Patients who have had psychiatric hospitalizations have more severe illnesses, higher psychiatric and medical costs, and are at greater risk of poor outcomes, including subsequent hospitalizations and suicide (
1–
3). Patients treated in inpatient psychiatric settings tend to have higher rates of co-occurring psychiatric illnesses, and the co-occurring substance use and comorbid disorders have been found to be strong predictors of poor prognosis (
4), including subsequent rehospitalization. In our prior work using administrative data from the U.S. Department of Veterans Affairs (VA) health care system, we found that the rate of completed suicide in the first 12 weeks after inpatient discharge was approximately five times the base rate in the overall VA patient population treated for depression (
5).
Close clinical monitoring of individuals during the high-risk postdischarge period has been suggested to reduce adverse outcomes (
6). Continued care after a hospitalization for mental illness supports the patient's transition back to the community and may reduce rehospitalizations for some individuals. Alternatively, close clinical monitoring may facilitate readmission if individuals are again in crisis (
7,
8). Although rehospitalization after discharge can occur for a number of reasons, it is often considered a proxy indicator of worsening or severe psychiatric symptoms and may result from less-than-optimal discharge planning (
9). In the general medical literature, rehospitalization is considered an adverse outcome and an indicator of poor-quality care.
The Healthcare Effectiveness Data and Information Set (HEDIS) currently calls for at least one outpatient visit in the first seven days or the first 30 days after psychiatric inpatient discharge to reduce suicide risk (
10). Although closer monitoring is recommended, no studies have shown definitively the effectiveness of increased monitoring in the posthospitalization period and improved patient outcomes. In this study, and on the basis of our prior work (
5), we focused on the effect of the intensity of monitoring during the first 12 weeks postdischarge from a psychiatric hospitalization in which acuity remains high as evidenced by high suicide risk.
The goal of this study was to assess whether increased monitoring (specifically, mental health and substance use outpatient visits) is associated with decreased risk of psychiatric rehospitalization in the overall population of patients with depression who are discharged from a psychiatric hospitalization. Given that patients treated in inpatient psychiatric settings tend to have higher rates of co-occurring psychiatric illnesses and substance use disorders, which have been found to be strong predictors of poor prognosis (
4), we also assessed whether increased monitoring might be more important in key subgroups of patients. Specifically, we hypothesized that increased monitoring is protective for patients with a diagnosed substance use disorder, other anxiety disorders, or posttraumatic stress disorder.
Methods
Study cohort
Study data were drawn from a large cohort of 887,859 unique patients receiving depression treatment between April 1, 1999, and September 30, 2004, in the Veterans Health Administration (VHA) health system. Patients were included in the depression treatment cohort if they received both a diagnosis of a depressive disorder and an antidepressant medication fill from VHA providers or if they had two visits with diagnoses of depressive disorders. Several prior studies and accrediting agencies have used similar definitions to define cohorts with depressive disorders when examining the quality of care for depression (
5,
11–
13). Patients were excluded if they received any diagnoses of bipolar disorder type I, schizophrenia, or schizoaffective disorder during the study period. The study was conducted with institutional review board approval from the VA Ann Arbor Health System.
Because of potential treatment indication bias, where more severely ill patients are more likely to be monitored postdischarge and more likely to be rehospitalized, a matched case-control design was used (
14,
15). In addition to the advantage of addressing potential treatment indication bias, a matched case-control design gives an added analytic advantage where specific functional relationships between potential confounding variables and the outcome of interest do not have to be specified.
We first identified all patients with at least two psychiatric hospitalizations in the depression cohort. These patients made up the case group in which the event of interest was a rehospitalization after discharge from the first (index) psychiatric hospitalization. No patient was included in the case group more than once. For each case, a control group was sampled from the source population (that is, patients who were discharged from a psychiatric hospitalization) who were at risk of rehospitalization when the patient in the case group was rehospitalized. Specifically, patients in the control group had to have a psychiatric hospitalization during the same fiscal year as the case group counterpart's index hospitalization and be alive and not rehospitalized for the number of days between the case group patient's discharge and subsequent rehospitalization. This sampling from the risk set accounted for time at risk because control group patients were matched to case group patients with respect to sampling time.
