The Department of Veterans Affairs (VA), like other branches of the government, is under increasing pressure to reduce costs (
1). However, veterans remain a highly valued political constituency, demanding high-quality health care, including substance abuse treatment (
2,
3). Thus VA has been seeking to provide high-quality services to veterans while at the same time cutting costs and eliminating wasted resources involved in providing these services.
This study had two competing hypotheses. One was that VA programs are pushed toward the legitimate form as a result of external pressure to produce both high-quality and more streamlined treatment, as well as uncertainty about how to achieve these outcomes. The second hypothesis was that cost is the primary concern of administrators, and that programs that are more expensive to operate, regardless of quality, are at greater risk of closure and, if they survive, are more likely to be pushed into line with programs of similar cost.
Methods
Data
Data were derived from two surveys of coordinators of VA substance abuse treatment programs: the Drug and Alcohol Program Structure Inventory (DAPSI) (
14) and the Drug and Alcohol Program Survey (DAPS) (
15). DAPSI obtained organizational data on the population of 273 VA substance abuse treatment programs for fiscal year 1990. DAPS gathered organizational data on the population of 389 VA substance abuse treatment programs for fiscal year 1994, including 223 programs assessed previously in 1990. In fiscal year 1994, a total of 166 new programs existed that did not exist in fiscal year 1990.
Both surveys were administered by the VA Program Evaluation and Resource Center. All surveys were completed and returned, for a 100 percent completion rate. In this report, inpatient and outpatient programs are examined separately.
Program closure and change
To test the competing hypotheses, three dichotomous variables were examined for fiscal years 1990 and 1994. The first was program closure, measured as either closure or survival of a program from fiscal year 1990 to fiscal year 1994. Program change was measured by two dichotomous variables, staff cuts and change in treatment type. Staff cuts in fiscal year 1994 measured whether a program received any cuts in the past year. Change in treatment type from fiscal year 1990 to fiscal year 1994 measured whether programs provided different types of treatment over time.
Treatment types
The types of treatment measured in inpatient and outpatient programs were 12-step groups, behavioral treatment, and training in daily living skills. Behavioral treatment consisted of social skills training, stress management training, and recreational therapy. Daily living skills training consisted of family therapy and vocational rehabilitation therapy. In some cases, combinations of the dominant types emerged, such as 12-step programs with behavioral elements. In some programs, no single treatment type dominated, and the programs were low in all three dimensions, which may have indicated the lack of a dominant treatment philosophy. Some outpatient programs also offered methadone maintenance, which was considered a fourth type of treatment. If a program changed from an inpatient to an outpatient format, it was considered a program closure in 1990 and a new program in 1994.
The type of treatment was assessed by converting several continuous measures of treatment services into dichotomous variables and then identifying patterns of responses across dimensions (
16). Treatment services were initially assessed by the percentage of patients involved in relevant treatment activities.
Staff types
Program staff were categorized as doctoral-level staff, nursing staff, and daily living staff. Doctoral-level staff included physicians, psychiatrists, and doctoral-level psychologists. Nursing staff consisted of registered nurses, nurse practitioners, physician assistants, licensed vocational nurses, and licensed practical nurses. Daily living staff consisted of addiction counselors, vocational counselors, and social workers. Consistent with the identification of treatment types, staff types were created based on patterns of available staff members within each program.
Enhancement funding
Congress provided $60 million for enhancement and expansion of VA substance abuse treatment programs in 1990 and an additional $15 million over the prior year's allocation in each subsequent year from 1991 to 1993. This money was to be used to develop new programs and increase staffing and treatment resources (
14). Receipt of enhancement funds represents a form of legitimization of the program by demonstrating its adherence to a known environmental goal.
Program coordinator characteristics
Two other independent variables assessed characteristics of the program coordinator. The first, program coordinator status, was treated as an indicator of legitimacy, given that a program coordinator should have a strong impact on the form the program takes and how legitimate it appears within the facility (
10). A dichotomous variable was created for whether or not the program coordinator held a doctoral-level degree.
The second dichotomous independent variable was the relative position of a program coordinator, or whether a coordinator was responsible for coordinating program activities only or was also a director of services related to substance abuse treatment. The latter role indicates a higher and, presumably, more powerful position.
