VA manages the largest integrated health care system in the United States, providing care at approximately 950 treatment facilities of various types located across the United States. Many of the more than 150 hospitals in the system are large metropolitan medical centers that are closely affiliated with medical schools, but the system also includes a spectrum of smaller general medical centers, psychiatric facilities, more than 400 outpatient clinics, 133 nursing homes, and more than 200 counseling centers. Thus the VA system broadly reflects health care delivery settings in the United States, although its patient population is significantly older, predominantly male, and more likely to have multiple comorbid diagnoses, especially including mental disorders, than the general patient population (
9,
10).
This study provided information on assault in VA facilities during a full fiscal year. Data include numbers, types, and locations of assaults; assault-related injuries to staff and time lost resulting from these injuries; and information on perpetrators of assaults. The survey also sought information about administrative and educational activities to prevent and manage assault.
Methods
The survey
A survey was distributed to all VA medical centers and freestanding clinics, asking for cumulative data for fiscal year October 1, 1990, through September 30, 1991. Several data elements were requested. First, facilities were asked the number of incidents and types of assaultive behavior during the period. The survey instructions provided facilities with examples for each of the categories. If an incident contained elements of more than one category, it was classified in the category that best reflected the severity of the incident. The survey asked for information on the locations in the health care facility where the behavior occurred. Facilities reported the number and types of injuries sustained by the patients involved (perpetrators or victims), staff, visitors, and others. They also reported the amount of staff time lost due to injuries sustained as the result of assault.
In addition, the survey requested information about the most common diagnoses of perpetrators of assaults, the number of staff trained in the management of assaultive behavior, the types of recommendations generated from formal reviews of the incidents, and the procedures in place for managing assaultive behavior at the facility.
Surveys were mailed to the director of each facility, which included 160 medical centers and eight freestanding multispecialty clinics. Completion of the survey was most often coordinated by the person in charge of the facility's quality management program (65 percent) or the chief of psychiatry or psychology (16 percent). Data sources used to complete the survey included mandatory reports on any incident adversely affecting a patient or visitor, police reports, worker's compensation and Occupational Health and Safety Administration reports, quality management and risk management reports, and staff training reports. A total of 159 medical centers and seven freestanding multispecialty clinics responded to the survey.
Additional data sources
Centralized VA data sources were also used in the study. They included staffing reports of the number of employees on duty on the last day of the study year. Data on the total number of patients treated on inpatient psychiatry units and the average length of stay during the study year at each facility were obtained from data files on discharges, deaths, and the end-of-year inpatient census. Information about per diem costs for direct clinical care on inpatient psychiatric units was obtained from the VA cost distribution report, which includes such costs for all facilities.
Results
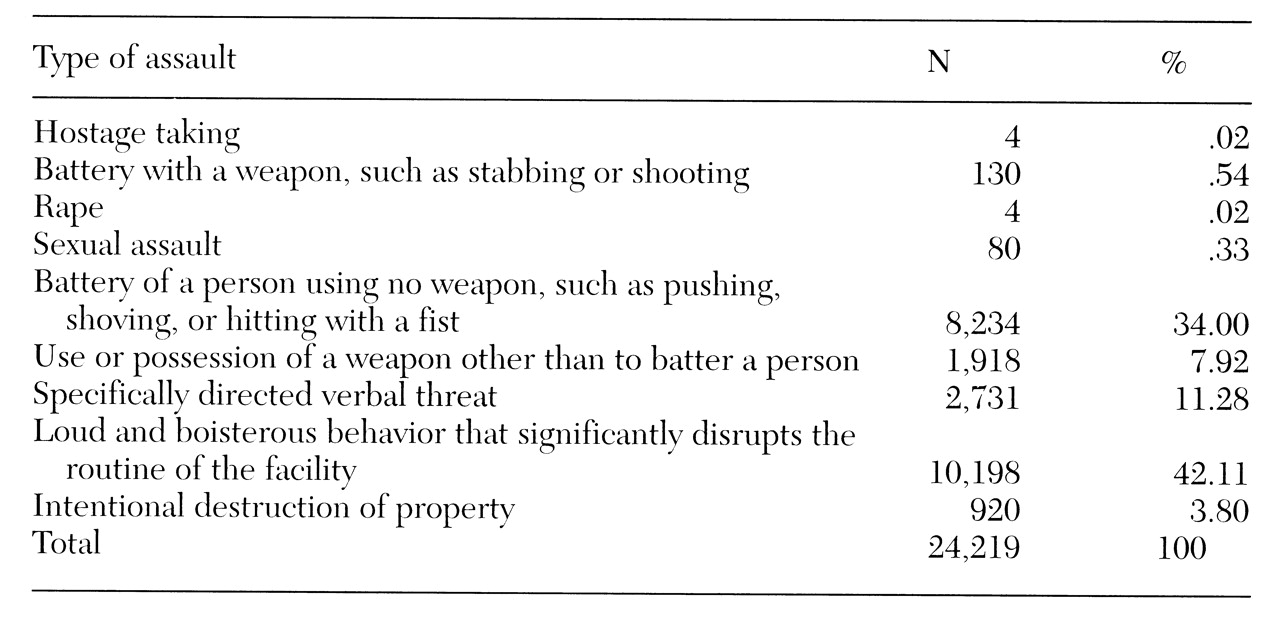
Table 1 presents the total number of incidents of assaultive behavior reported by all facilities according to the type of assaultive behavior and arranged by the severity of the behavior. During the one-year period, 24,219 incidents of assaultive behavior were reported by the 166 VA treatment facilities. Battery of a person or physical assault occurred 8,552 times. Weapon possession by perpetrators was common (8.5 percent of incidents), and weapons were used in 130 assaults (1.5 percent of assaults).
