Poor prenatal care is an established risk to the health of the infant and mother. Women who receive inadequate prenatal care are at risk for poor pregnancy outcomes (
1) and decreased use of pediatric care after birth, including missed immunizations and well-child visits (
2,
3). Therefore, increasing first-trimester prenatal care to at least 90 percent of live births has become a national health priority (
4). To determine the adequacy of prenatal care, both the timing of initiation of care and the total number of prenatal visits must be assessed.
Over the past two decades, epidemiologic investigations have identified a number of external barriers to prenatal care, including increased parity (having borne at least one child previously), African-American race, younger age, single marital status, and lower educational attainment (
1,
5,
6,
7). Financial barriers have also been identified as an important deterrent to adequate prenatal care (
5,
7). Programs to increase financial access have not eliminated the problem (
8). Other factors that may explain the persistence of inadequate levels of prenatal care among at-risk populations are being explored.
Investigators have begun to document internal barriers—psychological and emotional factors that inhibit pregnant women from gaining access to adequate care (
6,
9,
10). Joyce and associates (
10) asked their sample of 70 women to retrospectively report the primary reason they did not obtain prenatal care; more women reported depression, denial, and fear (47 percent) than financial or transportation problems (23 percent). Melnikow and Alemagno (
9) documented that shame and fear of the physician or pregnancy were associated with increased risk of inadequate prenatal care; these associations remained significant even when the analysis adjusted for demographic characteristics. In addition, an unwanted pregnancy is a strong predictor of inadequate prenatal care (
6). Although these studies assessed maternal psychosocial stress and mood states, they did not explicitly examine psychiatric symptoms.
Our review revealed no population-based studies examining the impact of maternal psychiatric disturbance on the level of prenatal care. Clinical investigations have documented that pregnant women with chronic schizophrenia have less adequate prenatal care than women without this disorder (
11,
12) and that pregnant psychiatric inpatients appear to have poor prenatal care before and after psychiatric hospitalization (
13,
14). However, these reports have a number of limitations. They were limited to women with severe psychiatric disturbance and did not adjust for other risk factors known to be associated with poor prenatal care. Furthermore, the small sample sizes and specialty mental health settings limited generalizability to the population of pregnant women with psychiatric disturbance cared for in the general obstetrical sector.
In contrast, it has been well established that maternal substance abuse has a negative impact on the utilization of prenatal care (
15). However, few studies have assessed the various dimensions of prenatal care in this population to determine if substance-abusing pregnant women are at higher risk for late initiation of care or decreased total number of visits.
The advent of linked databases allows for population-based approaches to the study of psychiatric disorders among pregnant women. To better understand the relationship between psychiatric and substance use disturbance and level of prenatal care, we undertook a cross-sectional analysis of data from the California Health Information for Policy Project (CHIPP) database. Our primary research questions were, Are women who have psychiatric and substance use diagnoses recorded in their obstetrical medical charts at increased risk for inadequate prenatal care? Do these increased risks persist when the analysis controls for demographic and financial barriers to care? We were also interested in determining whether women with psychiatric and substance use diagnoses were at risk for late initiation of prenatal care, decreased total number of prenatal visits, or both.
Methods
The CHIPP data set links vital statistics birth and infant-death records from the California Department of Health Services with maternal and infant hospital discharge records of the Office of Statewide Health Planning and Development. A detailed description of the data set and linkages is provided elsewhere (
16). In 1994 and 1995 a total of 1,094,178 maternal discharge records existed for women with single births who delivered in California civilian hospitals. Prenatal care information was missing for 5.3 percent (N=57,613) of the women. Demographic data were missing for 3.8 percent; a large proportion (58 percent) of women with missing prenatal care data also had missing demographic data.
Psychiatric and substance use diagnoses
The CHIPP database contains information on all International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnoses recorded on the obstetrical discharge summary, which allows for a maximum of 25 diagnostic codes. We examined the frequencies of psychiatric disorders using five broad diagnostic categories: substance-related disorders, schizophrenic disorders, mood disorders, anxiety disorders, and other psychiatric disorders.
