Almshouses, state asylums, and medical hospitals have all played roles in the institution-based care of mentally ill persons. The evolution from one type of organization to the next has been shaped by diverse factors, including political and economic changes, evolving models of intervention, shifts in responsibilities for social welfare between different levels of government, and the dominance of the private-enterprise model (
1). In recent years, the acute care psychiatric hospital industry has been challenged by managed care, government policies, and intense marketplace competition.
The California health care environment has been described as particularly turbulent. The penetration rate of health maintenance organizations (HMOs) in California is 40 to 45 percent, the highest in the country (
2). This managed care environment is characterized by regional networks, capitated reimbursement for hospitals and specialists, reduced inpatient days, reduced revenues, and consolidated services (
3). The viability of acute hospital-based psychiatric services within the context of this complex operating environment has received limited attention. Industry trend reports have difficulty capturing current industry operations in light of rapid marketplace changes, and they frequently do not reflect specific institutional characteristics that may influence facility survival or mortality.
This study was conducted to describe changes in the availability and performance of the acute psychiatric care delivery system in California between 1992 and 1996. It sought to answer three questions. What were the overall changes in availability and performance in California's acute care psychiatric facilities between 1992 and 1996? Did availability and performance differ between facilities with generalist and specialist licenses? Did availability and performance differ between facilities owned by the county, by not-for-profit organizations, and by for-profit organizations?
The study was based on a theory of organization-environment interaction. The external environment consists of resources and constraints that support or stifle specific types of organizations. Organizations continuously adapt to fit the demands of the environment; however, environmental turbulence periodically alters the boundaries and competitive structures of entire industries (
4). Distinct identifying organizational characteristics such as licensure or ownership status establish an organization's membership in the larger group of similar organizations. These characteristics directly and indirectly determine access to financial resources, define obligations to shareholders or interest groups, and create relationships with other health care providers and institutions. Accordingly, these characteristics shape economic outcomes and confer survival advantages.
Studies of licensed day care centers, apparel firms, and hospitals have demonstrated the competitive advantage offered by membership in a larger group of similar organizations (
5,
6,
7,
8,
9). Further research on the role of institutional relationships in the differential failure rates of specialist and generalist organizations has been recommended (
6). This recommendation is pertinent to the study of the acute psychiatric care delivery system. The privatization model of the past 25 years fueled the growth of the sector that includes licensed freestanding acute psychiatric hospitals as well as the sector that includes psychiatric units licensed within general hospitals. Exploring differences associated with ownership during this period of environmental turbulence in the California health care environment offered the opportunity to determine which types of organizations continued to consider care for the mentally ill population part of their mission and lines of business.
Acute care psychiatric hospitals are an outgrowth of deinstitutionalization and the expansion of public and private financing for health care and social services (
10). The general hospital sector and the acute psychiatric hospital sector grew dramatically during the mid-1980s as federal policies supported privatization and rerouted resources to the private not-for-profit and for-profit sectors. Between 1970 and 1990, the number of private psychiatric hospitals in the United States increased from about 150 to 462, and the number of nonfederal general hospitals with inpatient psychiatric services grew from 664 to 1,571 (
11). The for-profit sector grew from 88 to 350 facilities (
12). In California, the number of private psychiatric hospitals grew from 24 to 52 between 1984 and 1990, while the number of nonfederal general hospitals with psychiatric units increased from 103 to 121 (
11,
13). Thus privatization emerged as one of the most influential trends in mental health delivery in the past 20 years (
14).
Although opposition to the federal government's role in social welfare issues has existed since the New Deal, it has become significantly more influential since the 1970s. Conservative political philosophy has emphasized individual self-sufficiency, devolution of responsibility for social programs to the state and local levels, and reduced federal involvement in social welfare programs (
15). In addition, demands for control of health care costs have resulted in government policies and managed care programs that have influenced both commercial and government payment programs (
16). The health care environment has become volatile and competitive, particularly in California, and the traditional central role of the acute care hospital is diminishing (
17).