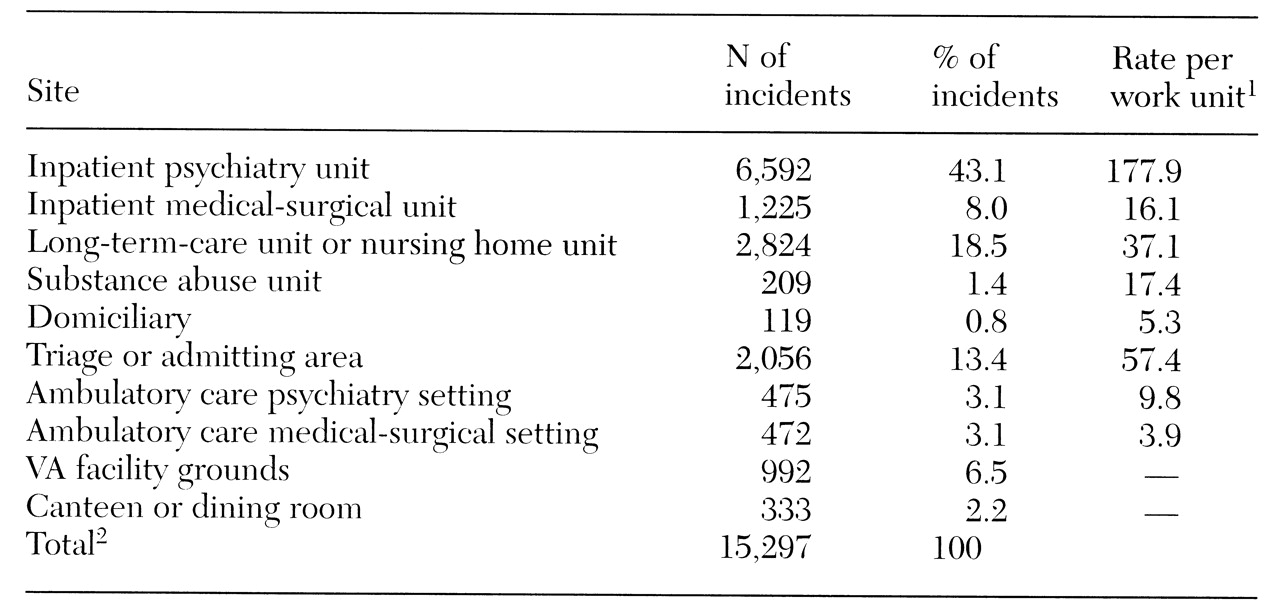
Table 2 presents locations within the facility where assaultive behavior occurred. Only 156 facilities reported locations, and they did not record the location for every event. Thus the total number of incidents is less than the total in
Table 1. The most frequent clinical sites for assaultive behavior were psychiatric wards (43.1 percent of incidents), long-term-care units (18.5 percent), and admitting or triage sites (13.4 percent). A substantial number of incidents (8 percent) occurred on inpatient medical and surgical units and in medical and surgical outpatient clinics (3.1 percent).
In addition to the total number of incidents, the rates of incidents per work unit were calculated. The rates for inpatient work units were based on 100,000 days of care provided during the year in the particular work unit at facilities reporting incidents for that unit. The rates for outpatient work units were based on 100,000 visits to the particular unit during the year for facilities reporting incidents for that work unit.