Two obstetrical ICD-9-CM diagnostic categories were also examined because they can be used in lieu of more specific ICD-9-CM psychiatric diagnoses: mental disorder of pregnancy (ICD-9-CM 648.4) and substance use disorder of pregnancy (ICD-9-CM 648.3). Disorders of childhood, dementia, and other cognitive disorders were excluded because they occur at the extremes of the life span and are of less relevance for women of childbearing age. Diagnoses that may be secondary to medical complications of delivery, such as delirium and diagnoses "due to a general medical condition," were excluded because they are likely to be transitory and confounded by the medical condition.
Given that our primary aim was to understand the unique associations between psychiatric and substance use disturbances and inadequate prenatal care, we did not include women with dual diagnoses as a separate group for investigation.
Prenatal care
The level of prenatal care was assessed from data in the birth record file using the Kotelchuck Adequacy of Prenatal Care Utilization Index (
17). This index provides a rating of overall prenatal care utilization—inadequate, intermediate, adequate, and adequate plus. The ratings are based on two dimensions: the adequacy of initiation of prenatal care, which is determined by the month prenatal care begins, and the adequacy of received services, which compares the total number of prenatal visits adjusted for length of gestation with the expected number of visits based on standards set by American College of Obstetricians and Gynecologists.
Inadequate overall prenatal care utilization is defined as either inadequate or intermediate initiation—after the fourth month of pregnancy—or inadequate received services, less than 50 percent of recommended visits. For further analyses, we categorized prenatal care utilization as a bivariate outcome as has been done in previous reports (
8): inadequate prenatal care versus any other category of prenatal care.
Demographic and maternal characteristics
The demographic and maternal characteristics we examined were extracted from the birth record file. Race was classified as white non-Hispanic, Hispanic, African American, Asian American, Native American, and other. Age was examined as a continuous variable. Education and marital status were dichotomized. Payment source was described using four categories derived from previous population-based investigations (
18): private insurance; Medi-Cal, which is California's Medicaid program, and other government programs; health maintenance organization (HMOs) or preferred-provider organization (PPOs); and self-pay or no insurance. Parity was categorized as no previous deliveries (primiparous), one to three previous deliveries, and four or more previous deliveries.
Prenatal care data were missing for approximately 5 percent of the women (N=57,613). Compared with women whose prenatal care data were recorded, a higher proportion of the women with missing data were Hispanic, single, and insured by Medi-Cal. They were also more likely to have had previous deliveries and to have lower educational levels, and a larger proportion had psychiatric diagnoses (2.7 percent versus 1.4 percent) and substance use diagnoses (2.6 percent versus 1.6 percent). Bivariate analyses including women with missing care data in the inadequate-care category did not substantially alter the association between inadequate overall prenatal care utilization and psychiatric diagnoses (odds ratio=3.07, 95 percent confidence interval=2.98 to 3.17) or substance use diagnoses (OR=3.29, CI=3.19 to 3.39). Therefore, we excluded women with missing prenatal care data from all further analyses.
Statistical analyses
We first ascertained the percentage of women for whom psychiatric and substance use diagnoses were recorded in the obstetrical medical chart. We next examined the bivariate associations between diagnoses and maternal characteristics and level of prenatal care. We calculated unadjusted odds ratios and 95 percent confidence intervals for psychiatric and substance use diagnoses and inadequate overall prenatal care utilization, as well as for the two subcomponents of the Kotelchuck prenatal care index: inadequate initiation of care and inadequate received services.
Three separate logistic regression models were constructed to ascertain the unique associations between psychiatric and substance use diagnoses and inadequate overall prenatal care utilization, between psychiatric and substance use diagnoses and inadequate initiation of care, and between psychiatric and substance use diagnoses and inadequate received services while adjusting for race, payment source, age, marital status, education, parity, and diagnostic group. The final multivariate logistic models included women for whom prenatal care and demographic data were available (N=1,027,871). All variables were entered into each logistic model simultaneously. Adjusted odds ratios and 95 percent confidence intervals were calculated by diagnostic group and demographic characteristic for the three components of prenatal care.