This political and financial climate has had an impact on the delivery of acute psychiatric care. By 1989 the tremendous growth of investor-owned psychiatric hospitals appeared to have come to an end; the rate of growth in 1989 was only 7 percent, compared with 41.2 percent in 1985 (
18). Since the early 1990s, the psychiatric hospital industry has experienced repeated declines in the number of facilities and beds as occupancy and lengths of stay have been reduced by tighter reimbursement practices, an oversupply of beds, expanded availability of outpatient and partial hospitalization programs, utilization review practices, and managed care penetration (
19,
20,
21,
22,
23,
24). Thus the niche occupied by acute inpatient hospital psychiatric services is in transition.
Methods
A retrospective longitudinal research design was used. This approach is useful in analyzing changes in incidence and distribution of variables in the context of the economic and political events of a period. A total population design, in which the total population is surveyed at each time point (
25), was chosen. In this study, although not every case was the same at each measurement point due to closure or opening of facilities, a majority were the same.
The base year of 1992 was selected because published data on private and general hospital psychiatric services indicated that the growth of the psychiatric hospital industry in California was in transition at about this time. At the time of the study, the most current hospital utilization data available from the Office of Statewide Health Planning and Development (OSHPD) were for 1996. In 1994 the county mental health authorities in California assumed responsibility for rate contracting and utilization review for Medi-Cal mental health funding. Thus data for the study period reflects the initial impact on hospital services of these changes.
The unit of analysis was acute care hospitals licensed to provide acute psychiatric services in California. Information on number of facilities, licensed beds, licensed bed-days, days of care, discharges, type of facility license, and ownership status is reported to OSHPD by California's nonfederal health facilities (
26,
27,
28). In this study the dependent variables were availability and performance. Availability was defined as the number of facilities and number of licensed beds. Performance was measured by the number of days of psychiatric care provided per year, the number of psychiatric discharges, the occupancy rate, and the average length of stay. The occupancy rate was calculated by dividing licensed bed-days by actual days of care. The average length of stay was calculated by dividing actual days of care by discharges.
The independent variables were licensure and ownership status. In this paper, general hospital facilities refers to psychiatric units licensed as part of a general acute care hospital. Two types of specialist psychiatric services were included in the study—licensed freestanding acute psychiatric hospitals and licensed psychiatric health facilities.
Psychiatric health facilities were established by California legislation in 1978 to provide an innovative and competitive acute psychiatric service alternative to hospital care. The legislation established program and licensure requirements for psychiatric health facilities and identified the California Department of Mental Health as having sole authority to grant requests for licensure, to approve programs, and to grant program flexibility. Psychiatric health facilities are prohibited by legislation from admitting patients with eating disorders, chemical dependency, or conditions requiring medical treatment. A majority of psychiatric health facilities are owned by local governments and are county funded. The remainder are owned and operated by private organizations. About 30 percent are either accredited by the Joint Commission on Accreditation of Healthcare Organizations or are federally certified to provide acute psychiatric services to recipients of Medicare or Short Doyle/Medi-Cal funds.
In the study reported here, ownership status was defined as not for profit, for profit, and county owned. Prisons, state mental hospitals, and chemical dependency recovery hospitals were excluded from the sample, as were general acute hospitals without licensed psychiatric beds. Data were analyzed using numerical description and comparisons based on a percent change calculation.