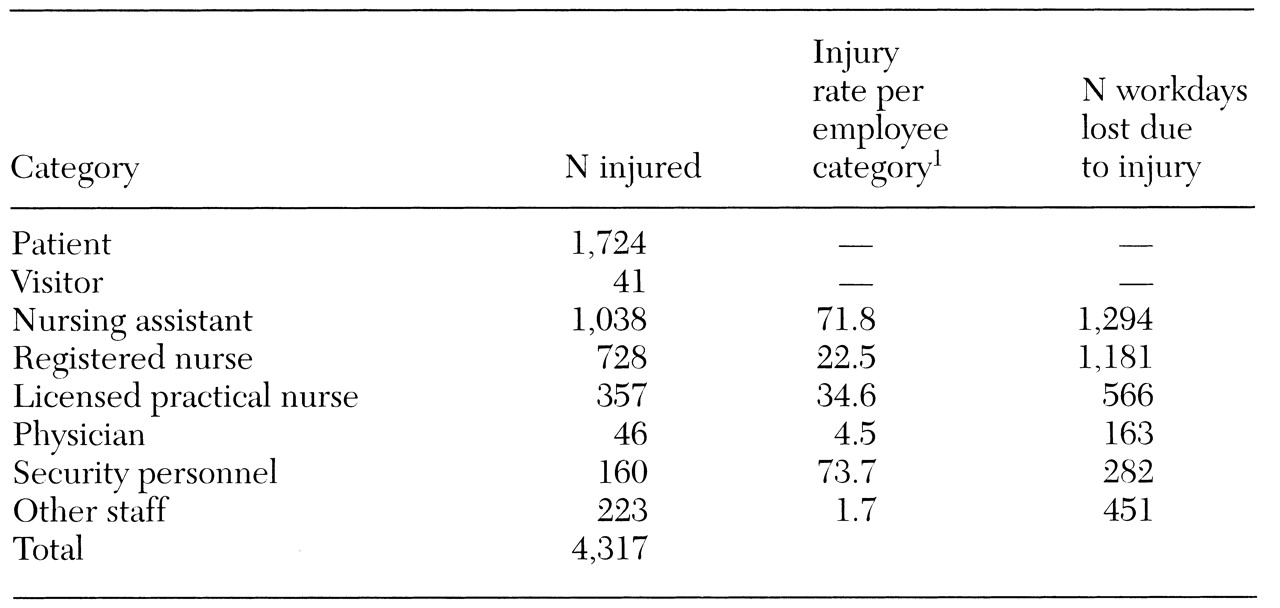
Table 3 presents information on the total number of individuals injured due to assault in various occupational and other categories and the resulting workdays lost. Data from VA centralized staffing reports on the number of employees on duty on the last day of the study year were used to estimate the rate of injury for the various categories of workers. Injuries were most common among nursing personnel. Nursing assistants and security personnel had the highest rates per employee category, with almost one of 14 staff in each of the two groups injured during the study year.
Not all facilities reported the diagnoses of patients involved in assaults. The most common diagnostic category of patients perpetrating assaults was schizophrenia and other psychoses at 71 of the reporting facilities (49.3 percent of the facilities), substance abuse at 23 facilities (16 percent), and dementia at 21 facilities (14.6 percent). Of 122 facilities responding to a question about the most common comorbid secondary diagnosis of those involved in assaults, 54 (44.3 percent) reported that it was a substance use disorder.
The 10 percent of medical centers with the highest rates of assaultive incidents per 1,000 inpatient or residential patients were identified. Of these 17 medical centers, 15 were facilities specializing in the care of psychiatric patients. Conversely, of the 17 facilities that constituted the top 10 percent of facilities with the highest rates of assaultive incidents per 1,000 outpatient visits, which included a cross-section of VA facilities, only three were psychiatric facilities. These findings are relevant to the types of care offered. For example, neuropsychiatric facilities care for more chronically assaultive patients and have less intensive staffing and a larger percentage of patients in inpatient care.
Because assaultive incidents most commonly occurred in inpatient psychiatry units, additional analysis of this portion of the data was undertaken. To equalize the data for workload, the number of assaultive incidents on an inpatient psychiatry unit per 1,000 patients treated in each unit was examined. A significant inverse relationship was found between the number of assaultive incidents per patient treated and the daily cost of direct clinical services for inpatient psychiatric care as reported on the uniform VA cost distribution report (r=-.21, p<.02).