Results
Characteristics of the population
The mean±SD age of women delivering in California in 1994 and 1995 was 27±6.2 years, and 40 percent of the mothers were primiparous. More than half of the women were ethnic minorities, with Hispanics constituting 48 percent of the population, African Americans 7 percent, Asian Americans 7 percent, Native American less than 1 percent, and Caucasians 34 percent. Sixty-seven percent of women were married, and 66 percent had at least a high school education.
Nineteen percent of the women were covered by private insurance, 28 percent by HMOs or PPOs, and 50 percent by Medi-Cal; 3 percent had no insurance. As
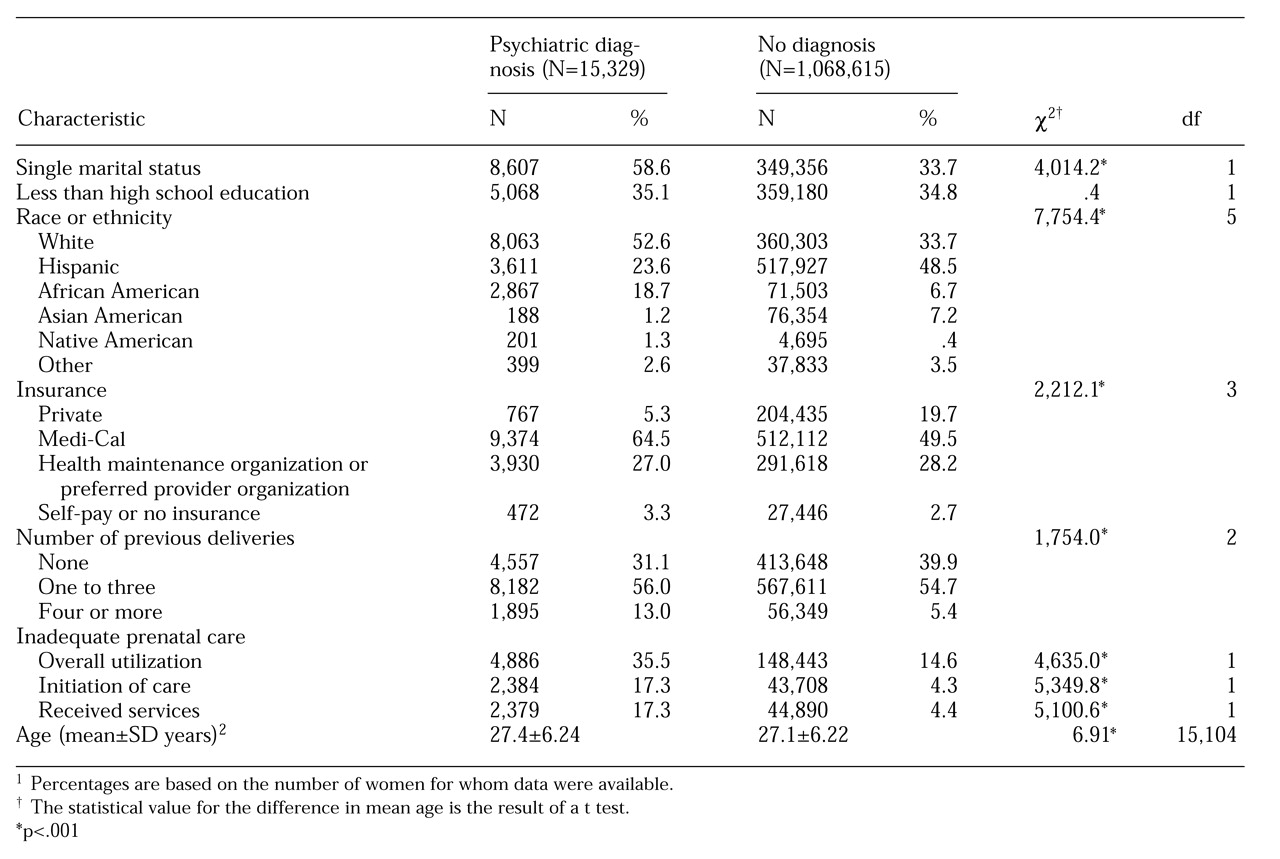
Table 1 shows, 15,329 women received psychiatric diagnoses, which constituted 1.4 percent of the population delivering babies during 1994 and 1995. Compared with women who received no psychiatric or substance use diagnoses, women with psychiatric diagnoses were significantly more likely to be single, African American, or white; to be covered by Medi-Cal or uninsured; and to have had a least one previous delivery.