For each patient in the case group, up to two control patients within the risk set of the case patient were individually matched on additional potential risk factors for intensive monitoring and psychiatric hospitalization: age at discharge (±5 years of case), gender, index hospitalization length of stay (within ±1 day of the number of hospital days if the case group patient's length of stay was fewer than ten days; otherwise, within ±10% of the case group patient's length of stay), and total number of several psychiatric comorbidities (no diagnosis or one or more of the following diagnoses: type II bipolar disorder, other anxiety disorder, personality disorder, any substance use disorder, and posttraumatic stress disorder [PTSD]). When more than two patients satisfied the matching criteria, two patients were randomly selected to match the patient from the case group.
Study measures
Covariates.
Patient covariates included age at index discharge; race; Hispanic ethnicity; diagnoses of a substance use disorder, PTSD, major depression, personality disorder, anxiety disorder and bipolar disorder type II; service connection in regard to disability benefits (indicating disability from conditions occurring or exacerbated during military service); number of Charlson medical comorbidities (
16); prior suicide attempt; use of services with Medicare claims; and numbers of outpatient visits, outpatient mental health visits, VA psychiatric hospitalizations, psychiatric inpatient days, and psychotropic medications filled during the year before the index hospitalization. If the
ICD-9-CM diagnosis codes indicated that the patient was in remission from a substance use disorder, then comorbid substance abuse or dependence was considered not present. Suicide attempts were based on
ICD-9-CM codes E950–E959 and on
ICD-10 codes X60–X84 and Y87.0 (
17). All diagnoses were defined on the basis of data from the 12 months prior to the index discharge, including diagnoses during the index hospitalization. Facility-level variables included region of the facility and whether the facility was in an urban area.
Clinical monitoring.
Monitoring visits were counted during the 84 days (12 weeks) immediately after a discharge from a psychiatric hospitalization because this was considered the period of highest risk for adverse outcomes, including suicide. Total number of visits included in-person visits with a psychiatric Current Procedural Terminology (CPT) code as well as in-person visits or visits by telephone that noted a mental health diagnosis with a nonpsychiatric CPT code. The psychiatric CPT codes included the following: 90801, 90802, 90804–90819, 90821–90824, 90826–90829, 90845, 90847, 90849, 90853, 90857, 90862, 90870, and 90871. On any given day, only one monitoring visit was counted, even if more than one qualifying visit occurred. Monitoring intensity was expressed as a rate of visits per 84 days to standardize the number of visits for those discharged fewer than 84 days before rehospitalization.
Statistical analyses
The primary endpoint was psychiatric rehospitalization at any time after discharge. To measure the association between psychiatric rehospitalization and monitoring, conditional logistic regression models were used. Because the patients in the control group were selected from the risk set of the patients in the case group—in other words, those who were at risk of rehospitalization when the case group patient was rehospitalized—the conditional logistic regression generated the rate ratios to estimate the relative risk (RR) of rehospitalization and associated 95% confidence intervals. The conditional logistic regression model based on risk set is equivalent to the Cox regression model, stratified by matched sets, with time from discharge to rehospitalization as the response variable where control group patients were considered censored shortly after the rehospitalization of the patient in the case group.
The adjusted RR associated with increased monitoring was obtained by including the covariates described above. Continuous covariates were categorized or transformed after we examined their distribution and their functional relationships to the outcome. The secondary endpoint was psychiatric rehospitalization during the first 84 days postdischarge; this was equivalent to an analysis of a subgroup of matched sets where patients from the case group were rehospitalized during the high-risk period.