A significant negative relationship was found between the length of stay on psychiatric units and the expenditure per day for direct clinical care (r=-.46, p<.001). VA psychiatric facilities tend to have longer lengths of stay and to spend less per day on direct clinical costs than psychiatric units in VA medical-surgical hospitals (
9). Length of stay was strongly associated with the rate of assaultive incidents per patient treated on inpatient psychiatry units (r=.56, p<.001).
When hospitals were categorized on the basis of how much was expended per day of care, the top 25 percent of hospitals (a mean daily rate of $218.48) averaged significantly fewer assaults per 1,000 inpatient psychiatric patients than the bottom 25 percent (a mean daily rate of $150.08). For the top quartile, the rate was 19.5 assaultive incidents per 1,000 patients treated on inpatient psychiatry units, compared with 46.8 assaultive incidents per 1,000 patients for the bottom quartile (t= 2.19, df=1.62, p=.032).
A total of 139 facilities reported data about staff training on management of assaultive behavior and recommendations from reviews of the incidents. A total of 27,302 staff were given such training at the 139 facilities during the study year. Numbers ranged from no staff trained at 17 facilities to a maximum of 1,419 trained at another facility (63 percent of the total staff). Overall, at the 139 facilities reporting, 20.5 percent of the staff were trained in managing assaultive behavior. The highest rates of training were for nursing service staff (55 percent) and security staff (36 percent). On average, training was provided to only three physicians per facility (less than 4 percent of physicians) during the study year.
A total of 146 of the 166 facilities participating in the survey had formal training programs for management of assaultive behavior, with 21 facilities (12.7 percent) mandating such training. Length of training varied—79 facilities (47.6 percent) reported that training lasted less than one day, 43 (25.9 percent) reported a full day of training, and 26 (16 percent) reported programs lasting two days or longer.
Most training used VA's national curriculum for the management of disturbed behavior. The multimedia training program, which incorporates workbooks, videotapes, and other tools, includes modules on prevention of assault, verbal interventions, physical control techniques, and treatment approaches for disruptive patients. Eighty-four (57.2 percent) of the 146 facilities with formal training programs reported that at least 25 percent of training time was devoted to teaching physical control techniques.
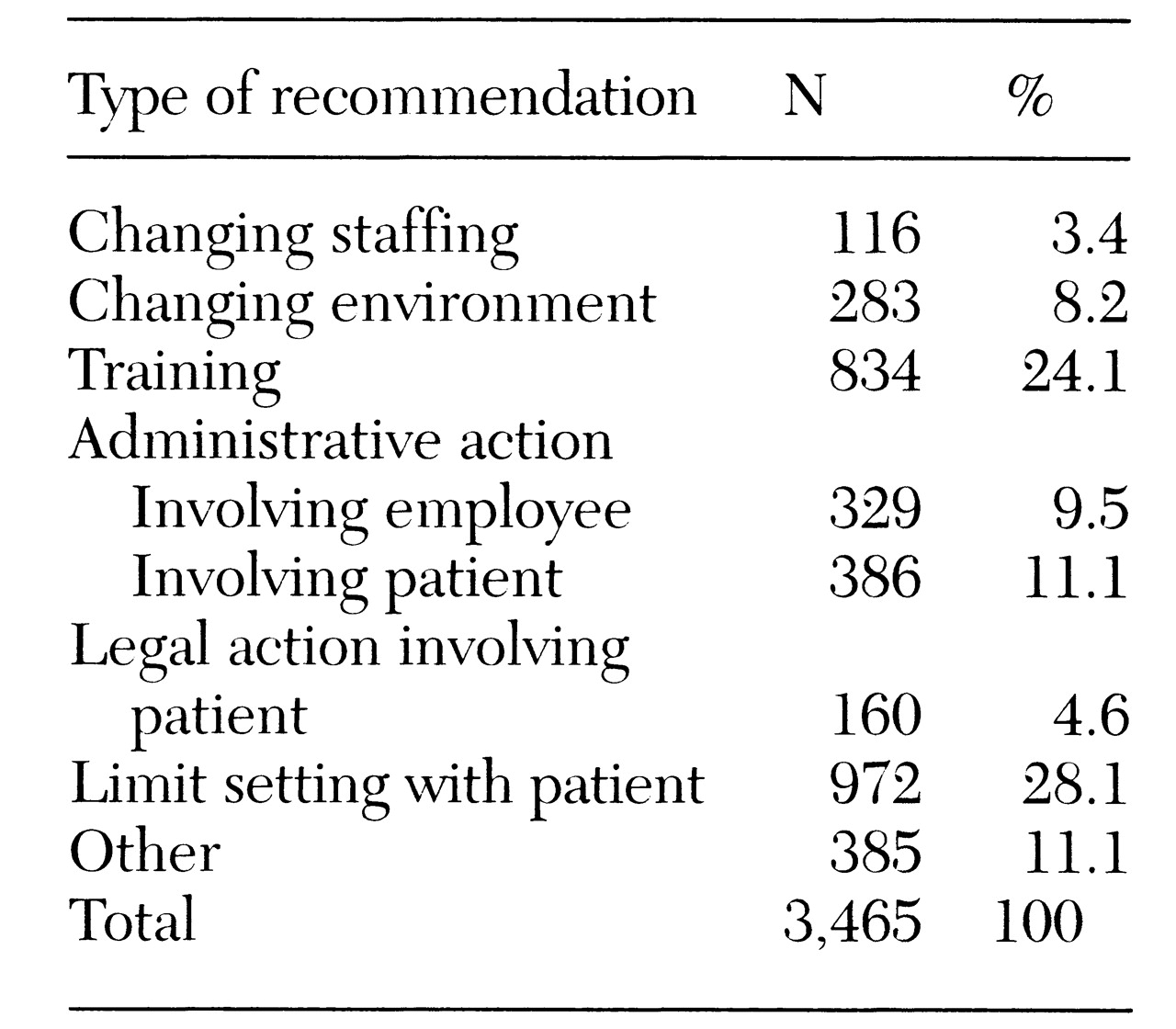
Table 4 categorizes the 3,465 recommendations made after reviews of the assaultive incidents. The most common recommendations involved setting limits on the behavior of patients. They included recommendations to establish systems for flagging problematic patients in the computer to alert staff to their history of violence and the restrictions that had been placed on them, as well as other measures for coping with chronic offenders. Training of staff and administrative action against the perpetrator were also common recommendations.