As
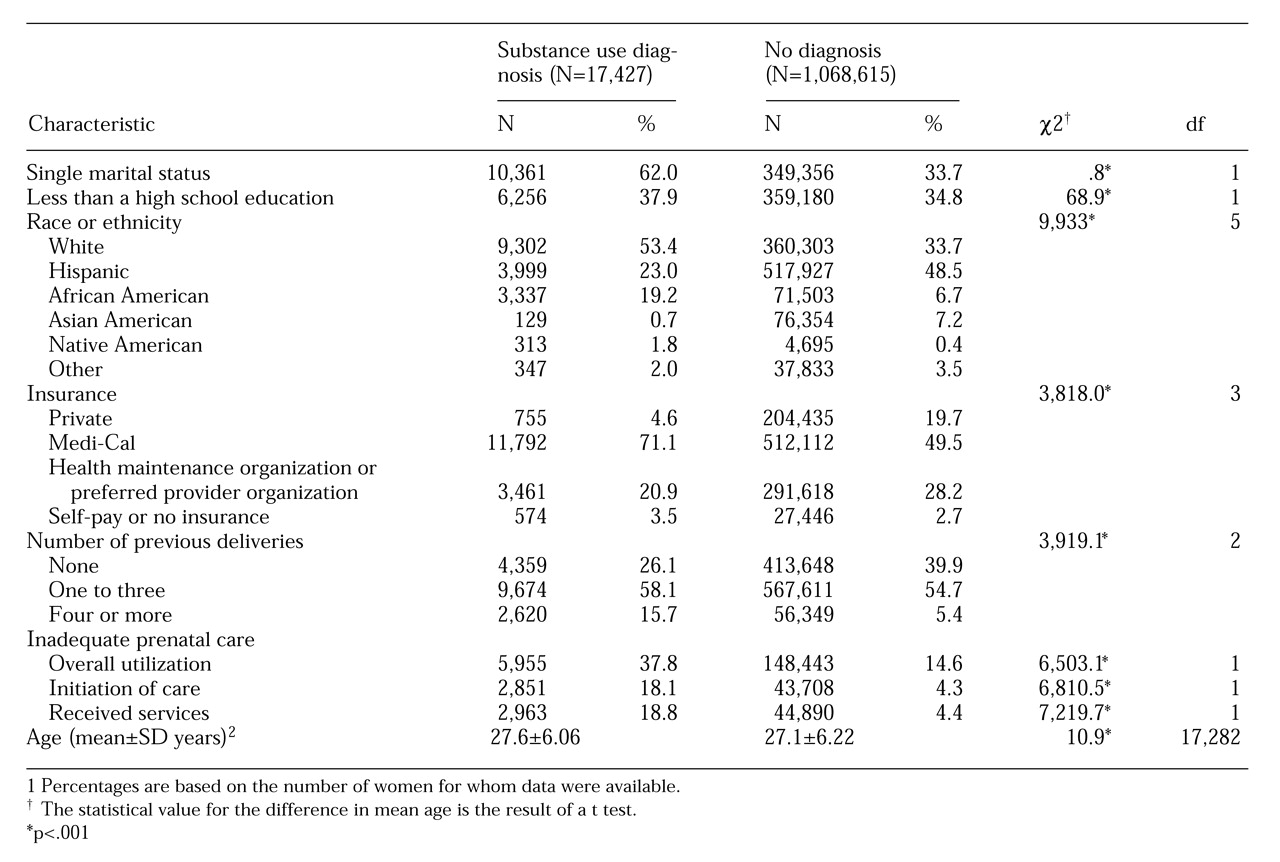
Table 2 shows, 17,427 women received substance use diagnoses, which constituted 1.6 percent of the women delivering in 1994 and 1995. The demographic and prenatal care characteristics of these women were similar to those of the women with psychiatric diagnoses, although the women who received substance use diagnoses were significantly more likely to have lower educational attainment than the women who received no psychiatric or substance use diagnoses.
