The new atypical antipsychotic medications represent major innovations in the treatment of schizophrenia and other psychoses (
1,
2). But the new medications cost more, and their widespread use may be discouraged in both public and private finance systems because older medications may be prescribed for a small fraction of the cost. Pharmacoeconomic analysis has become an important strategy in determining whether costs associated with newer pharmacotherapeutic agents are offset by clinical outcomes and associated cost savings in other areas (
3,
4,
5,
6).
Clozapine, the first of the atypical antipsychotic medications to appear on the U.S. market, is effective for the treatment of refractory psychosis (
7,
8,
9). However, it has been utilized with as few as 5 percent of eligible patients who have not responded to traditional neuroleptics (
10). Among the factors accounting for this lack of use may be clozapine's cost and the need for blood monitoring, which may make it prohibitive for all but the most treatment-resistant patients.
Previous studies have provided support for the cost-effectiveness of clozapine among subjects recruited in the hospital. Overall, the higher costs of clozapine treatment have been offset by decreased hospitalization, although two years' follow-up may be required for the net savings to become evident (
8,
11,
12,
13,
14,
15). The development of community-based clozapine programs suggests the need for further economic analysis of initiating clozapine treatment in the community (
10,
16,
17,
18).
The study reported here was designed to address this issue. We sought answers to several questions about patterns of service utilization and costs associated with clozapine initiated in a community clinic. Do patients who initiate clozapine in the community decrease their hospital utilization? Do the costs associated with outpatient services and maintenance in the community increase substantially? What is the net effect on overall cost of treatment for these patients? And finally, do the anticipated savings in hospital care fully offset the added costs of community-based treatment?
Methods
The patient sample was recruited from Community Counseling Centers of Chicago, an urban community mental health center with an outpatient clozapine program that has been in operation since 1991. The clozapine clinic serves a large multiethnic population (N=462); most of them (89 percent) initiated clozapine in the hospital, as indicated by a chart review of 95 randomly selected patients.
The study included all patients from the clozapine clinic who had a diagnosis of schizophrenia or schizoaffective disorder, were at least 18 years of age, had begun their clozapine treatment in the community, and whose records provided at least a year's information on service utilization before and after initiation of clozapine treatment. All patients met the following inclusion criterion: they had been treated unsuccessfully with at least two traditional neuroleptic agents before starting clozapine, with treatment being discontinued due to clinical inefficacy, tardive dyskinesia, or other major side effects.
Subjects' charts were reviewed by one of the authors (LL) to obtain information on the patients' demographic and clinical characteristics, the types of services they received, the duration of the services, and professional disciplines of service providers. Independent chart ratings by another experienced researcher indicated that interrater agreement on service utilization was high (.99). Chart review information on hospitalization was cross-checked with hospitalization data from the Illinois Department of Human Services database and found to be in complete agreement.
Costs were computed in 1996 dollars. Medication costs for clozapine were based on current drug costs plus Medicaid charges for laboratory work. The cost of traditional neuroleptics was computed based on state averages from the Department of Human Services pharmacy database. Private hospital costs were computed on the basis of metropolitan Medicaid per diem rates, and state hospital costs were computed on the basis of per diem estimates provided by the department. Community treatment costs were estimated using Medicaid reimbursement rates for specific services and the duration provided.
Based on an intent-to-treat approach, costs were calculated for all patients who received clozapine whether or not they completed the full year of treatment. Because it was predicted that hospital utilization would decrease after initiation of clozapine treatment, changes in the number of hospital admissions and in the number of hospital days were analyzed using the nonparametric Wilcoxon matched-pairs signed-ranks test, one-tailed.
Results
Of the 28 patients who met criteria for inclusion in the study, 21 remained on clozapine for a year, and seven discontinued the medication. Length of treatment in days for the seven patients who dropped out was as follows: 34, 35, 48, 90, 104, 104, and 150. Although data on the exact reason for discontinuing clozapine were not available for these patients, anecdotal information from the prescribing psychiatrist suggested that the major reasons included side effects and medication nonadherence.
The majority of patients had a diagnosis of schizophrenia (21 patients, or 75 percent), and the remainder had a diagnosis of schizoaffective disorder (seven patients, or 25 percent). The sample included more male patients than female patients (16 males, or 57 percent, and 12 females, or 43 percent). More than half were Caucasian (15 patients, or 54 percent); the remainder were Hispanic (seven patients, or 25 percent), African American (four patients, or 14 percent), Asian (one patient), and Native American (one patient).