To assess for differential effects of monitoring in key patient subgroups with a substance use disorder, PTSD, and other anxiety disorders, the model included interactions between rate of monitoring visits and each of these diagnoses. To better illustrate the differential effect of monitoring, the rate of monitoring during the high-risk period was categorized as none, low (≥1 and <2 visits), moderate (≥2 and <6 visits), high (≥6 and <12 visits) and very high (≥12 visits) monitoring. Although the actual visit intervals may not be equidistant, the high level of monitoring roughly corresponded to biweekly to weekly monitoring and very high monitoring corresponded to weekly or more frequent monitoring.
Several other models using different predictors or different parameterizations of the primary predictor were also completed. In one model, the total number of visits (censored at 13 as the maximum) was used as the primary predictor instead of the visit rate. A model was also fit where substance use disorder was coded according to four categories: no substance abuse or dependence, alcohol abuse or dependence only, drug abuse or dependence only, and alcohol and drug abuse or dependence. All analyses were conducted with Stata, version 10.2.
Results
In the cohort of 887,859 patients with depression, 64,925 (7.3%) had at least one psychiatric hospitalization. The case group included 17,856 (2.0%) patients who had at least two psychiatric hospitalizations, and of those with at least two psychiatric hospitalizations, four were not matched with a patient from the control group. Thus there were 17,852 patients in the case group and 35,511 in the control group. Thirty-seven percent (6,672 of 17,852) of case group patients were rehospitalized within 12 weeks (84 days) of the index discharge.
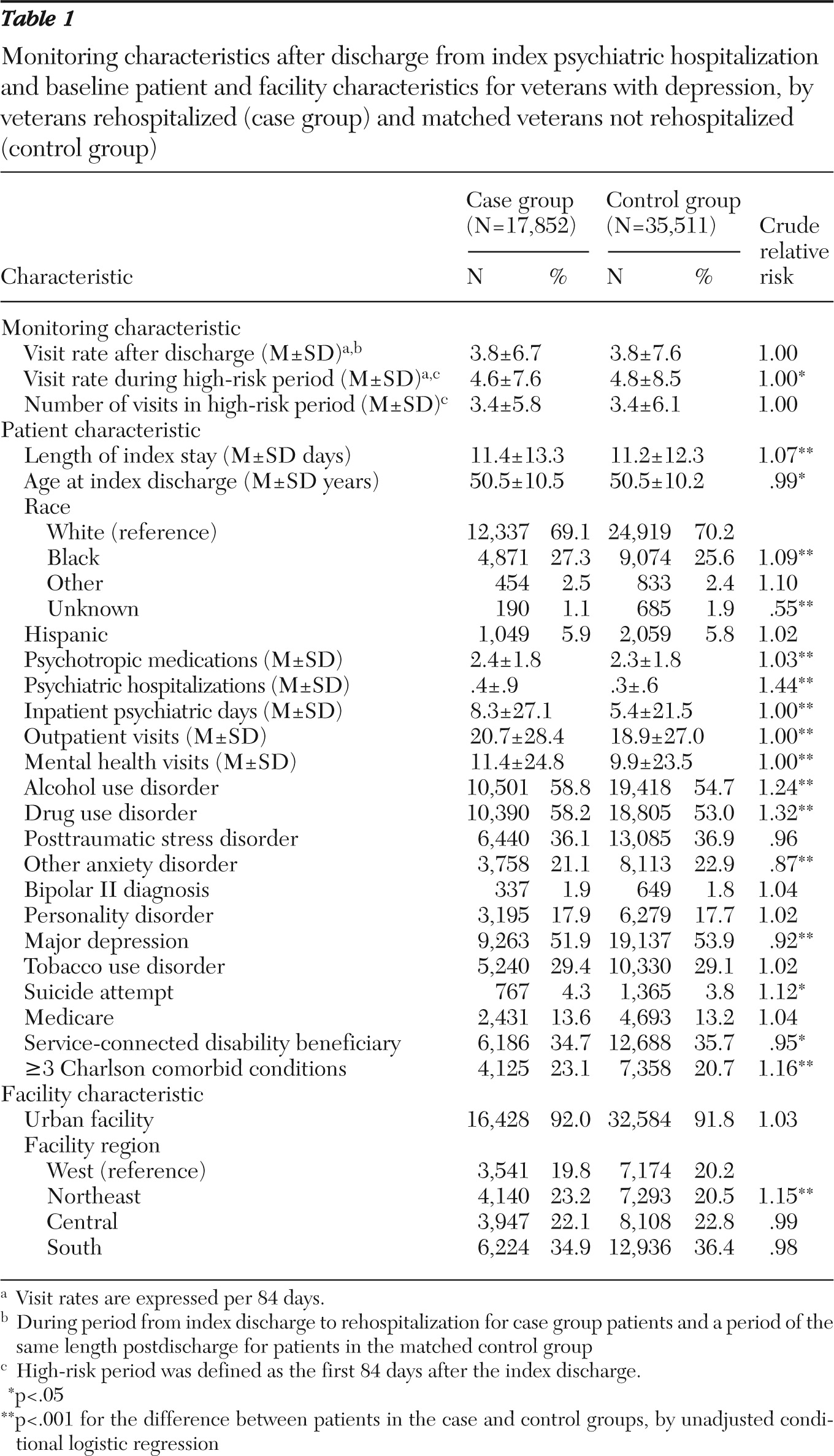
Table 1 shows baseline patient and facility characteristics of the case group and the control group. Despite the matching process, several factors differed significantly between groups, although most differences were not large. Of note, the number of psychiatric hospital days in the year prior to index hospitalization was greater for the case group than for the control group (8.3 versus 5.4), and the number of psychiatric hospitalizations was also greater for the case group than the control group (.4 versus .3).
The mean rate of visits for monitoring during the high-risk period was significantly lower for patients from the case group than for those in the control group (4.6 versus 4.8 visits per 84 days, p=.02). The subgroup of matched sets in which case counterparts were rehospitalized during the high-risk period gave similar results (5.3 for case group patients versus 5.6 per 84 days for control group patients, p=.03; data not shown). The unadjusted relative risk (RR) of rehospitalization associated with monitoring rate during the high-risk period was .997 (p=.02), and the covariate-adjusted risk was not statistically significant (RR=.999, p=.31).
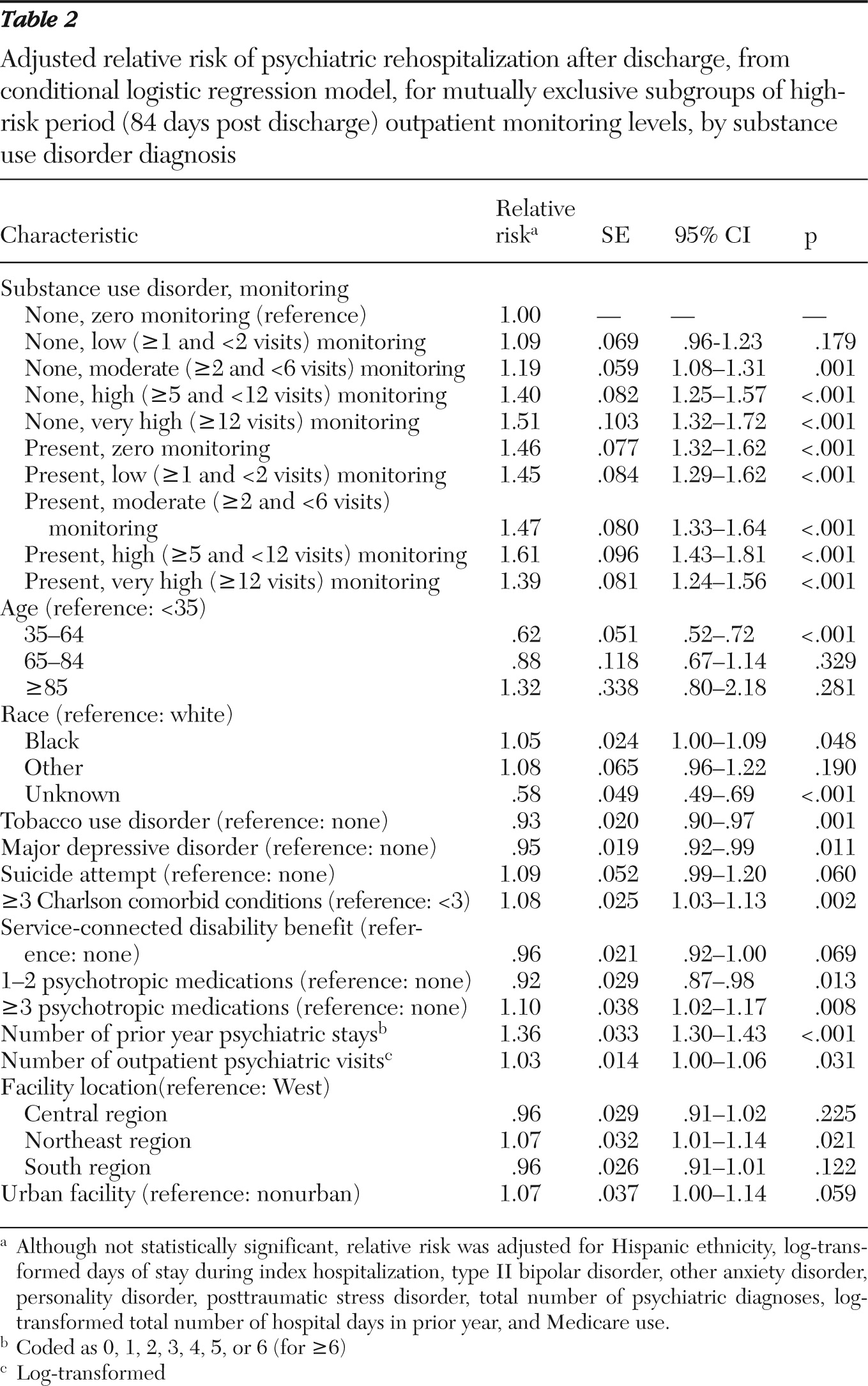
