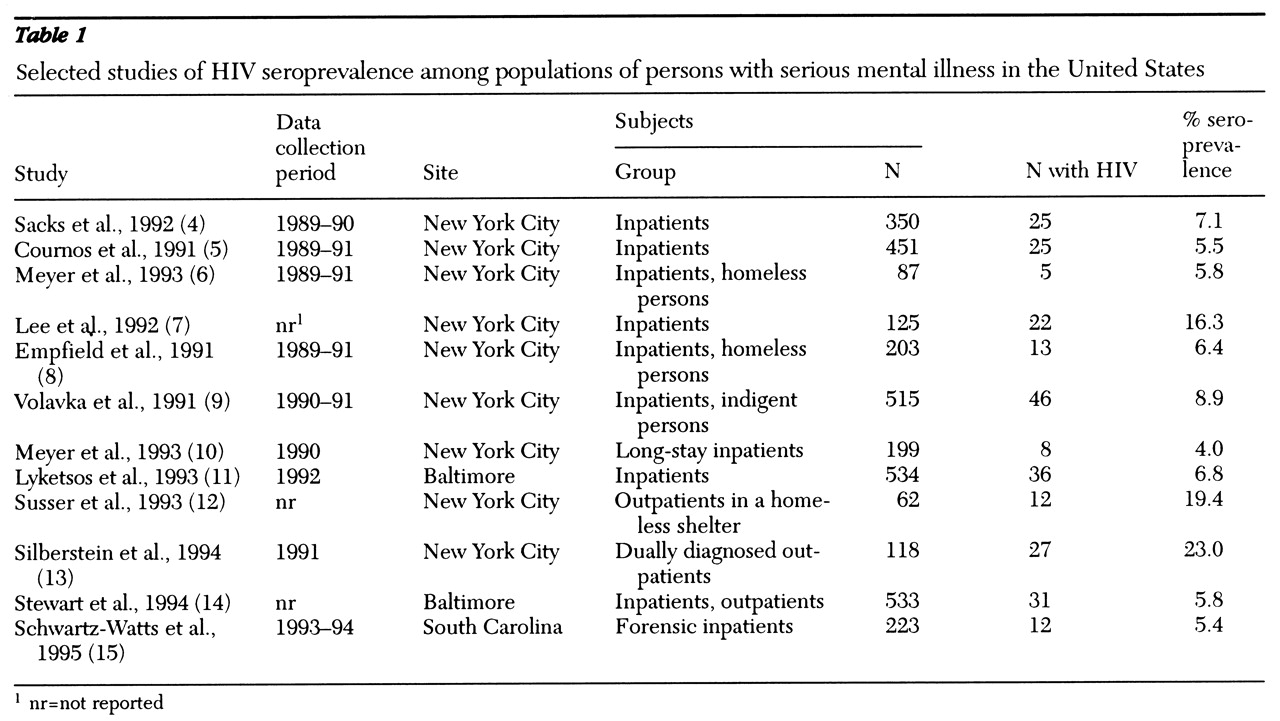
Since the late 1980s, evidence has been accumulating that persons with serious mental illness constitute a group at higher risk for infection with human immunodeficiency virus (HIV) than the general population (
1,
2). Although infection rates for the general population are about .3 percent (
3), they are much higher among persons with serious mental illness—as high as 23 percent in programs in the Northeast for special populations, such as homeless and dually diagnosed persons (
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15) (see
Table 1). Clearly, concerted efforts will be necessary to reduce the spread of HIV among persons with serious mental illness and to effectively treat those who are already infected. Public mental health systems can play a key role in such efforts.
This paper highlights current issues related to reducing HIV risk and effectively treating HIV infection in the seriously mentally ill population. We will discuss barriers to providing adequate care for this population and suggest ways in which public mental health systems can address these issues.
Methods
MEDLINE was searched for literature on HIV infection among persons with serious mental illness. All pertinent references published between 1980 and 1988 were obtained and reviewed.
