In a review of the literature, Felker and associates (
1) demonstrated consistently higher mortality rates for individuals with severe and persistent mental illness compared with the rate in the general population. The finding has been replicated internationally, for a variety of diagnoses and for both natural causes and unnatural causes such as accidents, suicides, and homicides. It has also been shown that the high mortality rate cannot be attributed solely to poverty (
2).
Although a variety of factors can contribute to the high mortality rate among mentally ill persons, one that certainly needs to be looked at is the physical health care they receive. The literature suggests that patient, provider, and systems issues can interfere with the ability of persons with severe mental illness to receive appropriate health care (
3). Provider and patient issues include inconsistency of the primary care provider, providers who do not like working with mentally ill individuals, and psychiatric symptoms that interfere with the ability to detect and communicate health-related problems and compliance with care (
4,
5). Systems problems often revolve around the fact that mental health care and physical health care in the public sector are provided through quite separate organizational structures (
6). This bifurcated approach creates communication barriers between providers and inconveniences for patients.
Thus the two primary issues to address in improving the physical health of persons with severe mental illness are the high mortality rate and a delivery system that makes it difficult to receive coordinated care (
7,
8). As a first step in designing a coordinated system of care, our research focused on quantifying health care utilization patterns of persons with severe and persistent mental illness.
Methods
Medical claims for physical health care of 220 Medicaid enrollees with severe and persistent mental illness were compared with medical claims of a randomly selected group of 166 Medicaid patients who were not enrolled in the public mental health system. The two groups were comparable to the extent that all individuals were enrolled in the same health plan under the auspices of the Arizona Health Care Cost Containment System (AHCCCS) and were between the ages of 21 and 65. The two groups were similar in gender, age, and ethnicity. Of the entire sample, 48 percent were men, and 52 percent were women. The mean age was 34, and 70 percent were Anglo, 8 percent were black, and 18 percent were Hispanic. Although income data were not available, Medicaid eligibility in Arizona is quite restrictive, and recipients' income must be no higher than 30 percent of the federal poverty level.
To be included in the sample, an individual needed to be enrolled in the AHCCCS health plan for the entire year that claims data were sampled—July 1994 through June 1995. The individuals with severe and persistent mental illness also had to be enrolled in the mental health carve-out program for that entire year.
Because AHCCCS health plans are run as managed care systems, there is a single database for all physical health care claims regardless of service setting, provider, or service type. The cost associated with each claim was based on the health plan reimbursement rate for the particular service.
Because the purpose of the study was to evaluate use of physical health care, claims related to mental health and substance abuse were not included in the analysis. Services related to pregnancy and childbirth were also excluded due to the higher fertility rate for the population without mental illness.
The data were analyzed in three ways: by total medical claims, service setting, and diagnostic category. All services were classified as having taken place in one of six settings: outpatient office, outpatient hospital, outpatient surgical setting, inpatient setting, emergency room, and ambulance. Statistical analysis was not conducted.