Of the key subgroups, a significant differential relationship between psychiatric rehospitalization and monitoring that depended on comorbid substance use disorder status was found. When monitoring was categorized to five levels, 31.5% (N=16,822) had no monitoring, 14.6% (N=7,769) had a low level of monitoring, 30.2% (N=16,144) moderate, 12.1% (N=6,479) high, and 11.5% (N=6,149) very high monitoring. In the model that included mutually exclusive monitoring levels by substance use disorder status (
Table 2), the adjusted risk of psychiatric rehospitalization of patients without a comorbid substance use disorder was 1.09 with low monitoring, 1.19 with moderate monitoring, 1.40 with high monitoring, and 1.51 with very high monitoring, compared with the referent subgroup of patients without a comorbid substance use disorder and no monitoring. On the other hand, compared with the same referent subgroup, the adjusted RR for those with a comorbid substance use disorder was 1.46, 1.45, 1.47, 1.61, and 1.39 with no, low, moderate, high, and very high monitoring, respectively. Hence, for patients without a comorbid substance use disorder, higher monitoring was associated with rehospitalization, but for those with a comorbid substance use disorder, higher monitoring was not associated with rehospitalization. In fact, those with a comorbid substance use disorder who received very high monitoring (weekly or more frequent visits) had lower risk of rehospitalization than those who received less frequent monitoring.