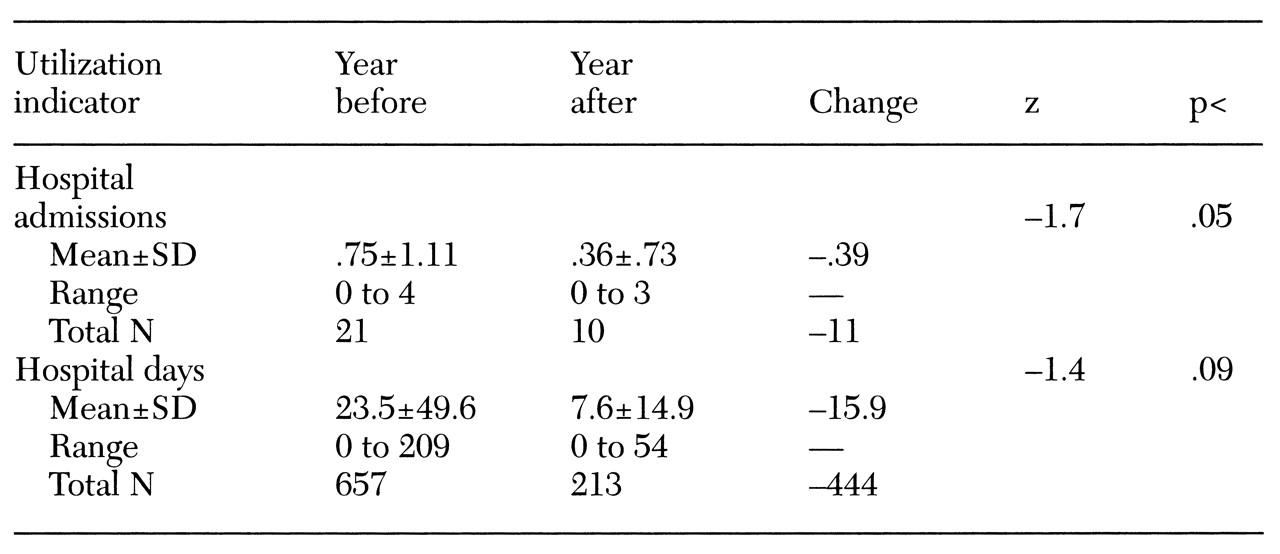
Table 1 presents data on hospital utilization for the year before and the year after initiation of treatment with clozapine for all 28 patients. In the year before starting clozapine, the patients collectively had a total of 21 hospitalizations, with a range from zero to four hospitalizations and a mean±SD of .75±1.11 hospitalizations per patient. In the year after the start of clozapine treatment, the total number of hospitalizations dropped to ten, with a range of zero to three and a mean of .36±.73 per patient (z=-1.70; p<.05). In the year before starting clozapine, patients spent an average of 23.5±49.6 days in the hospital; during the clozapine treatment year, hospital stays averaged 7.6±14.9 days, a two-thirds reduction approaching statistical significance (z=-1.40; p=.081). The number of patients who were admitted to the hospital decreased from 13, or 46 percent, in the baseline year to seven, or 25 percent, during the clozapine treatment year.