Results
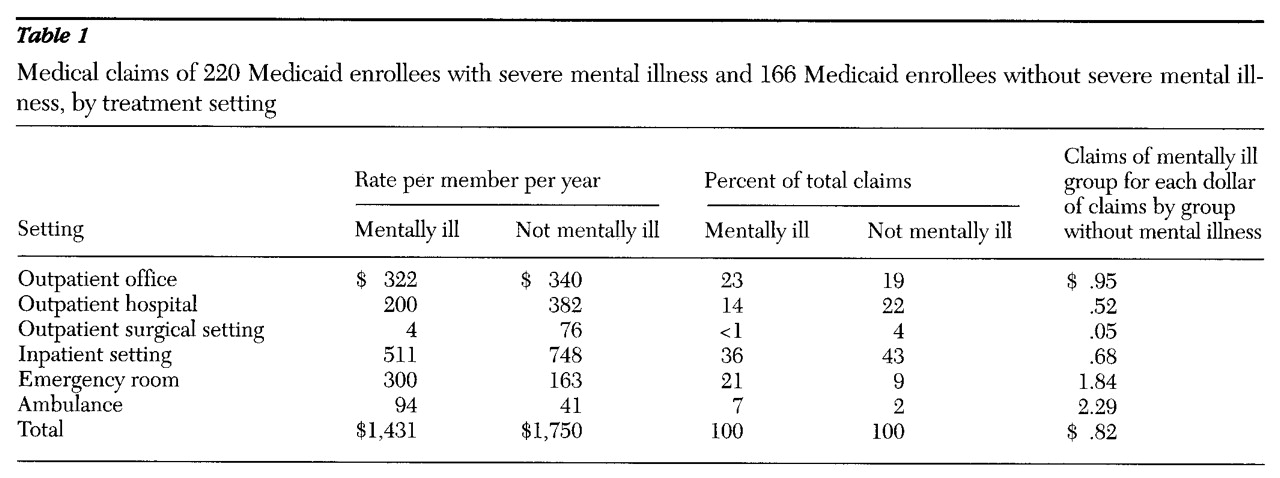
As shown in
Table 1, the total health care claims per member per year for the groups with and without severe mental illness were $1,431 and $1,750, respectively. The total amount for the mentally ill group was 18 percent less than the amount for the group without mental illness.
Table 1 also shows that the distribution of claims for the two groups differed across service settings. Individuals with severe mental illness had a lower rate of health care claims than the group without mental illness for outpatient hospital care ($200 per member per year versus $382), outpatient surgical care ($4 versus $76), and inpatient care ($511 versus $748), but a higher rate of claims for emergency rooms ($300 versus $163) and ambulances ($94 versus $41).
Twenty-eight percent of the health care dollar for patients with severe mental illness went to emergency rooms and ambulances, compared with only 11 percent for the patients without mental illness. On the other hand, 26 percent of the health care dollar for the group without mental illness went to outpatient surgical and outpatient hospital settings, compared with 14 percent for the mentally ill group.
Although both groups received care for similar physical health diagnoses, the settings where they obtained treatment for those diagnoses differed in some instances. An important example is genitourinary diagnoses. These conditions accounted for 8 percent of outpatient office claims for the group without mental illness, compared with less than 1 percent for the mentally ill group. Persons with mental illness who had these conditions were treated in more acute settings. Genitourinary diagnoses accounted for 19 percent of inpatient claims and 3 percent of emergency room claims for the mentally ill group, compared with less than 1 percent and .1 percent, respectively, for the group without mental illness. Thus the patients without mental illness generally received treatment in an outpatient office setting, whereas mentally ill patients with the same diagnosis appear not to have received treatment until a more urgent setting was mandated.
Discussion and conclusions
This study found that for every dollar in physical health care utilized by Medicaid enrollees without mental illness, enrollees with severe mental illness utilized 82 cents. In addition to using fewer health care resources, mentally ill individuals appeared to have a different pattern of health care utilization. Their rates of treatment utilization in urgent care settings were higher than those for their counterparts without mental illness, which appeared to be the case even for the same diagnoses. The relatively high rate of use of emergency services among these individuals is even more significant in light of the fact that Medicaid patients as a group tend to be high users of emergency services (
9). Thus, individuals with severe and persistent mental illness appear to stand out as high users of emergency services even in a high-user population.
Admittedly, patterns of service utilization do not necessarily provide information about the appropriateness of the health care received. When individuals have few support systems, minimal access to transportation, and a primary care physician with whom they are likely not familiar, seeking care in an emergency room might be an adaptive approach to obtaining health care. However, in a system designed to meet the needs of mentally ill persons, emergency treatment of routine illnesses might become less necessary.
The results of this research formed the foundation for design of a clinic to coordinate physical and behavioral health care for individuals with severe and persistent mental illness. The design provides for co-location of staff, shared records, coordination of care, and financial incentives for shifting treatment from the emergency room to the outpatient setting. It is anticipated that the clinic will improve health care delivery and the health status of those enrolled.
Acknowledgments
The authors are grateful to the late Alan Beigel, M.D., for helping to conceptualize this project and for securing the funding to carry it out. The research was made possible through funding from the Flinn Foundation.