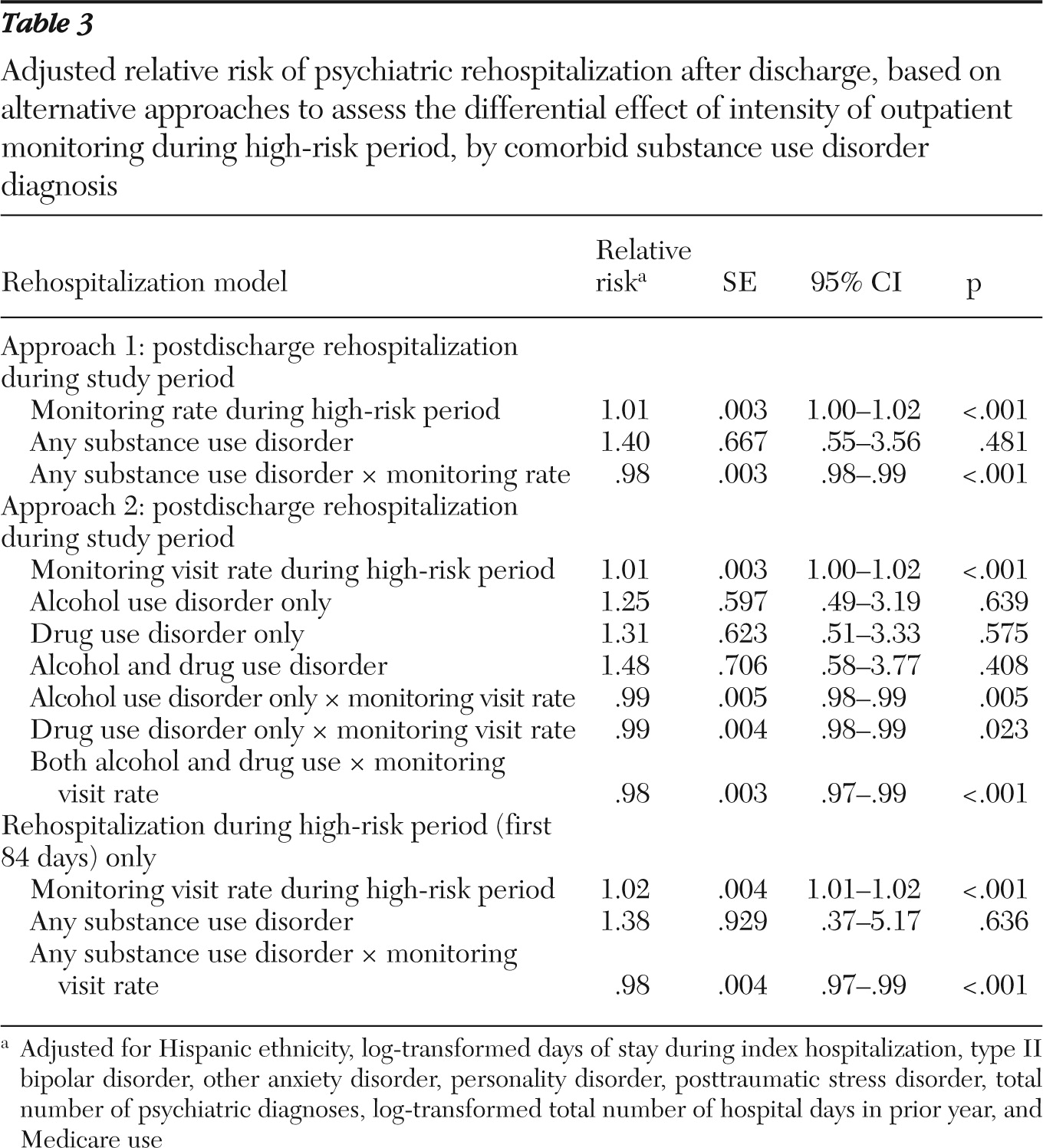
A model that examined the interaction of monitoring rate with substance use disorder status showed a significant negative interaction (p<.001) (
Table 3); rehospitalization was positively associated with increased monitoring of patients without a comorbid substance use disorder, but the risk associated with monitoring decreased significantly for patients with a comorbid substance use disorder. The risk of rehospitalization associated with a weekly visit (12 visits per 84 days) versus no monitoring visit was estimated to be 1.14 for patients without a comorbid substance use disorder, whereas the corresponding risk ratio was reduced to .94 for patients with a comorbid substance use disorder (estimated from the model). Similar results were found with various alternative models, including a model based on only the matched risk sets in which case group patients were rehospitalized during the high-risk period. When substance use disorder was modeled into four categories (no substance use disorder, alcohol use disorder only, drug use disorder only, and both alcohol and drug use disorders), having both alcohol and substance use disorders was more strongly associated with rehospitalization than having either disorder alone, and the interaction of monitoring rate and having both substance use disorders was more negative than the interactions of monitoring rate and either alcohol or drug use disorder.