Prenatal care utilization
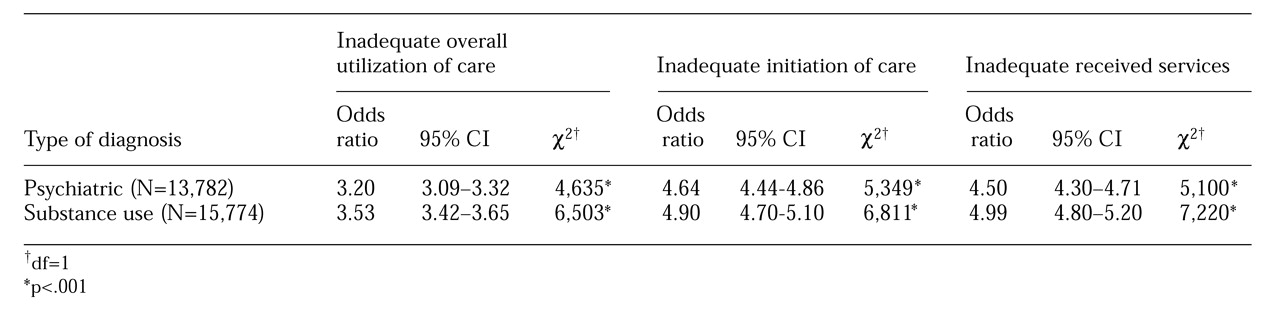
Fifteen percent of women delivering in 1994 and 1995 had inadequate overall utilization of prenatal care. As shown by the odds ratios in
Table 3, women with psychiatric diagnoses had more than three times the risk of inadequate overall utilization of prenatal care and approximately four and a half times the risk of inadequate initiation of prenatal care and inadequate received services than women who did not have a psychiatric or substance use diagnosis. For women with substance use diagnoses, the risk of inadequate overall utilization of prenatal care was three and a half times higher than for women with no diagnoses, and the risk of inadequate initiation of care and inadequate received services was nearly five times higher.
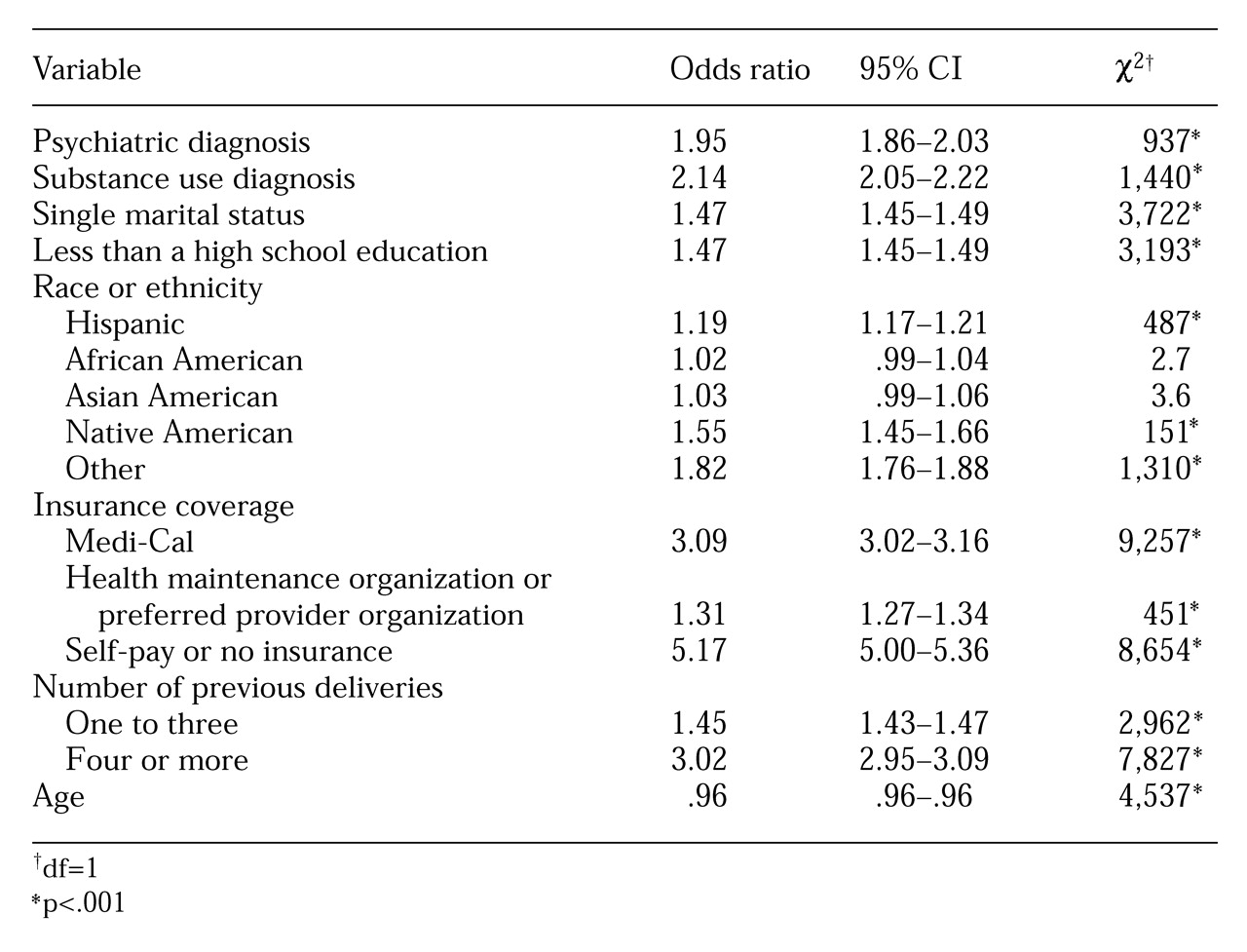
As
Table 4 shows, in multivariate models that adjusted for demographic variables, women with psychiatric or substance use diagnoses continued to have an increased risk of inadequate overall prenatal care. Furthermore, in the logistic regression models, the risk of inadequate overall prenatal care was similar for women with psychiatric and substance use diagnoses. Consistent with previous reports, predictors of poor prenatal care were not having private insurance, single marital status, lower educational attainment, having at least one previous delivery, younger age, and Hispanic and Native American race.
