Urinary incontinence is a common and disabling condition among community-dwelling (
1) and institutionalized (
2) persons, with prevalence rates of 3% to 60% (
3), which increase with age (
4). Costs associated with incontinence are significant (
5), and the condition is an independent risk factor for institutionalization (
6). Although there is an extensive database on urinary incontinence in the general and institutionalized aged populations, little information exists for younger cohorts or those with mental illnesses.
Most related studies among persons with mental illness have focused on women, small samples, certain medical conditions, and medications. Furthermore, previous work has shown that urinary incontinence does not figure prominently in the person's care plan and is not perceived as being an important clinical concern in inpatient psychiatry (
7). This exploratory study examined factors associated with urinary incontinence by using population-level data for persons admitted to inpatient psychiatric care in Ontario, Canada. It also examined differences in these factors by age group.
Methods
In 2005 the Ontario Ministry of Health and Long-Term Care mandated the use of the Resident Assessment Instrument-Mental Health (RAI-MH) in adult inpatient psychiatric facilities. The ministry also required submission of data to the Canadian Institute for Health Information's Ontario Mental Health Reporting System. This study analyzed admission data for 41,004 individuals assessed between October 2005 and June 2007. Ethics approval for secondary analyses of deidentified data was provided by the University of Waterloo Office of Research.
The RAI-MH is a comprehensive assessment instrument that is completed within the first three days of admission to an inpatient psychiatric facility (
8). Its 400 items evaluate status in key domains, including mental state, substance use, risk of harm to self and others, behavior disturbance, role functioning, social engagement and support, stressors, cognitive performance, self-care skills, communication, physical health, medications, and service utilization. The assessment is completed in about one hour by trained clinical staff. A detailed manual is available (
9). Psychometric properties of the RAI-MH have been reported elsewhere (
10).
The RAI-MH assesses bladder continence over the past three days with an item that uses a 7-point scale: 0, continent; 1, control with a catheter; 2, infrequent incontinence; 3, episode of incontinence; 4, occasionally incontinent; 5, frequently incontinent; and 6, incontinent. For this study, urinary incontinence was defined as any instance of incontinence—that is, a score of 1–6.
RAI-MH items used in this study include age; sex; psychiatric diagnoses; presence of an intellectual disability; self-rated health; dizziness, vertigo, or light-headedness; dry mouth; difficulty urinating or polyuria; flat or blunted affect; sleep problems; easily distracted; periods of altered perception; history of sexual, physical, or emotional abuse; electroconvulsive therapy or chair restraint; medication adherence; psychotropic medications stopped because of side effects; and intentional medication misuse. Validated scales that are embedded in the RAI-MH were also used; these scales are related to depression (
11), positive psychotic symptoms (
7), anhedonia (
7), pain (
12), health instability (
13), cognition (
14), and self-care (
15).
All analyses were performed with SAS, version 9.1. Before multivariate logistic regression models were developed, collinearity was assessed. To determine which factors were independently associated with urinary incontinence, unconditional multivariate logistic regression was performed for each age group. Only statistically significant (p<.05) findings are reported.
Results
Overall, patients were in their mid-forties (mean±SD age=44.6±16.8). Most were male (51.2%, N=20,983) and occupied acute care beds (81.6%, N=33,449). Primary provisional psychiatric diagnoses included mood disorders (41.6%, N=16,546), psychotic disorders (31.6%, N=12,538), substance use disorders (14.5%, N=5,746), delirium or dementia (4.7%, N=1,861), and anxiety disorders (3.0%, N=1,186).
The overall prevalence of urinary incontinence was 6.2% (N=2,547). Prevalence was higher among women (6.8% of women, N=1,358, and 5.7% of men, N=1,189; p<.001) and among older adults (under age 45, 2.0%, N=451; aged 45–64, 5.9%, N=789; and aged 65 and older, 25.2%, N=1,307; p<.001). A significant age-sex interaction was found: women had higher rates of incontinence than men before age 65 (under age 45, 2.4% versus 1.7%, p=.001; and aged 45–64, 6.6% versus 5.1%, p<.001) and lower rates than men at age 65 and older (22.1% versus 29.4%, p<.001).
