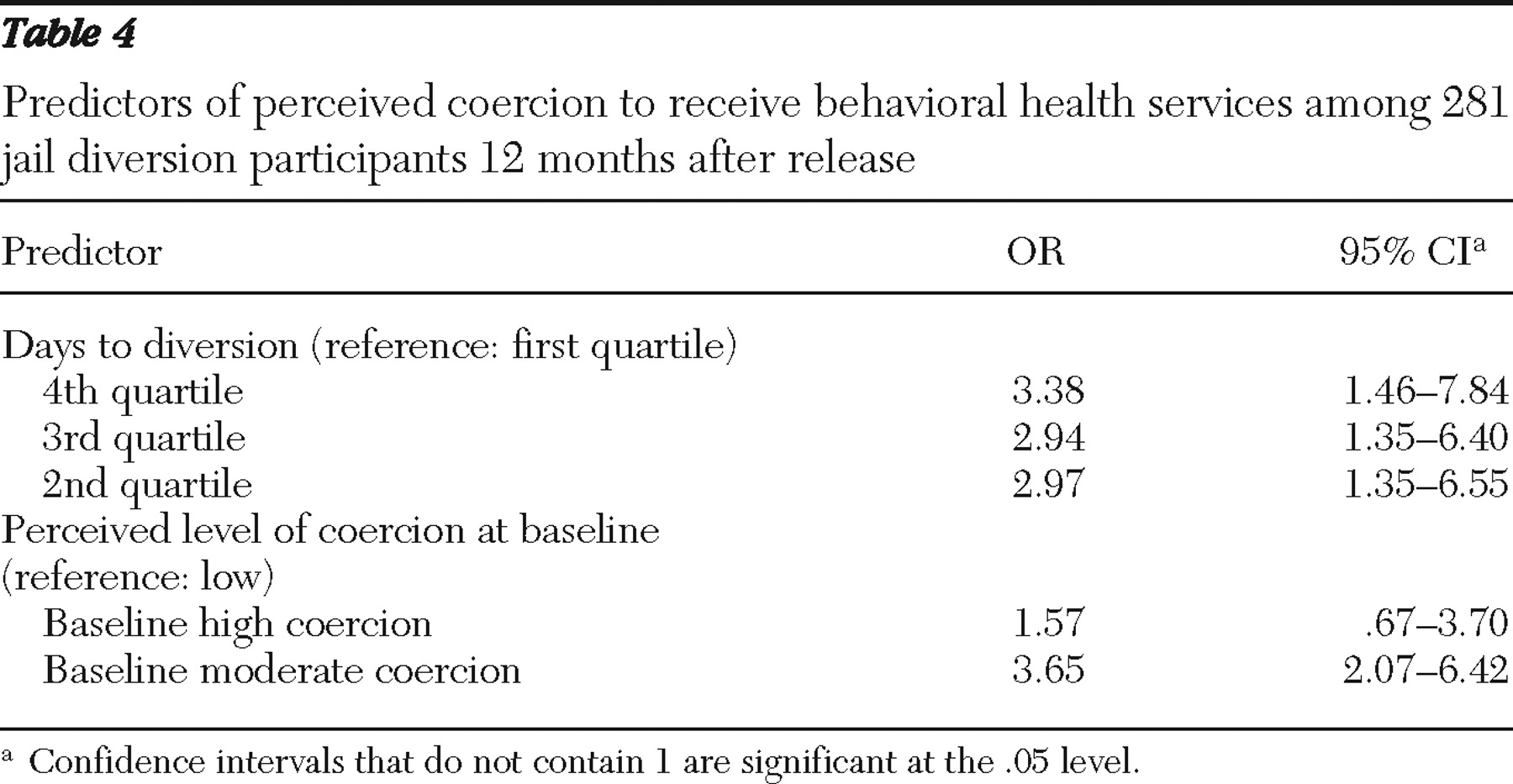
Potential predictors of coercion to enter the jail diversion program (baseline) or to receive behavioral health services (12-month) included characteristics of the violation, such as charge type (drug offense, minor offense, or an offense involving another person, violence, or sex), and charge level of the index violation (misdemeanor, felony, or violation), point of diversion (at booking or on parole or probation violation), days from arrest to diversion (quartiles), and number of previous arrests; demographic variables, including age (dichotomized at age 35), gender, black race, Hispanic ethnicity, income (dichotomized at the median of $596 per month), employment status, education (dichotomized at 12 years), and housing status (has housing or lives in a shelter or on the street); clinical variables, such as diagnosis (schizophrenia, bipolar disorder, depression or anxiety disorder, or other) and severity of symptoms on the CSI (in quartiles); substance abuse status (nonuser of drugs or alcohol, moderate user or abuser, or heavy abuser); and exposure to violence (indicator of witnessed violence in past 12 months and indicator of lifetime witnessed violence, indicator of physical violence victimization in past 12 months and indicator of lifetime physical violence victimization, indicator of sexual abuse in past 12 months and indicator of lifetime sexual abuse, and sum of traumatic life events in past 12 months and sum of lifetime traumatic events).
Interactions chosen a priori for investigation were the interactions between race and gender, sexual abuse and gender, physical abuse and gender, sexual abuse and drug use, and physical abuse and drug use. The race-by-gender interaction term was chosen because past research has indicated Caucasian women are most likely to be diverted (
3 ). Interaction terms of gender with physical or sexual abuse were chosen because of the potential for the abuse variables to measure vastly different experiences for women and men. We chose to examine the possible interaction of physical and sexual abuse with substance abuse because a history of sexual abuse or posttraumatic stress disorder is associated with reporting more coercive experiences in the psychiatric setting (
16 ) and because the greater mental illness severity found among individuals with a history of interpersonal abuse and also substance abuse problems was assumed to amplify the effects of the interpersonal abuse on coercion. No other interactions were considered.
A random-effects model was used to account for the potential correlation between participants at each site. The SAS GLIMMIX procedure was used with a multinomial response distribution, cumulative logit link function, and maximum likelihood estimation in order to model the dependent variables—coercion to enter the diversion program and coercion to receive behavioral health services. The proportional odds model was selected for the ordinal coercion outcomes after testing in a saturated model whether the fit of the generalized logistic model was superior. Starting with a model containing all main effects and the a priori selected interactions, a stepwise model selection procedure was implemented. To model outpatient service counts, we used a random-effects model with a negative binomial distribution and log link. Backward selection was used to select a final model.