Substance abuse in this dually diagnosed population contributes to increased hospital admissions and poor treatment outcomes (4-9). Despite the prevalence and impact of substance use disorders in schizophrenia, previous studies indicate deficiencies in the quality of care provided for this population (10-13).
Some of the measurable indicators of inpatient management of a substance use disorder include the provision of withdrawal prophylaxis, referral to inpatient substance abuse treatment, and diagnosis and treatment referral at discharge. For patients with schizophrenia who have received a diagnosis of a substance use disorder, disposition, including treatment referral, is particularly important (
18). For example, when such a patient makes the transition from inpatient to outpatient care, communication of the substance use diagnosis to outpatient providers and referral to appropriate substance abuse treatment is necessary to ensure continuity of care.
The purpose of this descriptive study was to examine the extent of clinicians' recognition of comorbid substance use disorders among inpatients with schizophrenia who had a comorbid substance use disorder as diagnosed by researchers using a structured interview. We expected that clinicians would often not recognize substance use disorders in patients admitted to an acute psychiatric unit. We also wanted to explore issues of clinical management, including whether patients would receive a referral to inpatient substance abuse treatment programs, a discharge diagnosis of a substance use disorder, and a referral to outpatient treatment services at discharge. In addition, we hypothesized that a majority of patients diagnosed with alcohol dependence would not receive alcohol withdrawal prophylaxis.
Methods>
Sample
Subjects for this study were identified from among participants in a longitudinal study of outcomes of care for schizophrenia (
9). Subjects who were included in the study met
DSM-III-R criteria for schizophrenia as confirmed by the Structured Clinical Interview for DSM-III-R (SCID) (
20), were between 18 and 55 years old, and provided written informed consent. The SCID is a diagnostic tool that can be used in clinical settings to ensure that all diagnoses are systematically evaluated (
20). The SCID was administered by a trained clinical research assistant who is a licensed clinical social worker. Subjects also had to meet
DSM-III-R criteria for a current substance use disorder as determined by the SCID. All subjects had a lifetime diagnosis of a substance use disorder, with substance use in the past 30 days. All treating physicians were blind to the structured-interview diagnosis of a substance use disorder.
Subjects were recruited between February 1992 and May 1993 from the acute psychiatry inpatient units of two facilities, the Little Rock Veterans Affairs Medical Center, a 276-bed tertiary care facility, and Arkansas State Hospital, the primary inpatient facility for the state's mental health system, with approximately 200 beds. Records of previous services received from the VA medical center, including diagnosis and treatment of a substance-related disorder, were available to inpatient providers on request. Admission to the state hospital for acute psychiatric care required a screening and referral from the patient's local mental health center. The screening provided information on the patient's current symptoms and history, including psychiatric and substance-related diagnoses.
Forty-two patients with SCID-confirmed diagnoses of both schizophrenia and a current substance use disorder were included in the study. Three additional subjects from the longitudinal study who met the inclusion criteria were not included in the study reported here because medical records were not available. These subjects did not differ from the included subjects in age, race, duration of illness, educational level, or employment status.
Twenty-three patients (55 percent) were enrolled from Arkansas State Hospital and 19 (45 percent) from the VA medical center. The patients from the two facilities did not differ significantly in age, race, duration of illness, educational level, or employment status. The mean± SD age of the sample was 37.3±5.8 years. The mean duration of illness was 13.2± 8.5 years. The sample included 40 men (95 percent) and two women (5 percent). The women did not differ from the men in the areas evaluated and therefore were not excluded from the study. Twenty-four patients (57 percent) were African American, and 18 (43 percent) were Caucasian.
Instrument and procedures
Medical records were reviewed by a physician (the first author) to examine two areas of the inpatient process of care—the admission evaluation and inpatient management, including disposition. Specific areas reviewed were admission diagnosis, laboratory toxicology screens obtained on admission, alcohol withdrawal prophylaxis, substance abuse treatment focus in the patient's treatment plan, referral to substance abuse treatment during inpatient hospitalization, discharge diagnosis, and referral to outpatient substance abuse treatment at discharge.
The provision of prophylaxis for alcohol withdrawal was defined as an order for benzodiazepines, either scheduled or as needed (
21,
22), and one or more of the following: an order for thiamine, an order for frequent monitoring of vital signs, or an order for an assessment of subjective signs of withdrawal.
Data analysis included two components, descriptive analysis of SCID diagnoses and elements from the medical record review and comparison of demographic and clinical characteristics of subjects who received a substance use diagnosis at discharge and those who did not. Chi square and two-tailed t tests were used. The significance level was set at .05.