Results
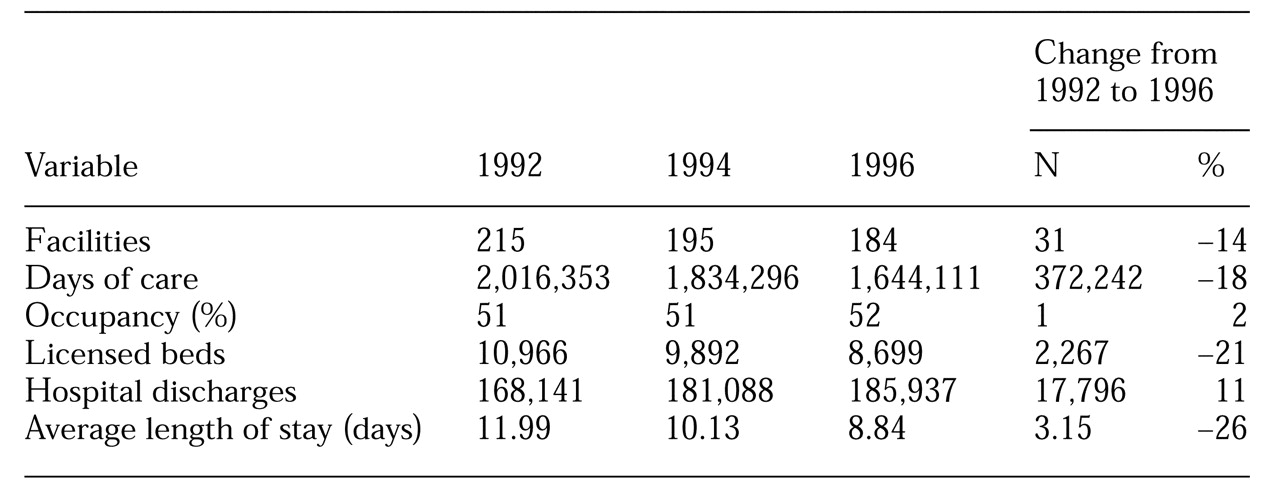
As shown in
Table 1, between 1992 and 1996 the number of acute care psychiatric facilities in California declined by 14 percent, licensed beds by 21 percent, days of care by 18 percent, and average length of stay by 26 percent. In contrast to these declines, psychiatric discharges and occupancy increased, by 11 percent and 2 percent, respectively.
The increased discharges were not evenly distributed across all regions of the state. Psychiatric discharges increased between 1992 and 1996 in eight of 14 Health Service Areas (HSAs), specifically, West Bay, East Bay, North San Joaquin, Santa Clara, Mid-Coast, Los Angeles, Inland Counties, and Orange County. Psychiatric discharges declined in the remaining six HSAs of Northern California, Golden Empire, North Bay, Central, Santa Barbara/Ventura, and San Diego/Imperial.
In 1996 approximately 70 percent of the state's population, or 24.3 million people, lived in the eight HSAs with increased discharges. Seventy-one percent of psychiatric facilities in these HSAs were general hospital facilities. A total of 9.5 million people lived in the six HSAs with decreased discharges.
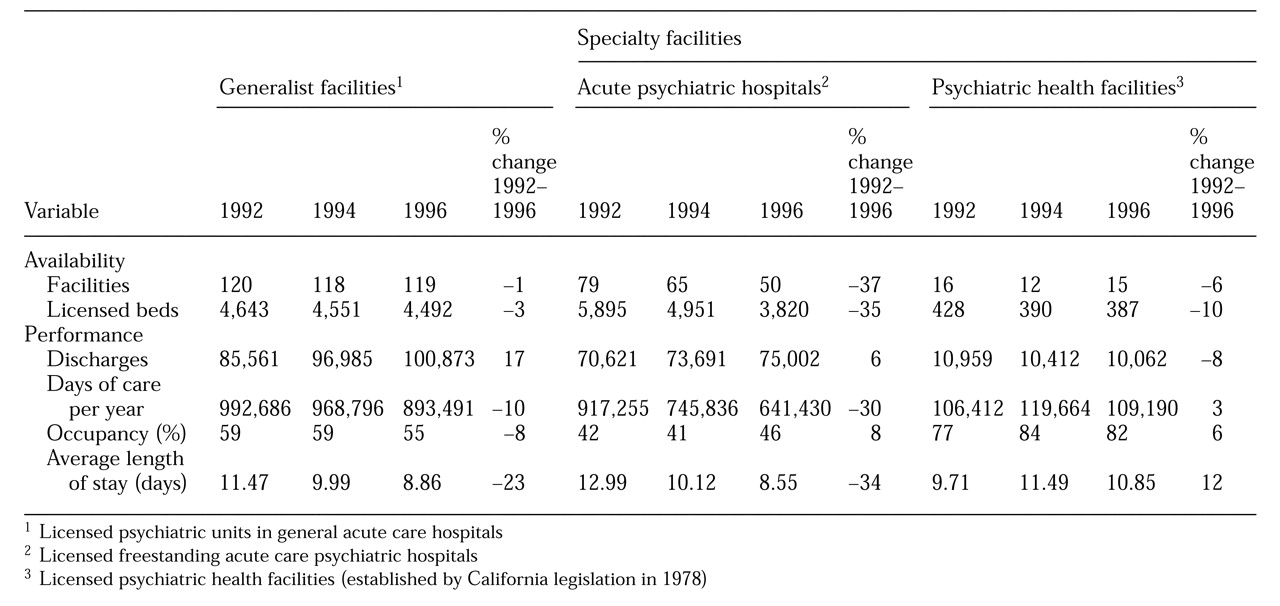
As
Table 2 shows, availability and performance differed between facilities with generalist and specialist licenses. The largest reduction in availability occurred among specialty acute psychiatric hospitals, where the number of facilities decreased by 37 percent and the number of licensed beds decreased by 35 percent. As measured by discharges, the largest increase in performance (17 percent) occurred in general hospital facilities. As measured by average length of stay, the largest increase in performance (12 percent) occurred in specialty psychiatric hospitals.