Discussion
Although a significant number of assaults were reported in this survey, the results indicated that some facilities were not tracking or reporting all assaultive incidents. A previous study of assaultive behavior at a VA neuropsychiatric facility noted that only 44 percent of incidents involving physical assault were formally reported (
11).
In our survey, assaultive behavior occurred most frequently on inpatient psychiatry units, which is not surprising, given the nature of the patients treated there and the fact that during the study year psychiatric beds represented 30 percent (20,049 beds) of the hospital beds in the VA health system. However, the number of incidents in other care delivery sites (43.8 percent of incidents) underscores the reality that assaultive behavior is not confined to psychiatric care settings, and that staff and management throughout the health care delivery system should focus on this problem.
Long-term-care and nursing home units were the second most common inpatient or residential area for assaultive behavior. An earlier study at a VA general hospital with a 206-bed nursing home care unit reported that more than half of assaultive incidents occurred on that unit (
6). In our survey, the number of incidents in outpatient medical-surgical areas was almost identical to the number of incidents in outpatient psychiatry.
The data on incident sites from this study is consistent with limited data from non-VA facilities. The admitting and triage areas of VA medical centers had the second highest rate per work unit of assaultive behavior. This finding is consistent with the results of a survey of emergency departments at 127 large university hospitals, in which 43 percent of the facilities reported at least one physical attack per month (
12). Conn and Lion (
13) examined violence in a university hospital setting and found as many assaults in nonpsychiatric inpatient areas as on the psychiatric unit; the admitting area accounted for 18 percent of assaultive incidents, which is close to our finding that 20 percent of assaults occurred in the admitting-triage area.
Our data on use or possession of weapons and the incidence of battery with a weapon provide a national perspective on the finding of Goetz and colleagues (
14) that in a metropolitan university hospital emergency department, 15.7 percent of medical patients and 17.3 percent of psychiatric patients searched were found to be carrying weapons. In general, VA facilities reporting large numbers of incidents of battery without a weapon were facilities with large psychiatric workloads.
Our finding that the highest incidence of assault-related injuries occurred among nursing staff is consistent with other literature on assault among health care workers (
15). In our systemwide survey, VA staff lost 3,937 workdays due to injury during the study year. Few studies have used this marker of the cost of violence. Lanza and Milner (
16) noted 78 workdays lost due to assault-related injuries over a four-month period at a VA medical center, for an estimated cost to the facility of $6,209. Hunter and Carmel (
17) reported 4,291.5 days lost from work at a large forensic hospital in a year.