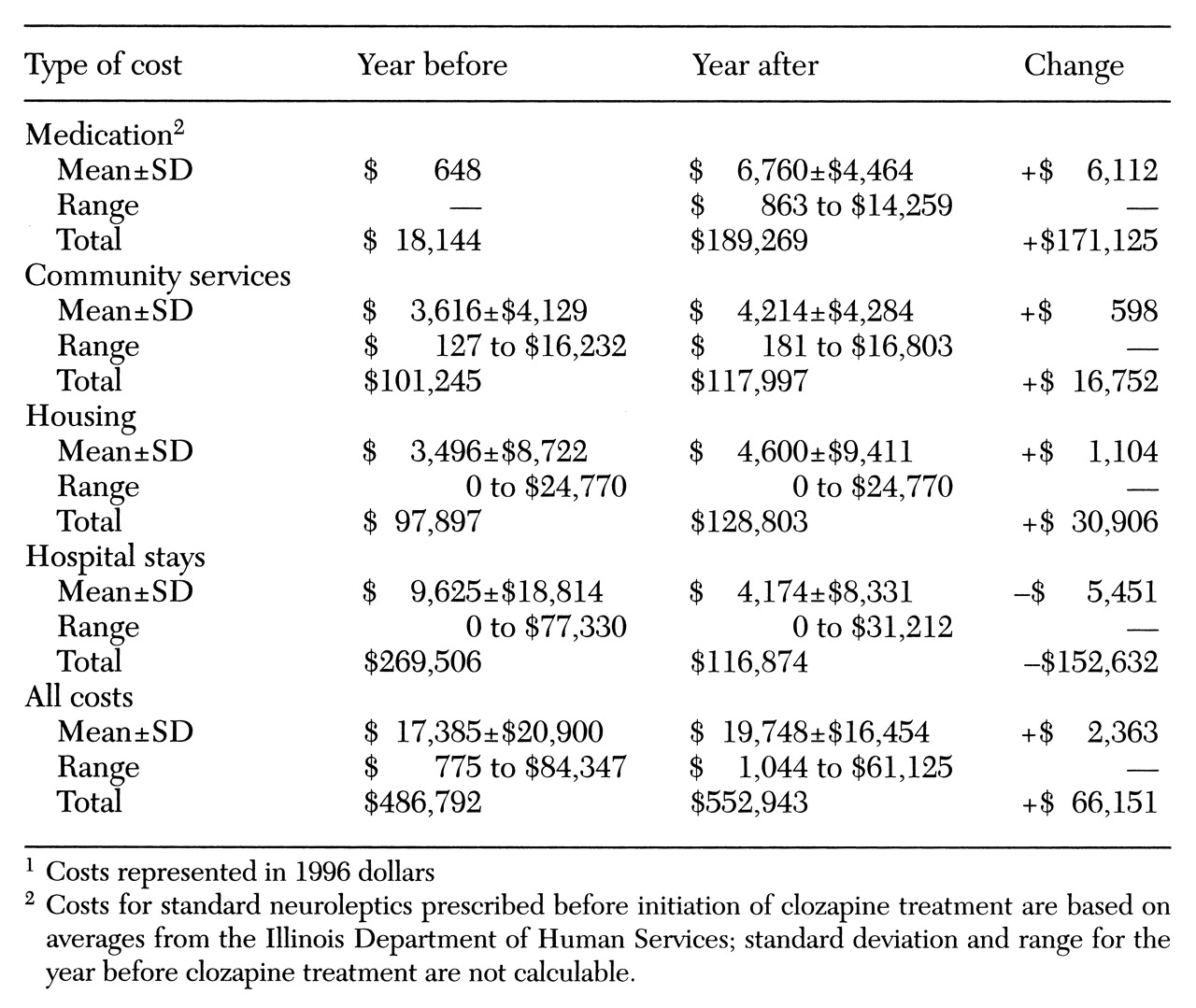
Table 2 shows the service utilization costs associated with initiation of clozapine treatment for all 28 patients on an intent-to-treat basis. The costs associated with hospitalization were more than cut in half, from a mean of $9,625 to a mean of $4,174 per patient. For the patient sample collectively, the total costs of hospitalization decreased from $269,506 to $116,874, for a total savings of $152,632.
Annual medication costs for clozapine, including weekly blood tests, came to an average of $6,760 per patient. By comparison, the annual cost of traditional neuroleptics, at $1.78 a day, averaged $648 per patient. The net increase of $6,112 a year per patient translates into a total cost increase of $171,125.
As for community services, the cost of nonmedical community services used by the patients decreased from an average of $3,375 in the baseline year to $2,872 in the clozapine treatment year. However, costs of medical community services related to the use of clozapine, including physician visits and medication monitoring, increased nearly sixfold from a mean of $241 to $1,342. The net increase per patient in the overall cost of outpatient services during the clozapine treatment year averaged $598, with the cost of outpatient services increasing from $3,616 in the baseline year to $4,214 on clozapine. For the sample, this difference translated into a total increase in the cost of community services of $16,752, from $101,245 before clozapine to $117,997 during clozapine treatment.