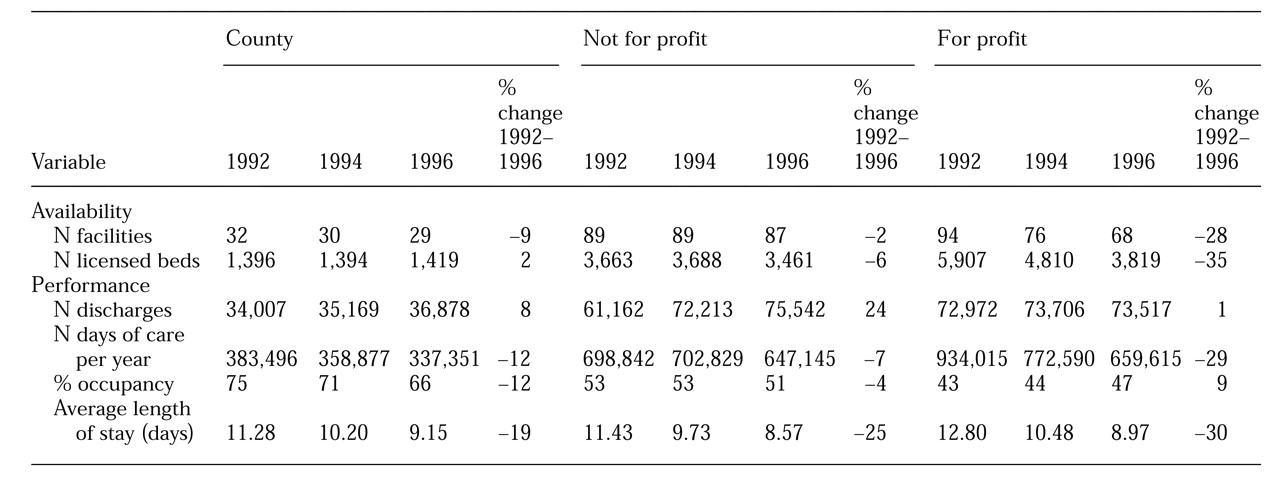
As
Table 3 shows, by ownership status, the largest decreases in availability as measured by facilities and by licensed beds were in for-profit organizations—28 percent and 35 percent, respectively. For-profit organizations also showed the largest declines in performance as measured by days of care (29 percent) and by average length of stay (30 percent). Not-for-profit organizations showed small reductions in availability as measured by facilities and by licensed beds (2 percent and 6 percent reductions, respectively). Small reductions in performance were also noted in not-for-profit organizations as measured by days of care (7 percent) and by occupancy (4 percent).
The data in
Table 3 also indicate that not-for-profit facilities showed a large decline in performance (25 percent) as measured by average length of stay and a large increase in performance (24 percent) as measured by number of discharges. County-owned facilities showed reductions in availability as measured by number of facilities (9 percent) and in performance as measured by number of days of care (12 percent), occupancy (12 percent), and average length of stay (19 percent). In county-owned facilities, slight increases were noted in the number of licensed beds and discharges (2 percent and 8 percent, respectively).
Sixty-eight percent of the specialty acute psychiatric hospitals had for-profit ownership status in 1996 compared with 78 percent in 1992. All the acute psychiatric hospitals that were closed had for-profit ownership status. In 1996 a total of 61 percent of general hospital psychiatric units had not-for-profit ownership status, 25 percent had for-profit status, and 14 percent had county-owned status. The increased discharges in the generalist network were distributed across ownership types.