Staff costs
Costs of staff represent the main alternative to legitimacy factors as an explanation for program closure and change. It was assumed that other facility-level costs were constant across sites and that staff costs accounted for most of the variation in program cost. Staff costs were measured as the number of staff, by position, multiplied by the average national salary for that position. The total costs of all staff for each program were calculated. Costs of administrative or secretarial staff were not included.
Costs of treatment staff at each facility based on national averages were maintained by VA through centralized accounting for the local management file and the cost distribution report. Cost totals for fiscal year 1990 were adjusted to fiscal year 1994 dollars. Fiscal year 1990 salary dollars were adjusted to fiscal year 1994 dollars using the Consumer Price Index for Urban Consumers. The 1990 index was 130.7, and the 1994 index was 148.2. Dividing 148.2 by 130.7 yields an adjustment term of 1.13, or approximately a 13 percent wage adjustment. Staff cost data were transformed with a natural logarithmic transformation (
17).
Results
Separate logistic regressions for inpatient and outpatient programs were tested. Because the results are estimated in log odds, the interpretation of the effect is in the form of odds ratios (
18). For log total staff cost, the only continuous variable, the odds ratio is not given because of inflated values, due to the log transformation of a logged variable (
19). (In a separate analysis, region of the country where the facility was located was not found to be related to any outcomes for inpatient or outpatient programs.)
Basic program characteristics
A total of 273 VA substance abuse treatment programs were operating in fiscal year 1990, of which 59 did not survive to fiscal year 1994. Thirty-eight were inpatient programs, and 21 were outpatient programs. Of the 38 closed inpatient programs, four changed treatment format and became outpatient-only programs by 1994. These programs were treated as closures in 1990 and new programs in 1994, as were five of the 21 outpatient programs closed in 1990 that began providing inpatient treatment by 1994.
Most other surviving inpatient programs made no changes in treatment setting, although 22 percent added outpatient services to their inpatient format, and 12 percent dropped outpatient services.
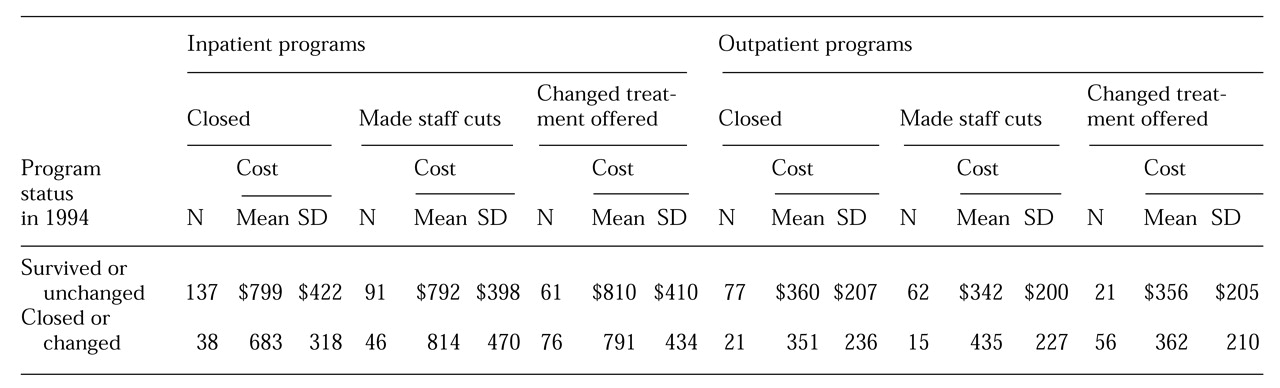
Staff costs
Table 1 shows staff costs for fiscal year 1994 for programs that survived or that did not change the type of treatment offered between 1990 and 1994 and for those that closed or that changed treatment type. It also shows staff costs for the programs in both groups that made staff cuts. No statistically significant differences in staff costs were found between any of these programs—that is, between those that closed, those that changed treatment type, or those that made staff cuts. This finding held for both inpatient and outpatient programs.
Closed programs tended to be less costly than surviving programs, and programs that made staff cuts tended to be more costly, although the differences were not statistically significant. These findings suggest that costs alone cannot account for organizational change and point to a more complex strategy by decision makers determining organizational structure.