HIV risk factors
Serious mental illness typically has its onset when patients are in their later teens or early twenties. In most cases of co-occurring serious mental illness and HIV, the mental illness preceded the HIV infection. However, providers are more frequently seeing patients whose serious mental illness appears to have begun after they contracted HIV (
16). Although many persons with HIV experience psychiatric problems, such as anxiety and depression, a smaller number develop psychotic symptoms, usually in late-stage HIV disease. It is sometimes unclear whether the psychotic illness has occurred secondary to HIV central nervous system involvement or has developed independently (
17).
Regardless of etiology, persons with serious mental illness share certain characteristics that affect their risk of acquiring or transmitting HIV. Although a smaller portion of persons with serious mental illness are sexually active compared with the general population, those who are active engage in sexual behaviors that involve higher risk for HIV infection (
18,
19,
20,
21). This high-risk activity may partly derive from poor interpersonal functioning, especially as the onset of serious mental illness often interferes with normative psychosocial development. Further, chronic mental illness itself is often associated with poor judgment, affective instability, and impulsiveness. The use of drugs and alcohol, endemic in many segments of the serious mentally ill population, may further impair individuals' ability to respond safely in high-risk situations.
The sexual activity of seriously mentally ill persons tends to occur within casual rather than long-term relationships or with others who are also socially marginalized, and it is often characterized by naiveté, abuse, and exploitation (
22,
23). Researchers in a variety of clinical settings across the U.S., not only in high-risk HIV "epicenters," have documented very high rates of unprotected sex with multiple casual and high-risk partners among persons with serious mental illness (
24). Among certain seriously ill populations, including homeless persons, the practice of trading drugs for sex is common (
12,
21).
Little is known about seriously mentally ill persons' risk for HIV through injection drug use. Although lifetime rates of injection drug use appear to be quite high in this population—ranging from 6 percent in Milwaukee (
18) to 15 percent in New Orleans (
20), 17 percent in Tampa (
21), and 20 percent in New York City (
25)—relatively little information about how these drugs are used is available. We know little about how persons with serious mental illness learn to inject themselves or the extent of their knowledge about or participation in safe injection practices, such as the use of bleach to clean needles or needle exchange programs.
Although knowledge about HIV transmission and HIV-related illness among persons with serious mental illness varies by study site—perhaps reflecting regional rates of AIDS cases—overall it is comparable to knowledge about AIDS in the general population (
26). A diagnosis of schizophrenia has been associated with variation in knowledge about HIV in some, but not all, studies. The presence of symptoms, such as delusions or hallucinations, may be a more important predictor of risk than diagnosis or knowledge about AIDS (
26).
Many public mental health systems have been responsive to the educational needs of clients with serious mental illness (
27,
28), but knowledge alone is unlikely to result in effective prevention (
21). Cognitive-behavioral interventions designed to lower HIV risk have been successfully tested, but reductions in risk behaviors appear to be time limited and to require "booster" interventions to maintain behavioral gains (
29). Such interventions, which are costly and labor intensive, are not widely used in public mental health systems.
Even before the HIV epidemic, about 50 percent of serious physical disorders among seriously mentally ill persons who were receiving psychiatric treatment went undetected (
30,
31) and mortality rates, excluding deaths from suicide, far exceeded those of the general population (
32,
33). Obtaining treatment for an illness that has been detected requires locating an appropriate health care provider, making an appointment, obtaining transportation to the site, and paying for the services or arranging reimbursement—a daunting set of activities for many seriously mentally ill persons. Some in this population, especially those who are chronically homeless, avoid formal service delivery systems altogether, ignoring health problems until they become unmanageable (
34).
In the case of HIV, treatments with newer antiretroviral regimens require dosing on a rigid schedule, often with several different agents. Some observers have suggested that seriously mentally ill persons may not be appropriate candidates for treatment with these complex regimens (
35). However, we know very little about whether they are able to manage such regimens or to benefit from methods that have improved adherence for others.
Persons with serious mental illness also tend to be unemployed and poor. They are overrepresented among or live in close proximity to other disadvantaged groups at very high risk for HIV, such as homeless persons, those who are incarcerated, and impoverished ethnic minorities (
36,
37,
38). Like these groups, seriously mentally ill persons lack political power and may lack strong advocates for better HIV-related care. They are stigmatized by both their mental and their HIV-related illnesses. Physical health providers may be less inclined to do a careful workup of a person with serious mental illness who presents with early symptoms of HIV infection or AIDS, while mental health providers may be reluctant to treat clients who are HIV positive. Clients lack resources to purchase materials essential in preventing HIV infection, such as condoms (
21), or to buy expensive antiretroviral medications out-of-pocket.