Discussion
Impact is not uniform
The findings of an overall reduction in acute psychiatric hospitals and services are consistent with the downward trend in the survival of psychiatric hospitals identified in the early 1990s (
11,
20,
21,
22). However, the turbulence in the California health care environment has not had a uniform impact on all types of acute care psychiatric facilities. Although segments of the industry showed significant declines—specifically, acute care specialty psychiatric hospitals and hospitals with for-profit ownership status—psychiatric units in general hospitals, acute psychiatric health facilities, and facilities with not-for-profit ownership status and county-owned status did not experience such dramatic declines. In fact, the increased discharges from psychiatric units in general hospitals is consistent with national observations of increased discharges from general hospitals of patients with a primary diagnosis of a mental disorder (
29,
30).
The finding of a lack of uniformity in the hospital industry in response to the impact of environmental pressures is consistent with the conclusions of other observers (
31,
32,
33). Different segments of the industry are, to varying degrees, influenced by different types of pressure and are buffered from selection pressures by complex institutional environments.
The overall reduction of almost 400,000 days of care between 1992 and 1996 represents a loss of institution-based services that may or may not have been replaced by outpatient services. Hospital-based programs have traditionally not been well integrated into planned systems of community care (
34). In light of the decline in community mental health services during the 1980s as well as the early stage of development of outpatient networks by managed care companies, it is unlikely that these days of care were entirely replaced by services in a less restrictive setting. This reduction in days of care more likely represents a range of outpatient replacement, absorption of previously funded services by unpaid work of families and the community, and service elimination (
35).
It is not possible to conclude whether this decrease in capacity represents a decline in quality of care. It does reflect a shift in resources and a change in service delivery patterns, with concomitant ramifications for the performance of the psychiatric services industry.
Survival advantages
Reimbursement advantages.
One advantage enjoyed by psychiatric units in general hospitals is that federal law allows Medicaid reimbursement for adult patients between the ages of 21 and 64. This law has fueled the growth of general hospital psychiatric programs since passage of Medicaid in the mid-1960s.
Although managed care for psychiatric inpatients covered by the Medi-Cal program was implemented in 1994, the impact on psychiatric admissions has not been uniform statewide. Between fiscal years 1994 and 1996, Medi-Cal admissions declined in four regions—Bay Area, Central, Southern California, and Superior. However, admissions for the Los Angeles region continued to climb (California Department of Mental Health, unpublished data, 1997).
Provision of psychiatric services in units of general hospitals has had another reimbursement advantage over provision in other acute psychiatric facilities. Although psychiatric services provided in both units of general hospitals and acute specialty psychiatric hospitals are usually reimbursed by Medicare based on a "reasonable cost" methodology, per-discharge interim payments for services provided in general hospital units have been noted to be higher than interim payments to acute specialty psychiatric hospitals (
36). In 1995, 74.2 percent of Medicare-funded psychiatric discharges were from general hospitals (
36). During this same time period, only about one-third of Medicare beneficiaries in California were enrolled in HMOs (
37). The volume of Medicare-funded discharges for psychiatric services provided in general hospitals, the reimbursement methodology, and the lack of managed care controls suggest that this payment source was advantageous to general hospitals.
Referral channels.
A second advantage of providing services in general hospital psychiatric units is the links to referral channels offered by these hospitals and their accessibility to referring physicians from other specialties and their patients. California managed care is distinguished by the central role played by organized physician groups, which have frequently negotiated with HMOs to receive both capitated payments for physician services and dollars targeted for hospital and ancillary services (
37). General hospitals are included in these multispecialty delivery systems and contractual networks, giving them a distinct advantage over specialty psychiatric hospitals.
Behavioral health benefits are increasingly carved out of general health insurance policies, and contractual networks are separately negotiated. However, psychiatric units in general hospitals may still have better access to the contracting infrastructure and psychiatric provider network to facilitate negotiated relationships with carve-out companies.
Geographic dominance.