Inpatient programs
In fiscal year 1990, a total of 175 VA inpatient substance abuse treatment programs were operating. Of those programs, 137 (78 percent) survived, and 38 (22 percent) closed. Thirty-four percent of the 137 surviving programs made staff cuts, and most (56 percent) changed the type of treatment provided.
Among inpatient programs, a trend was noted for more of the surviving programs to have received enhancement funding compared with the programs that closed, although the difference was not statistically significant. No other differences between the closed and surviving inpatient programs were significant, and the multivariate analysis did not yield predictors of programs that closed or survived.
An additional model was tested in an effort to explain program closure among the inpatient programs, using a dichotomous variable indicating whether the program was the only inpatient substance abuse treatment program at that VA facility. This model was based on the rationale that eliminating inpatient substance abuse treatment programs is a cost-saving measure but that removing all such programs from a facility threatens legitimacy, because no inpatient services would be provided for a serious health problem among veterans. By allowing at least one program to survive, both cost savings and legitimacy concerns might be satisfied.
The results from the logistic regression model indicated that lone programs within a facility were significantly less likely to close. Being a lone program reduced the likelihood of program closure by a third (coefficient=-.53, SE=.19, odds ratio=.35, p<.01; model χ2=7.92, df=1, p<.01; R2=.04, N=175).
No significant differences were noted between inpatient programs that made staff cuts and those that did not. The logistic regression analysis did not yield any predictors of which inpatient programs made staff cuts and which did not.
Inpatient programs that offered 12-step groups with behavioral elements in 1990 were significantly less likely in 1994 to have changed treatment type than programs that offered other types of treatment in 1990. Seventy-four percent of the inpatient programs that remained unchanged offered 12-step groups, compared with 29 percent of programs that changed (χ2=27.2, df=1, p<.01).
This finding held for the logistic regression analysis. Programs that offered 12-step groups with behavioral elements were significantly less likely to change treatment type; the likelihood of change was reduced by a tenth. The overall model was significant, explaining 17 percent of the variance in treatment type change (coefficient=-1.09, SE=.22, OR=.11, p<.01; model χ2=31.65, df=6, p<.01; R2=.17, N=137).
Outpatient programs
In fiscal year 1990, a total of 98 VA outpatient substance abuse treatment programs were operating. Of that number, 77 (79 percent) survived, and 21 (21 percent) closed. Nearly 20 percent of surviving programs made staff cuts. Seventy-three percent of programs changed the type of treatment offered.
Bivariate comparisons indicated that outpatient programs that closed were significantly more likely to have program coordinators who held doctoral degrees and were significantly more likely to offer the most prevalent type of treatment, 12-step groups. Eighty percent of outpatient programs that closed had program coordinators with doctoral degrees, compared with 45 percent of the surviving programs (χ2=7.3, df=1, p<.01). Sixty-seven percent of closed outpatient programs offered 12-step groups, compared with 33 percent of surviving programs (χ2=8.1, df=1, p<.01).
Results of logistic regression analysis confirmed those findings. Programs in which the coordinator held a doctoral degree were more than six times more likely to close than those in which the coordinator did not have a doctoral degree (coefficient=.92, SE=.36, OR=6.36, p<.01; model χ2=20.99, df=6, p<.01; R2=.21, N=98). Moreover, programs offering the prevalent treatment type were nearly six times more likely to close than those offering other types of treatment. The overall model was significant and explained 21 percent of the variance (coefficient=.88, SE=0.30, OR=5.79, p<.01; model χ2=20.99, df=6, p<.01; R2=.21, N=98).
The finding that outpatient programs offering the prevalent treatment type were more likely to close might be explained by a shift toward other treatment philosophies, specifically, treatment low on all dimensions. In a separate analysis, programs offering treatment low on all dimensions were less likely to close, although the finding was not significant in the multivariate model. A program that measures low on all dimensions may provide care that is customized to individual patients, rather than having an overarching treatment philosophy applied to all patients. This explanation is consistent with VA's goal of matching treatment to the needs of patients.
The finding that outpatient programs in which the program director held a doctoral degree were significantly more likely to close might relate to a cost variable rather than, or in addition to, a legitimacy variable, as staff at this level earn substantially more than other staff.
No significant differences across predictors were found between outpatient programs that made staff cuts and those that did not. The logistic regression analysis did not yield predictors of which outpatient programs made staff cuts and which did not.