Barriers to care
Barriers to detection and effective treatment exist at the individual level of client and provider and within service delivery systems, such as clinics, hospitals, and mental and physical health systems. Persons with serious mental illness, particularly those whose mental illness preceded their HIV diagnosis, most commonly enter formal treatment through public mental health systems. These systems are thus positioned to play a critical role in the detection and treatment of HIV-positive clients. However, many public-sector mental health systems appear reluctant to address issues of HIV, perhaps because of concerns about confidentiality, clients' mental competency, and public responsibility associated with treating HIV-positive persons with serious mental illness (
11).
In 1995 we surveyed nine large metropolitan public mental health systems in the U.S. and found striking variation in HIV risk and detection policies for seriously mentally ill populations. The policies ranged from aggressive risk screening and HIV testing to strong discouragement of staff's even inquiring about or documenting clients' HIV status (Sullivan G, unpublished data, 1995).
Public mental health systems that have distanced themselves from addressing HIV risk among their clients have done so ostensibly because of fears that confidentiality could not be assured. However, failing to detect HIV or to assess risk for HIV also relieves these already underfunded, overburdened systems from having to take responsibility for a problem that is potentially very costly. In several seroprevalence studies conducted in New York City, where risk screening is mandated, as many as three-quarters of HIV-positive clients were not known by providers to be infected with HIV (
5,
9,
39). In other systems of care, rates of detection are likely to be even lower.
Even before the HIV epidemic, public mental health systems had long faced problems in helping their clients receive adequate physical health care. These systems have used a variety of methods of delivering physical health care, including direct service provision, contracting out for services, and coordinating services across a range of agencies. Although some newer managed care wraparound plans in public mental health systems have included physical health care, it is not considered a specific responsibility of these systems. Many seriously mentally ill persons have Medicaid, but access to care, particularly high-quality physical health care, is often problematic (
40).
To obtain needed treatment, persons with serious mental illness are usually required to navigate between several publicly funded "systems" of care, including the public mental health system, the public physical health care system, and the sectors that manage entitlements, such as publicly funded health insurance. In the best of scenarios, case managers help with this task. However, many persons with serious mental illness lack case managers; for others, the size of the managers' caseloads prevents meaningful assistance (
41). The needs of seriously mentally ill persons can easily fall through the cracks. Providers, especially HIV experts who are inexperienced in treating persons with serious mental illness, often find them difficult to manage. Coordination between public mental health and physical health care providers may be a challenge, as neither group may be willing or able to assume ultimate responsibility for the patient (
42).
One recent development is the creation of integrated mental health- HIV programs, many of which have been funded through the Ryan White CARE Act. Yet informal surveys of these integrated programs find that those enrolled are often not the traditional "seriously mentally ill" clients, but are HIV-positive individuals who are depressed or anxious, who are difficult to treat, or who do not "fit in" in other treatment settings, such as substance abuse treatment programs.
In a recent pilot study conducted by our group in an integrated mental health-HIV program in the Northwest, most clients labeled "seriously mentally ill" actually had histories of intravenous drug use and carried diagnoses of psychotic disorder not otherwise specified (Sullivan G, Perlman J, Koegel P, et al, unpublished report, 1998). Most were not currently taking antipsychotic medication and were much higher functioning than typical persons with schizophrenia. Thus even though efforts have been made to create programs that better integrate mental and physical health care, such programs are relatively rare, and they may not engage "typical" seriously mentally ill populations.
Providers' concerns about interactions between antiretroviral medications and psychiatric medications pose other problems. Some antiretroviral medications, especially the protease inhibitor saquinavir, have package inserts that warn about the concurrent use of specific psychotropic medications based on the theoretical potential for elevating the blood levels of these drugs. While we await published clinical data, clinicians can nonetheless find successful regimens by either choosing alternative psychotropic agents or using lower doses and carefully monitoring the patient (
43).