Relatively few patients used housing that was subsidized by the state of Illinois either in the year before clozapine treatment (N=4) or during the year of clozapine treatment (N=7). The total cost of this housing increased from $97,897 during the baseline year to $128,803 during the clozapine year, a $30,906 increase. Mean subsidized housing costs increased from $3,496 in the baseline year to $4,600.
The sum total of the above costs, including hospital, medication, community services, and housing costs, was $486,792 for the year before clozapine treatment and $552,943 during the clozapine treatment year, which represents an increase in total costs of $66,151 for this patient sample. The mean of total costs per patient before clozapine treatment, $17,385, increased by $2,363 to $19,748 during clozapine treatment. In terms of cost offset, the additional costs associated with clozapine during the first year of outpatient-initiated treatment ($218,783) were 70 percent offset by the savings in institutional care ($152,632).
Discussion and conclusions
The study reported here differs from most previous reports of service utilization associated with clozapine treatment by focusing on patients whose clozapine treatment was initiated in the community, rather than in the hospital. The results indicated first that even in a large community-based clinic, only a small minority of patients treated with clozapine started taking the medication on an outpatient basis.
Patterns of service utilization among these patients did show evidence of change in the predicted direction during the first year of clozapine treatment. Fewer patients were hospitalized during that year, and the total number of hospital admissions was cut in half. The corresponding per-patient hospitalization rate was significantly lower during the clozapine treatment year than in the baseline year. Bed days of hospital care dropped by nearly 70 percent during the first year of clozapine treatment, and this finding was associated with a decrease in hospitalization costs of well over 50 percent. The difference in mean days of hospital care approached statistical significance. A slight increase in the cost of community outpatient services was found, related primarily to medical monitoring of clozapine treatment. Similarly, there was a marginal increase in total treatment costs. Overall, the additional costs associated with clozapine were substantially, although not completely, offset by savings in institutional care during the first year of treatment.
Previous studies have addressed the issue of the cost-effectiveness of clozapine treatment for neuroleptic-resistant patients (
8,
1112131415). A number of the studies have been limited not only by the use of mirror-image or pre-post designs but also by the lack of data on patients who dropped out of clozapine treatment. The absence of such information makes it difficult to assess the impact of the decision to start clozapine treatment on service utilization and associated costs for patients who meet entry criteria for a trial of clozapine. An intent-to-treat approach, assessing service utilization and costs during follow-up for all patients started on clozapine, including those who discontinue the medication, attempts to recover additional information about the overall impact of the decision to treat.
Briefly, earlier studies provided evidence of dramatic reductions in hospital utilization and associated costs for patients who continued to be followed up in treatment on clozapine, although cohort size usually decreased substantially over time. Revicki and associates (
11) compared patients with schizophrenia who were treated with clozapine for at least a year with a matched group of patients who received standard neuroleptic treatment. They found that although treatment costs changed little in the first treatment year, the overall cost of treatment for clozapine-treated patients decreased significantly by the second year of treatment. A similar pattern of decreased hospitalization, decreased hospital costs, and increased cost savings over time was detected in several other mirror-image studies that included patients who started clozapine in the hospital (
8,
12,
14,
15). Savings were particularly likely to be realized by the second year of treatment.
In a study that incorporated an intent-to-treat analysis, Meltzer and associates (
13) evaluated treatment costs for neuroleptic-resistant patients with schizophrenia during the two years before and the first two years after initiation of clozapine treatment in a university hospital setting. They reported significantly decreased overall costs of treatment for clozapine-treated patients, with cost savings accounted for primarily by decreased hospitalization. It is important that they also provided cost data on patients who dropped out of clozapine treatment. Separate analysis showed that the patients who dropped out continued to have high rates of hospital utilization and that the total costs of treatment for these patients increased. However, an intent-to-treat analysis calculating the mean cost per patient for all patients who were started on clozapine—including those who dropped out and were frequent utilizers of hospital services—showed a substantial decrease in total mental health care costs compared with the preclozapine period. Significantly, this study demonstrated the rising cost of care for patients who drop out of clozapine treatment and the net cost savings associated with the decision to prescribe clozapine even when those whose treatment fails in the first two years are included in the cost analysis.