As shown in
Table 2, persons of middle age (35–64 years) were less likely than younger persons (<35 years) to be rehospitalized, and prior use patterns, such as prior hospitalizations, were associated with rehospitalization. Interestingly, a major depressive disorder diagnosis (versus “other depression diagnosis”) and a tobacco use disorder were negatively associated with rehospitalization. Geographic variation was also seen, with patients in the Northeast region being 7% more likely to be rehospitalized than those in the Western region.
Discussion
This study found that increased outpatient monitoring of patients with depression during the 12-week period immediately after psychiatric hospitalization was not associated with a decreased risk of rehospitalization. However, study findings supported a relationship between increased monitoring and decreased rehospitalization among depressed patients with a comorbid substance use disorder. Among those without a substance use disorder diagnosis, increased monitoring was associated with increased risk of rehospitalization, whereas among those with a substance use disorder increased monitoring was associated with decreased risk of rehospitalization.
The positive relationship between increased monitoring and rehospitalization of patients with depression without substance use comorbidity is likely due to remaining treatment indication biases where, despite matching, patients with more severe depressive symptoms were seen more often and also were more likely to be rehospitalized. On the other hand, despite a potentially similar treatment indication bias among depressed patients with a substance use disorder, this study indicated that among these patients, increased monitoring was no longer associated with increased risk of rehospitalization beyond what might be associated with having a comorbid substance use disorder. Moreover, in this subgroup, weekly or more frequent monitoring compared with less frequent monitoring during the high-risk period was associated with the lowest risk of rehospitalization.
A closer look at the subset of patients rehospitalized within 30 days of discharge and their matched counterparts showed an even bigger contrast among those with a comorbid substance use disorder, where the percentage of rehospitalized patients decreased with increasing monitoring. Specifically, 35.5% were rehospitalized patients among those with no visit, 35.7% of those with one visit, 34.5% with two visits, 32.7% with three or four visits, and 24.4% with five to eight visits, whereas only 22.3% of patients were rehospitalized among those with more than eight visits. This finding is in contrast to the finding with patients with no comorbid substance use disorder, for whom more visits generally were associated with a higher percentage of patients being rehospitalized: 29.2% were rehospitalized among patients with no visit, 30.8% with one visit, 35.6% with two visits, 35.5% with three or four visits, 43.7% with five to eight visits, and 45.5% with more than eight visits.
A previous study assessing the relationship between monitoring during various high-risk periods and suicide risk of patients with depression was not able to establish a definitive relationship between closer monitoring during the high-risk period and reduced suicide risk (
18). Demonstrating such a relationship is difficult due to the low rate of completed suicides. This study instead evaluated whether closer monitoring during the high-risk period would affect rate of rehospitalization after a discharge from a psychiatric hospitalization. Given that rehospitalization is not a rare outcome, sample size was adequate to assess the relationship. Nonetheless, we found no relationship between increased outpatient monitoring during the high-risk period and rehospitalization. Our finding of a differential relationship between rehospitalization and intensity of monitoring between those with and those without a comorbid substance use disorder, however, was seen in various alternative analyses. We also found consistent results among patients with an alcohol use disorder and those with a drug use disorder and a more pronounced association among those with both alcohol and drug use disorders.
These findings are potentially important, given the high levels of substance use comorbidity among patients hospitalized with a depression diagnosis and the fact that comorbid substance use disorder is associated with a substantially higher likelihood of rehospitalization among depressed patients. The result is also consistent with the findings by Ilgen and colleagues (
9), who showed that continuing care for substance use disorder for 30 days postdischarge was associated with a lower risk of early readmission after an index inpatient psychiatric treatment among patients with co-occurring substance use and psychiatric disorders. Our study differs from the Ilgen study in that we focused on a cohort of patients who received depression treatment and we used national VA data from multiple years.