Little is known about the optimal management of seriously mentally ill persons in the later stages of HIV illness, when HIV-related neuropsychiatric symptoms may appear in combination with increased sensitivity to side effects of antipsychotic medications. Additional research on drug interactions should be a high priority.
At least one report has found that psychosis decreases survival time among persons who are HIV positive, even after adjusting for race, age, opportunistic infections, and cluster of differentiation (CD-4) cell count (
44). Such findings may not be surprising given what we know about the barriers to treatment, the difficulties involved in integrating mental and physical health care, and the challenges involved in detecting illness and managing treatment of seriously mentally ill persons with serious physical comorbidities of any type. Yet the findings surely represent a challenge to public mental health systems, consumer advocacy groups, and researchers to increase efforts to improve the quality of HIV treatment for persons with serious mental illness and to address the many issues that remain unstudied.
Role of public mental health systems
A variety of interventions exist that could decrease risk and improve detection of HIV for seriously mentally ill persons and ensure better care for those who are HIV positive. To improve detection, public mental health systems should routinely obtain HIV-related risk histories that can classify clients into high-, medium-, or low-risk groups; the systems should then offer and strongly encourage HIV testing and counseling, especially for those whose histories suggest any risk and for all pregnant women.
To decrease risk for infection and prevent further transmission of HIV, public mental health systems should:
• Implement programs to increase all clients' awareness of HIV-related issues.
• Make condoms available free of charge. This measure is far less expensive that treating HIV-related illness.
• Provide information about and facilitate access to needle exchange programs and use of bleach to clean injection equipment.
• Offer selected groups of high-risk clients intensive behavioral risk-reduction interventions to reduce their risk of acquiring and transmitting HIV and other sexually transmitted infections.
To improve treatment effectiveness, public mental health systems should:
• Educate mental health providers, especially those who work with HIV-positive clients, about what constitutes appropriate treatment for HIV-related illnesses so that they can provide at least rudimentary monitoring of treatment. For example, clients who are HIV-positive but are asymptomatic should have an assessment of immune status (viral load, CD-4 cell count) at regular intervals.
• Educate mental health providers about common medical complications of HIV and the typical medications used to treat HIV-related conditions.
• Educate physical health care providers who treat HIV-positive clients with serious mental illness about the concurrent use of psychotropic and HIV medications and provide consultation when psychiatric symptoms interfere with medical management.
• Offer education and support to family members of HIV-positive clients as appropriate.
• Require programs that offer integrated mental health-HIV treatment to target "traditional" seriously mentally ill persons.
• Create formal or informal arrangements with local public health providers to ensure coordinated treatment of HIV-positive clients.
• Provide every seriously mentally ill person who is HIV positive with effective case management, either through the public mental health system or the public physical health care system.
• Create forums to examine the reluctance of public mental health systems to address HIV-related issues in seriously mentally ill populations.
• Ensure through appropriate local mechanisms that expensive antiretroviral medications will be available to appropriate seriously mentally ill clients.
• Advocate for the inclusion of seriously mentally ill persons or their family members in local political processes involving HIV treatment services.
Conclusions
The HIV epidemic has posed complex challenges for health care systems and providers across the U.S. The particular challenges at each point in the epidemic's history have varied for different high-risk populations, such as gay and bisexual men and intravenous drug users, reflecting differences in their formal and informal support networks and in the organization and financing of health care systems that typically serve these populations.
Even before the HIV epidemic, the provision of adequate physical health care to persons with serious mental illness was often problematic. Nevertheless, now that efficacious treatments for HIV-related illnesses exist, it is critical that public mental health systems take a proactive approach to detecting and treating HIV-related illnesses among their clients. Additional research is needed to address several important issues for this population, including improving adherence to antiretroviral treatment regimens, improving management of concurrent provision of antipsychotic and HIV-related medications, and integrating mental and physical health care. Meanwhile, a number of interventions outlined in this paper are possible. To be optimally effective, public mental health systems will need to tailor these policies and practices to best suit local circumstances.
Acknowledgment
This paper was supported by grant 3RO1-MH-55936-0251 from the National Institute of Mental Health.