Also using an intent-to-treat design was the prospective "real-world" medical effectiveness study by Essock and colleagues (
19), in which state hospital patients with schizophrenia or schizoaffective disorder were randomly assigned to receive clozapine treatment on an open-label basis or usual care, including an assortment of conventional neuroleptics. The findings indicated that although the two groups of chronically hospitalized patients did not differ in the likelihood of being discharged over time, once patients who received clozapine were discharged from the hospital, they were much less likely to be readmitted than the usual-care patients, and they accrued more days in the community over the two-year follow-up. Because this study made no effort to control clinical practice beyond random treatment assignment, the results may provide the best estimate of service utilization and clinical outcome after the decision to prescribe clozapine for a population of chronically hospitalized patients with schizophrenia.
More recently, a British study reported on service utilization and costs associated with outpatient clozapine treatment of patients with schizophrenia or schizoaffective disorder (
20). Using an intent-to-treat approach, the authors collected data for the three-year period before clozapine treatment was initiated and for a minimum of one year afterward (mean=36.4 months). Service utilization data revealed a decrease in hospital days per year during clozapine treatment, compared with the period before clozapine use, and an increase in use of community-based services. Although housing as well as medication costs increased with clozapine treatment, total costs showed a statistically nonsignificant decrease. A cost-effectiveness ratio, computed as the Quality of Life Scale score (
21) divided by the total treatment cost per year, showed that the cost-effectiveness of treatment during the clozapine period was more than double the cost-effectiveness of treatment before clozapine was started.
The study reported here, which also used a mirror-image design and an intent-to-treat approach, has provided data suggesting a pattern of decreasing hospital utilization early in the course of outpatient-initiated clozapine treatment. This information is of particular interest because the baseline hospital utilization in this outpatient clinic sample clearly differs from that of patients in a number of the studies of clozapine treatment started on an inpatient basis. The decrease in hospitalization observed in the study substantially, although partly, offset the increased expense of outpatient care.
In a Swedish study assessing cost-effectiveness of clozapine treatment for treatment-refractory patients with schizophrenia over an 18-month period, Jonsson and Walinder (
22) found that inpatient treatment costs decreased absolutely and as a proportion of overall treatment costs while the cost of outpatient care increased, leading to an overall increase in treatment cost of 10 percent. The authors suggested that the increase in total treatment cost could be best understood as a short-term expense; their analysis of data from the outpatient phase of treatment suggested that clozapine treatment is cost-effective for maintenance therapy. The short-term increase in overall treatment cost associated with clozapine is not incompatible with the findings of other studies that have suggested major cost reductions over longer-term follow-up periods (
8,
11,
12,
1314,
15). The importance of weighing the long-term benefits and probable cost savings against the short-term expense has been emphasized (
23).
In interpreting the results of the study reported here, certain limitations should be kept in mind. The mirror-image design is not as rigorous and conclusive as a randomized, controlled prospective study. It is possible that trends toward decreasing use of hospital care in the community at large could confound the decrease in hospitalization that we have attributed to clozapine. However, patients in the study were prescribed clozapine over a four-year time period, and in assessing trends over time, we noted that for any given year the hospital utilization of the clozapine treatment group was lower than hospital utilization of the pretreatment group. This finding supports the view that decreased hospital use was due to clozapine, rather than to an overall trend. Finally, indirect costs such as lost work and disability payments are important considerations but were not measured in this study.
The study provided evidence of a cost-offset process at work in the first year of outpatient-initiated clozapine treatment. In contrast to the study by Aitchison and Kerwin in the United Kingdom (
20), the added cost of clozapine was only partly offset. The fact that only two of the 26 patients they studied dropped out of treatment, compared with seven of the 28 patients in our study, might account for the added cost savings. The availability of clozapine for these patients makes a difference in service utilization patterns and may result in longer-term cost savings for this less severely ill, noninstitutionalized population.
Other new antipsychotic agents such as risperidone and olanzapine have become attractive to many clinicians and patients as potential first-line drugs because their side-effect profiles appear to be superior to those of the older neuroleptics. Considering the expense of chronic care and the longer-term costs of medication-adherence difficulties, further pharmacoeconomic research focused on outpatient-initiated treatment with these newer agents may demonstrate cost savings that are more substantial than those reported to date.
Acknowledgments
This study was supported by a home health care research grant from the University of Chicago to Dr. Luchins. The authors thank David Meltzer, M.D., Ph.D., for his review of the manuscript and consultation on pharmacoeconomic methodology.