The finding that psychosis was the most common diagnosis among assault perpetrators is consistent with other recent findings (
18,
19). The Epidemiologic Catchment Area (ECA) study found that individuals in the general population who met criteria for psychosis had a 21.5 times greater likelihood of assaultive behavior (
20). Consistent with our study, the ECA study found that subjects with comorbid psychosis and substance use disorders had a rate of reported violence 3.6 times higher than individuals with psychosis who did not have a comorbid substance use disorder. Karson and Bigelow (
21) found that 15 percent of 424 VA patients with schizophrenia had been violent during the admission studied. Studies in public psychiatric facilities have noted psychosis as the most common diagnosis among assaultive patients (50 percent to 64 percent); dementias were also common among assaultive patients (approximately 20 percent) (
22,
23). These figures closely parallel the findings of our survey.
Although recognition of the importance of training clinical staff to prevent and manage assault is growing, no consensus exists on the content and length of such training. Most facilities in our survey reported having training programs for staff, but the facilities varied widely in the length of the training course and the number of staff actually trained. Training often focused on staff in psychiatric care areas and was directed primarily toward nursing and security personnel. Lavoie and colleagues (
12) surveyed university hospital emergency departments and reported that only 40 percent provided any formal training for staff on how to manage or prevent assaultive behavior.
The benefit of providing training in management of violence to staff in health care facilities has not been well studied. Lehmann and colleagues (
24) reported that training in a single VA facility improved staff members' knowledge of and performance in handling violent behavior, but the effect of training on the frequency of violent behavior was not evaluated. Results of several studies suggest that training in the management of violence is associated with decreased rates of assault and injury among staff (
7,
25). Our survey found no relationship between the proportion of staff trained and the rates of assaultive behavior at the facilities; however, this study provided only a gross, cross-sectional comparison of training rates and rates of assaultive behavior.
The literature on the relationship between staffing on inpatient psychiatric units and assaultive behavior is sparse. Reports from single-facility psychiatric units have linked increased violent behavior with lack of adequate or stable staffing and a physical environment not conducive to good patient control (
6,
26,
27,
28), but these studies have limitations. Our data indicate a negative correlation across all facilities between expenditures per day for direct care on psychiatric units and the rate of assaultive behavior per patient treated on these units. We also found a substantial correlation between length of stay and the total amount expended on direct care per day. This finding likely reflects the reality that staffing as listed on VA cost distribution reports is generally lower in psychiatric hospitals than in academically affiliated acute facilities. VA psychiatric facilities are also characterized by longer lengths of stay.
Because the rate of assaultive behavior on inpatient psychiatric units is also strongly associated with length of stay, it is impossible to clearly establish the relationships between expenditures for direct care, length of stay, and the rate of violence. However, the data suggest the importance of evaluating staffing levels carefully, particularly when the patient population may be prone to assaultive behavior. The importance of such evaluation is underscored by our finding that 11.6 percent of all recommendations made after the incidents were reviewed involved changing the staffing or the environment.
Conclusions
The survey on assaultive behavior was part of VA's ongoing program on prevention and management of assaultive behavior, which is designed to decrease the number of such incidents and the attendant injuries. We confirmed the significance of violence in VA settings and found that certain aspects of violent incidents, such as rates, location, and patient demographic characteristics, were consistent with findings of other, smaller studies. We noted a risk of assault in nonpsychiatric settings, including nursing homes and medical-surgical inpatient and ambulatory care sites. We found an inverse correlation between expenditures on staffing on inpatient psychiatric units and the frequency of assault.
The results of the survey were disseminated throughout the VA health care system. Subsequently, new training modules for the physical restraint of patients and the management of dangerous situations in ambulatory care settings were developed. The use of computerized flagging and specialized treatment planning for individuals with histories of repeated violence in admission and triage areas (
29) was also expanded.
Based on the findings of this study, we have several recommendations for consideration by all health care facilities and systems. Health care staff should be made aware of the prevalence of assaultive behavior, especially among patients with a psychiatric diagnosis, including those with substance abuse. Training in the prevention and management of assaultive behavior should be mandatory for all staff members who have frequent direct contact with clinical populations. As health care becomes increasingly based in ambulatory settings, outpatient sites need to pay special attention to the assessment and management of assaultive behavior. Facilities should incorporate ongoing monitoring of assaultive behavior into their quality improvement activities. More research is needed on the relationship between violence and staffing levels on inpatient psychiatric units and on enhancing the efficacy of training in the management of violence.