Results
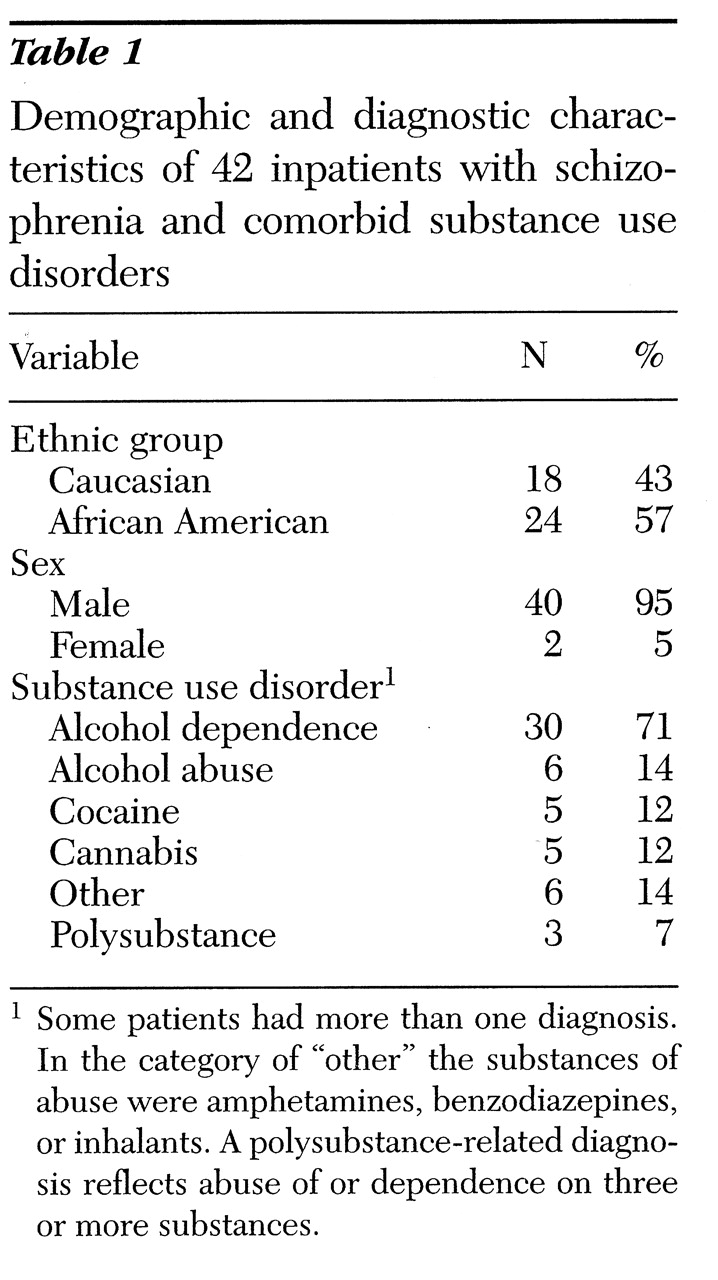
Table 1 shows the frequency of SCID substance use diagnoses for all subjects. Some patients had more than one diagnosis; 32 (76 percent) met criteria for only one substance use disorder, and ten (24 percent) met criteria for two or more. Alcohol use disorders were the most frequent, with 30 patients meeting diagnostic criteria for current alcohol dependence and six for alcohol abuse. Five patients had a cocaine use disorder, and five had a cannabis use disorder.
The medical record review revealed that in this sample of patients with SCID-confirmed dual diagnoses, 24 patients (57 percent) did not receive an admission diagnosis of a substance use disorder. A urine drug screen was completed on admission for 38 (90 percent) of the patients. Alcohol screening tests, either a blood or urine alcohol concentration test or a breath analysis test, were obtained for 28 patients (67 percent). At discharge, substance use diagnoses were not recorded for 19 of the patients (45 percent). Alcohol use disorders were the most frequently missed diagnoses; 17 (47 percent) of the 36 patients with SCID-confirmed alcohol use disorders did not receive a substance use discharge diagnosis.
Demographic characteristics of patients with and without a diagnosis of a substance use disorder at discharge were compared. Caucasians were less likely to receive a comorbid substance use diagnosis (39 percent) than African Americans (67 percent), although the difference was not statistically significant (p=.07). Patients who did not receive a discharge diagnosis of a substance use disorder had significantly fewer years of education than subjects who did (mean of 11.2 years versus 12.8 years; two-tailed t test, t=-2.6, df=37, p<.05).
Review of the management of substance use disorders revealed that alcohol withdrawal prophylaxis was ordered for ten (33 percent) of the 30 subjects with a SCID-confirmed diagnosis of current alcohol dependence. For 28 patients (67 percent), the substance use disorder was addressed in treatment planning, and 16 (38 percent) were referred for inpatient substance abuse treatment during their inpatient hospitalization. Referral to outpatient substance abuse treatment at discharge was documented in eight (19 percent) of the records.