A third advantage for general hospital psychiatric units is their dominance in the eight HSAs with increased discharges, where 70 percent of the state's population reside. Such units constituted 71 percent of the psychiatric facilities in these HSAs. The provision of inpatient psychiatric care has been shown to be extremely sensitive to the supply of both providers and inpatient psychiatric treatment units (
38).
Unique nature of psychiatric health facilities
The specialty psychiatric health facilities were more successful as measured by increases in days of care, occupancy, and average length of stay. These facilities are primarily county owned, and funding is primarily from public sources. The facilities are frequently located in areas with limited competition. Their performance is potentially susceptible to the owner-payer's management goals. For example, when the owner and payer is the same entity, such as the county, the desirability of maintaining a stable occupancy to meet budget targets, ensuring maximum federal match for local dollars when matching is an option, and maintaining a stable labor pool may influence management decisions. Many psychiatric health facilities are located in rural areas, which may have fewer community-based resources to provide nonacute care and limited incentives to develop alternatives to acute care because the alternatives might undermine the stability of the acute care resource. Also, because of travel difficulties in nonmetropolitan areas, staff may be less willing to discharge a patient who may require aftercare assistance (
39).
Ownership status
General hospital psychiatric units constituted more than 80 percent of the facilities with not-for-profit ownership status in 1992 and 1996. Therefore, some of the generalist facilities' advantages also applied to not-for-profit ownership status. As discussed above, these advantages were related to serving the Medi-Cal population, Medicare reimbursement methods, geographic location, and referral channels.
The reduction in availability of acute psychiatric services was most apparent among specialty acute care psychiatric hospitals and for-profit facilities. The substantial declines in facilities and beds in these facilities are best explained by the overriding goal of maximizing revenue in the for-profit sector. This sector has focused almost exclusively on inpatient services and has relied primarily on client fees and private insurance from better-insured client groups (
40). As managed care and the competitive market environment have made inpatient psychiatric care unprofitable, these programs are being closed.
The finding of a reduction in services provides evidence to support concerns that for-profit systems may abandon privatized services in the face of unacceptable profitability (
41). These concerns become more critical as not-for-profit and county-owned general hospitals undergo ownership conversions to for-profit status. The fact that the number of specialty acute psychiatric facilities under not-for-profit ownership remained unchanged between 1992 and 1996 does not automatically mean that the services provided in this ownership category were more financially successful. It may simply be an example of the greater reluctance of not-for-profit facilities to reduce excess capacity or to eliminate unprofitable services (
42,
43). Not-for-profit systems are expected to serve community needs in order to justify their tax-exempt status. Service to the indigent population was also an explicit requirement of the 1946 Hill-Burton construction legislation (
12). Thus not-for-profit psychiatric facilities have traditionally served a broad mix of patients, including those with poor reimbursement coverage (
40).
Challenges
The Balanced Budget Act of 1997.
Most psychiatric hospitals and psychiatric units of general medical hospitals have been exempt from Medicare's inpatient prospective payment system since its implementation in 1983. These psychiatric services have been reimbursed under provisions of the 1982 Tax Equity and Fiscal Responsibility Act (TEFRA). The TEFRA payment system reimbursed hospitals according to a formula that considers each hospital's specific operating costs up to a limit for each discharge. The TEFRA payment system also reimbursed capital costs on a reasonable basis, paid bonus payments when reimbursable costs were below the target amount per discharge, and reimbursed bad debt on a dollar-for-dollar payment schedule (
44).
The Balanced Budget Act of 1997 provided for $150 billion in Medicare savings and $8.4 billion in net Medicaid reductions in the five-year period between 1998 and 2002. Under the act, 63 percent of the Medicare spending reductions in fiscal year 1998 were to come from reduced payments to hospitals (
45).
The new Medicare rules also include major changes in the cost-based reimbursement policies that applied to many psychiatric hospitals and units under TEFRA, including a freeze in the fiscal year 1998 update factor (an inflationary increase of the TEFRA limit), reduction in bonus payments, a 15 percent reduction in capital payments, and bad-debt payment reductions of 25 percent in fiscal year 1998, 40 percent in 1999, and 45 percent in 2000 and thereafter. The rules establish an overall payment limit, or national cap, for programs exempt from the prospective payment system (
44).