Outpatient programs with coordinators who held a doctoral degree were less likely to change treatment type. Sixty-two percent of the programs that did not change treatment type had a program coordinator with a doctoral degree, compared with 36 percent of programs that did change treatment type (χ2=4.3, df=1, p<.05).
This finding was supported by a trend found in the logistic regression analysis, although the effect was not statistically significant. No other predictors of which outpatient programs changed treatment type were statistically significant.
The trend toward a change in treatment type in outpatient programs with a coordinator who held a doctoral degree is contrary to the finding of a higher likelihood of closure among programs in which the coordinator held a doctoral degree. The results suggest a possible cost-related effect on program closure and a legitimacy-related effect on program change.
Discussion and conclusions
For both inpatient and outpatient substance abuse treatment programs, staff costs were not related to closure, staff cuts, or change in treatment type, and the cost differences between surviving programs and those that closed or changed were small. Closed programs were actually less expensive than surviving programs. Legitimacy is but one possible alternative explanation.
For inpatient programs, closure was associated with having more than one program at a single VA facility, suggesting a combination of cost and legitimacy factors. At these facilities the number of programs could be reduced in order to lower costs as long as at least one program remained open for purposes of legitimacy. Program change was associated with initially offering treatment other than the prevalent type, 12-step groups with behavioral elements. Again, legitimacy seems to play a role here because programs that adhered to the legitimate form were more likely to retain their form over time.
For outpatient programs, closure was associated with offering the prevalent treatment (12-step groups) and having a program coordinator with a doctoral degree.
VA guidelines for substance abuse treatment during this time period were to offer more individualized treatment of no dominant type. A trend was noted for programs that adopted the guidelines to be less likely to close. Although more evidence is needed to determine whether the programs offering undifferentiated treatment types are in fact offering individualized treatment, the results suggest that outpatient programs might be changing in the direction of a new legitimate form.
Programs that had program coordinators with a doctoral-level degree also had an increased risk of closure. Doctoral-level staff substantially increase program cost. However, they may also provide greater legitimacy for the program. The legitimacy would be more in the eyes of VA administrators than of clientele; clients in programs based on the 12-step approach typically interact with staff members who are in recovery, and coordinators with higher-level degrees are probably less likely than other coordinators to be in recovery themselves.
Modeling change within VA
The findings provided support for the legitimacy hypothesis, which holds that programs are pushed toward the legitimate form by external pressures to produce both high-quality and more streamlined treatment, as well as by uncertainty about how to achieve these outcomes. A trend was found for inpatient programs to have been influenced by these external pressures, while outpatient programs appear to have been influenced by both cost and legitimacy factors.
Change within VA is certainly occurring; however, modeling the change is more complex than looking strictly at costs, which is made clear by the fact that the staff cuts made in inpatient and outpatient programs could not be attributed to the sole aim of reducing costs.
One reason for the complexity in predicting change among programs is that the models attempted to uniformly predict decisions made by facility directors. Personal characteristics, such as their beliefs about the effectiveness of substance abuse treatment, may play a substantial role in their decisions. Likewise, political considerations, such as the quality of relationships between facility directors and program coordinators, also may be important determinants.
Another point to consider is that program changes may have been implemented to save programs from closure. Programs that were able to avoid closure may have possessed an ability to cope with organizational changes. Unfortunately, data were unavailable to test this hypothesis, because these factors and others related to administrative decision making could not be addressed in the secondary analyses of the data reported here.
To adequately model change within VA, which has a structure strongly determined by administrative decisions, more information about the guidelines under which the decisions are made is also required. The analysis of inpatient program closures hints at an answer, because program closure was related to having more than one program at a facility. This finding suggests that both cost and legitimacy concerns are at work. It also suggests that unmeasured or idiosyncratic factors at the local level, such as decisions made by facility directors, may be the most important factors.
Future directions
Further research is needed on existing programs, because the period examined here captured only the beginning of a downsizing trend. Measurement at a third time point would allow determination of whether these treatment programs adapted further. New programs could also be examined, providing a clearer application of institutional theory to this administrative structure. In addition, more information on the decision-making processes of facility directors should be gathered to help make sense of the organizational changes taking place in these treatment programs.