When the subcomponents of the Kotelchuck index were examined in multivariate models and the analyses adjusted for demographic variables, women with psychiatric diagnoses continued to have an increased risk of inadequate initiation of prenatal care (OR=2.36, CI=2.23 to 2.50; χ2=910, df=1, p<.001) and inadequate received services (OR=2.18, CI=2.06 to 2.31; χ2=751, df=1, p<.001). In these logistic models, women with substance use diagnoses also continued to have an increased risk of inadequate initiation of care (OR=2.42, CI=2.30 to 2.55; χ2=1,135, df=1, p<.001) and inadequate received services (OR=2.60, CI=2.46 to 2.73; χ2=1,361, df=1, p<.001).
Discussion and conclusions
This study is the first population-based investigation to examine the association between psychiatric diagnoses and inadequacy of prenatal care. Our findings document that among all women delivering babies in California in 1994 and 1995, women with chart-recorded psychiatric diagnoses at the time of delivery were about twice as likely as women without psychiatric or substance use diagnoses to receive inadequate prenatal care. In addition, our results confirm that women with substance use diagnoses were also at risk for poor prenatal care, and that the increased risk was similar in magnitude to that for women with psychiatric diagnoses.
We found that women with psychiatric diagnoses and those with substance use diagnoses were at increased risk for both late initiation of care and fewer prenatal care visits.
A strength of this study is that having data on the entire population allowed us to control for potentially confounding maternal demographic factors known to affect the level of prenatal care. Our findings confirm previously established demographic risk factors for poor prenatal care, including being from a nonwhite ethnic group, single marital status, lower educational attainment, not having private insurance, younger age, and having at least one previous delivery.