Eighty-four percent of psychiatric facilities will experience payment reductions as a result of these reductions in Medicare reimbursement (
46), which will save about $7 billion over the five-year period (
44). The Medicaid savings are largely aimed at reduction in payments to disproportionate-share hospitals, facilities that provide a disproportionate volume of services to the Medicaid population. It is anticipated that these cuts will result in hospital closures and further reductions in bed capacity (
47).
Alternative providers.
Alternative providers to licensed inpatient psychiatric services also present significant challenges. Advances in psychopharmacology and the ability of primary care providers to diagnose and treat psychiatric symptoms divert to other settings patients who might have previously received inpatient psychiatric care. Psychiatric patients may be hospitalized in general hospital units not licensed for psychiatric services (
48).
Subacute psychiatric care organizations have made inroads into the traditional inpatient psychiatric hospital market share. Subacute levels of care, as well as crisis residential facilities, represent a less costly alternative to acute hospital services for patients requiring continued institutional care. Such alternatives reduce lengths of stay in acute care facilities or replace acute services altogether. The remaining niche for psychiatric units in general hospitals is likely to involve difficult-to-treat patients, including those with substance abuse or those with complex psychiatric and medical comorbidities (
49).
Conclusions
The recent declines in the for-profit, acute care psychiatric hospital specialty sector demonstrate that over the short term, reductions in services are related to organizational characteristics. However, changes in federal Medicare reimbursement policy to psychiatric services exempt from the prospective payment system are likely to result in further closures of all types of psychiatric acute care facilities. This eventuality represents a reversal of the 1980s policy of supporting privatization through the redirection of public funds to the for-profit sector. Instead, current policy demonstrates the redirection of public funds away from institution-based services and the diminution of the federal government's involvement in social welfare issues.
The closures between 1992 and 1996 in the for-profit specialty hospital sector represent early exiting by organizations highly susceptible to declines in profitability. Closing of facilities in the for-profit sector supports concerns that this form of ownership may not sustain long-term commitment to individuals and communities that rely on less profitable services. This concern becomes more critical as private not-for-profit and county-owned general hospitals convert ownership to for-profit status.
However, it should not be assumed that closures of psychiatric services would be avoided if such changes in ownership did not occur. Not-for-profit and county-owned systems will still grapple with the dilemma of sustaining access not only to psychiatric services but also to other unprofitable medical services as funding streams are reduced in the next few years. The for-profit specialty sector has simply taken more rapid steps to stem financial losses.
The striking increase in the number of patients discharged from acute psychiatric units in general hospitals, regardless of ownership status, should not be automatically interpreted as an indicator of business acumen in this sector or that these facilities have long-term, sustainable advantages. This success likely reflects the short-term buffering that results from greater opportunity to participate in publicly funded programs, linkages to nonpsychiatric health care providers and resources, and geographic location. Buffering does not necessarily offer a permanent advantage; it simply eases the requirement for rapid reorganization.
In fact, the trend of increasing discharges in the generalist sector requires examination of repeat admissions to evaluate whether shorter hospital stays are associated with recidivism. With average lengths of stay driven down to about eight and a half days, acute inpatient psychiatric care has become focused on crisis stabilization. Provision of supportive care has shifted to alternative settings.
The trend toward an increasing number of discharges should also be examined for payer mix to determine whether it represents disproportionate hospital utilization by a population such as Medicare patients who have not yet fully experienced the limitations of managed care. Programs that have attempted to improve their financial position by expanding services to Medicare patients are likely to find that this solution is transitory.
Challenges to institution-based services for the mentally ill population now extend beyond the state hospital system to include community-based acute psychiatric hospital services. Recent declines in the for-profit, acute care psychiatric hospital specialty sector as well as the success of the generalist and not-for-profit sectors demonstrate the lack of uniform responses to environmental pressures by organizations with different licensure and ownership characteristics. However, changes in federal Medicare reimbursement policy established by the Balanced Budget Act of 1997 as well as competition from alternative providers are likely to result in further closures of all types of facilities over the next few years.
Acknowledgments
The author acknowledges the contributions of Wingham Liddell, Ph.D., Andrew Merrifield, Ph.D., and Noel Byrne, Ph.D., to this study.