Discussion and conclusions
Overall, the results of this study indicate that among patients with schizophrenia and a comorbid substance use disorder who were hospitalized on psychiatry units, the substance use disorder was frequently undetected. Although this finding is not surprising, it does suggest a need for improvements in the quality of care delivered to this population. In this sample of patients whose diagnoses of both schizophrenia and a substance use disorder were confirmed by a structured clinical interview, 85 percent had an alcohol use disorder. This result is consistent with findings of other studies.
For patients with schizophrenia who have a substance use disorder that has not been clinically identified, alcohol is the most common substance of abuse (
2,
6,
8). Despite extensive research findings of a high prevalence of alcohol use disorders among patients with schizophrenia, these disorders frequently are not recognized or documented in the clinical setting and, as we found, are often not adequately managed by clinicians (
2,
13,
19).
Although the substance use disorder was addressed in treatment planning for a majority of the patients in our study (67 percent), only 38 percent received a documented referral to inpatient substance abuse treatment during hospitalization, and only 19 percent received a referral for outpatient substance abuse treatment at discharge. Explanations for these findings are not immediately apparent because facilities in our study had adequate treatment options to which to refer patients with substance use disorders. At the time of the study, the VA medical center had specialized inpatient and outpatient treatment programs for patients with a dual diagnosis in addition to standard psychiatric programs.
Substance abuse treatment and mental health services at the state hospital existed as parallel systems of care. Therefore, to enter substance abuse treatment, the patient required a specific referral by the inpatient or outpatient mental health provider. Nonetheless, these findings are consistent with those of Brady and colleagues (
23), who reported that fewer than half of psychiatric inpatients who have a current or past history of a substance use disorder also receive inpatient or outpatient treatment for the disorder. In their study, patients with schizophrenia were the least likely to receive such treatment.
In our study, neither age nor duration of illness was associated with the SCID-confirmed diagnosis of a comorbid substance use disorder. Subjects who received a substance use discharge diagnosis had more years of education, although the difference between groups was less than two years. Although racial differences in discharge diagnoses were not statistically significant in our study, they are similar to those in a recent report by Strakowski and associates (
24), who found that of 490 patients seen by a psychiatry emergency service, African-American patients were significantly more likely than Caucasian patients to be diagnosed as having both schizophrenia and a substance use disorder.
In our opinion, the most clinically pertinent findings of this study are the lack of documentation of a substance use diagnosis by the inpatient physician and the lack of referral to outpatient substance abuse treatment at the time of discharge. In providing continuity of care, the discharge diagnosis is a primary method of communication between inpatient and outpatient care settings. Although the design of our study did not allow for definitive conclusions about these issues or causal explanations, our results do suggest that future research should examine why these disorders go undocumented and unmanaged in acute settings. Possibilities might include an examination of whether clinicians feel a lack of "ownership" for treating the disorder (
25), or whether they lack knowledge of a formal method for detecting and diagnosing substance use disorders (
11,
26).
In addition, patients who require an acute psychiatric hospitalization may be unwilling to provide a reliable history or may be unable to do so because of cognitive impairment (
11,
17). Future research is needed to explore the ability or willingness of patients with schizophrenia to provide an accurate substance use history. This information, coupled with vigilant laboratory documentation, will help provide essential data for clinicians to accurately detect, diagnose, and treat comorbid schizophrenia and substance use disorders.
Another implication of these results for future research and education is the lack of clinical recognition and management of current alcohol use disorders on acute psychiatry units. Orders for alcohol withdrawal prophylaxis were not given for 20 subjects with SCID-confirmed current alcohol dependence (67 percent). Although our study found no evidence that the lack of such orders led to poor outcomes, prophylaxis orders do indicate the provider's awareness of a possible alcohol use disorder and the intention of careful monitoring.
Limitations of our study include that it was performed in the context of a larger longitudinal study and therefore had a fixed sample size. In addition, the study included only two women, thus limiting the generalizability of our findings. The public-sector sites from which our patients were enrolled treat large numbers of patients with schizophrenia; however, these hospitals and their patients have some unique characteristics. Thus the results may differ in a general hospital psychiatric unit or a freestanding psychiatric facility.
Despite its limitations, this descriptive study is a valuable addition to the growing literature on the assessment and treatment of persons with co-occurring addictive and mental disorders. To our knowledge, this is the only study that has examined inpatient and discharge management in a patient population identified by a structured clinical interview in which the treating physician was blind to the comorbid substance use diagnosis. In addition, this study emphasizes the need for sustained vigilance in assessing the possibility of comorbid diagnoses in all patients.
Acknowledgment
The authors thank Doris Hutchins, L.C.S.W.