Many possible explanations can be offered for our findings. It has been documented that situational and psychosocial risk factors, including lack of social support (
19), are associated with poor prenatal care. These psychosocial risk factors may precipitate psychiatric symptoms or disturbance in vulnerable women. In addition, a relationship may exist between maternal psychiatric disturbance and unwanted pregnancy or deliberations about the termination of pregnancy, both of which have been associated with poorer prenatal care (
6,
20).
It has also been shown that women who are less aware of the signs and symptoms of pregnancy or who deny a pregnancy delay seeking care (
6,
21); these women may also be at risk for psychiatric disorders. Last, some psychiatric disturbances may affect motivation for care or belief in the benefit of care, both of which have been shown to affect care seeking (
22).
The similar demographic profiles and increased risks for inadequate prenatal care among women with psychiatric and substance use diagnoses are a source of concern. Previous research has established that inadequate prenatal care for substance-using pregnant women has serious consequences, including poorer pregnancy outcomes (
23,
24) and increased hospital cost and length of hospital stay for their neonates (
25). Whether or not poor prenatal care among psychiatrically disturbed women is associated with these poor outcomes remains to be seen.
Several important considerations arise in the interpretation of our findings. Because the CHIPP data is cross-sectional, it does not allow for an examination of the course of mental disturbance or of obstetrical decision-making patterns. We assume that recorded psychiatric diagnoses at the time of delivery are indicative of ongoing mental disturbance during pregnancy. It is possible that some of the psychiatric disorders recorded at delivery developed during later stages of pregnancy or at the time of delivery and therefore would have had less impact on the use of prenatal care. However, if this were the case, our reported estimates of the association between diagnoses during pregnancy and poor prenatal care may be conservative. An additional potential bias is the possibility that obstetricians are more likely to diagnose psychiatric disturbance at delivery among women with inadequate prenatal care.
An additional limitation of this study is that psychiatric disorders appear to be underreported on hospital discharge summaries (
26). Previous epidemiologic reports have documented much higher prevalence rates of mental disorders during pregnancy than the prevalence rates reflected in the chart-recorded diagnoses we documented. This discrepancy suggests that a substantial number of women with disorders were included in the group of women with no diagnosis, which again may mean that the association between diagnoses and inadequate care is stronger than our findings suggest.
Finally, the CHIPP data set does not allow for an assessment of the validity of the chart-recorded psychiatric and substance use diagnoses. It has also been suggested that the accuracy of information obtained from birth certificates may not be optimal (
17,
24). However, the demographic predictors of poor prenatal care we demonstrated reflect those found in previous epidemiologic reports, suggesting that the data adequately represent the population.
Further clinical research is needed to elucidate the processes of prenatal care for women with psychiatric and substance use diagnoses. In addition, future investigations will need to assess the risk of poor perinatal outcomes among psychiatrically disturbed women who receive poor prenatal care and will need to examine the benefits of providing interventions to this population. Research on drug- and alcohol-abusing pregnant women has shown that providing prenatal care can reduce the incidence of premature birth, low birth weight, small head circumference, and other perinatal complications (
24,
27).
In summary, this study suggests that in addition to maternal substance abuse, maternal psychiatric disturbance should be included in the complex theoretical framework of predictors of poor prenatal care. Recent epidemiologic reports suggest that psychiatric disorders are as prevalent among pregnant women as in the general population of women, which indicates that they would affect a significant proportion of women requiring prenatal care (
28,
29,
30). Because successful interventions to increase the adequacy of prenatal care have been difficult to design (
31), identifying and treating women with psychiatric diagnoses may improve levels of prenatal care as well as the use of pediatric health care services after delivery. Our findings, if corroborated, suggest that strategies to improve both early initiation of care and continuity of care among psychiatrically disturbed women are needed.
Acknowledgments
This research was conducted with the support of National Research Service Award grant 1-F32-MH-11892-01 from the National Institute of Mental Health to Dr. Kelly and additional support from the University of California, Davis. The California Health Information for Policy Project data set is supported by a grant from the Robert Wood Johnson Foundation.