Because of the observational nature of our data, this study does not elucidate the reasons for different monitoring rates among patients with substance use disorder diagnoses. One possible explanation is that some inpatients with a comorbid substance use disorder were discharged prematurely. Although we found patients with comorbid substance use disorders to have shorter length of index hospital stay than those without a comorbid substance use disorder (means of 10.8 days versus 12.2 days, respectively; p<.001), we did not find a difference in the length of index hospital stay between substance use disorder patients who were rehospitalized versus those who were not (10.9 days versus 10.8 days, respectively; p=.68). Increased monitoring may reduce the risk of rehospitalization among depressed patients with substance use disorders because higher levels of monitoring are particularly helpful in assisting with substance-related issues among depressed patients. Such patients may benefit from increased monitoring and from linkage to appropriate addiction treatment services. Alternatively, increased monitoring may be an indicator that a patient is stable enough to take advantage of outpatient care (that is, substance use does not interfere with making visits) or that the patient is motivated to address his or her substance use or mental health needs—both of which may represent resilience and may be associated with decreased risk of rehospitalization.
We did not directly assess the validity of the HEDIS indicators measuring receipt of outpatient mental health follow-up within seven or 30 days of hospital discharge. Patients could have received close outpatient monitoring within the 12-week high-risk period and yet have not met criteria for the HEDIS indicators and vice versa. However, our study suggests that all patients discharged from a psychiatric hospitalization may not benefit equally from close outpatient monitoring and therefore perhaps should not all be subjected to the same indicator. In addition, patients with comorbid depression and substance use disorders may benefit more from closer monitoring within 30 days postdischarge than the one visit required to meet the HEDIS monitor.
The study was limited in that diagnostic information was obtained from clinical encounters and not standardized interviews. Underdetection of substance use disorder among depressed patients is likely, and our study findings are relevant to those whose substance use is salient enough to be noted by the treating provider. Because our patient population was mostly male veterans, and both the index hospitalization and rehospitalization occurred at VA facilities, this may limit applying our findings to non-VA populations. The risks of readmission associated with comorbid mood and substance use disorders, however, are not unique to VA settings. Similar risks have been reported in a predominantly female population of U.S. Medicaid recipients (
19). Other health systems, particularly those treating patients with high rates of comorbid substance use and depression, should consider investigating the relationship between close monitoring and readmission among their patient populations.
Conclusions
Despite the limitations, our study emphasizes the importance of monitoring depressed patients with a comorbid substance use disorder during the 12 weeks immediately after their discharge from a psychiatric hospitalization. Our study suggests that increased monitoring of patients with a substance use disorder during the high-risk postdischarge period may be a rational allocation of resources in the depression treatment population. Efforts to improve participation in outpatient monitoring may be of more benefit to this subgroup. We could not demonstrate that outpatient monitoring after a psychiatric hospitalization had a protective effect (that is, prevented rehospitalization) for patients without a comorbid substance use disorder, potentially because of remaining treatment selection biases. The reasons why increased outpatient monitoring may not be as successful at reducing the risk of rehospitalization of depressed patients without a substance use disorder deserve further study. Future research should incorporate measures of clinical status, ability to access care, motivation for treatment, and whether the readmission was voluntary or involuntary to further our understanding of the relationship between monitoring and rehospitalization and the role of comorbid substance use disorder. Future work should also address whether deliberately increasing monitoring rates for this important subgroup results in improved outcomes.
Acknowledgments and disclosures
The funding sources for this work were grants IIR 04-211-1 and MRP 03-320 from the U.S. Department of Veterans Affairs, Health Services Research and Development Service, and grant R01-MH078698-01 from the National Institute of Mental Health. Resources were also contributed by the Serious Mental Illness Treatment Resource and Evaluation Center, Ann Arbor.
The authors report no competing interests.