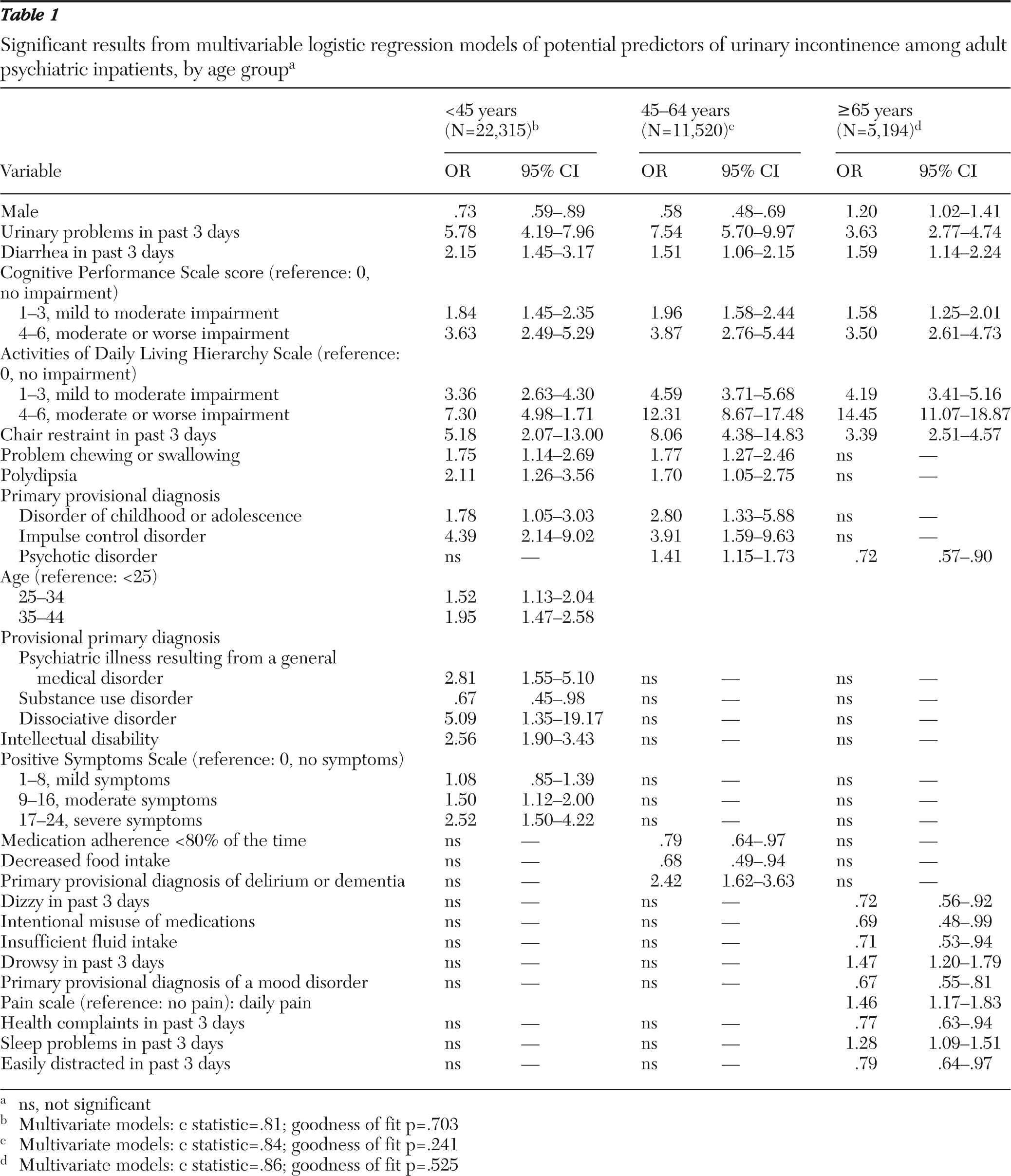
Table 1 shows the significant results of the multivariate analyses for the three age groups. Some variables had positive associations with incontinence for all age groups, including urinary problems, diarrhea, cognitive impairment, functional impairment, and chair restraint. In the two younger age groups, problems chewing or swallowing, polydipsia, and a primary provisional diagnosis of a disorder of childhood or adolescence or an impulse control disorder were positively associated with incontinence.
Variables that were associated with incontinence only among patients under age 45 included a primary provisional diagnosis of dissociative disorder and of a psychiatric illness resulting from a general medical disorder. Although a primary provisional diagnosis of a psychotic disorder was not significantly associated with incontinence in this age group, presence of positive psychotic symptoms was. Having an intellectual disability and increasing age (within this age group) were also positively associated with incontinence. A primary provisional diagnosis of a substance use disorder was associated with decreased odds of incontinence among those under age 45.
Among patients aged 45–64, a primary provisional diagnosis of delirium or dementia more than doubled the risk of incontinence, whereas being adherent to medications less than 80% of the time and having a decreased food intake reduced the risk.
For patients aged 65 and older, an increased risk of incontinence was associated with drowsiness, daily pain, and sleep problems, whereas dizziness, intentional misuse of medications, insufficient fluid intake, a primary provisional diagnosis of a mood disorder, health complaints, and being easily distracted decreased the risk.
Discussion
This is the first large-scale investigation of urinary incontinence that examined both prevalence and factors independently associated with this condition among psychiatric inpatients. A prevalence of 6.2% was found, and although incontinence was more common among older adults, it was still a problem for younger patients. Furthermore, findings suggest that several factors amenable to intervention were positively associated with urinary incontinence across the three age groups, including diarrhea, poorer cognitive and physical functioning, and use of chair restraint.
This study is not without limitations. First, the cross-sectional nature of the data limits our understanding of the direction of the effects. Second, the lack of information on general medical conditions and specific medications used prevented us from examining potential causes of incontinence. Although the RAI-MH documents medical diagnoses and the medications that patients are taking, inclusion of this information in the national database had not been mandated at the time of this study. Some of the significant factors that we identified, such as intellectual disability or dementia, may not have been significant in multivariate models that included information on medications. Therefore, findings reported need to be put into the context of general medical comorbidity, because we were unable to control for that. However, it is expected that such data will be available in the future. Third, lack of detail about the type of urinary incontinence and corresponding symptoms limits understanding of the issue.
Conclusions
Urinary incontinence is an abnormal condition—not a normal part of aging or an expected condition among psychiatric patients—and the prevalence rate found in this study is higher than some might have imagined. Future work is needed that examines the extent to which urinary incontinence persists beyond hospital admission and how general medical diagnoses and medications alter the relationships reported here.
Acknowledgments and disclosures
The authors report no competing interests.