Appointments for medication management (
1) are brief and spread out over time (
2–
5). Currently, medication management in outpatient psychiatric practice is usually provided in the context of split treatment, in which a psychiatrist provides pharmacotherapy and a nonpsychiatrist clinician provides psychotherapy (
6–
10).
Medication management is referred to in other studies as “med checks” (
11,
12) or pharmacotherapy (
6). Psychiatrists who provide pharmacotherapy are commonly referred to as psychopharmacologists (
13,
14). Stahl (
15) characterized psychopharmacologists as “psychiatric subspecialists with a high degree of expertise in the diagnosis and treatment of drug-responsive psychiatric disorders.” Kontos and colleagues (
16) described the psychopharmacologist's role in care as specific, narrow, and explicitly “medical” rather than “psychotherapeutic.” That is, they prescribe medications based on symptom assessments.
Though the psychopharmacologist's role is well described, there is concern that the role is insufficient to address patients' psychosocial needs (
17). Other investigators have expressed concern that the pharmacotherapeutic relationship may cause the psychopharmacologist to disengage from exploring issues important to care delivery, such as educating patients about the nature of their illness (
18), negotiating a treatment plan (
19), developing a trusting, caring, and participatory relationship with patients (
18), and bolstering patients' self-management skills (
16).
To acquire a greater understanding and appreciation of what transpires in pharmacotherapy appointments, we performed an exploratory, cross-sectional, observation study that provided a quantitative analysis of psychiatrist-patient communications during split-treatment appointments. We set out to answer several questions. Are interaction analysis systems, that is, observation instruments for quantifying the salient features of physician-patient verbal and nonverbal communications (
18), useful in characterizing the salient features of psychiatrist-patient verbal and nonverbal communications in pharmacotherapy appointments? Are there particular communication patterns that psychiatrists employ in these appointments? If so, which psychiatrist and patient factors are associated with these communication patterns? Last, are psychiatrists flexible in their use of communication patterns to meet patients' needs?
Methods
Study design and population
Visits involving unique psychiatrist-patient dyads, falling between the first and sixth appointments, were audiorecorded at four community-based mental health clinics affiliated with the University of Pittsburgh Health Care System.
Psychiatrists were eligible to participate if they practiced at a participating study clinic. Patients were eligible if they were 18 to 65 years of age; had received a diagnosis of major depressive disorder, depressive disorder, not otherwise specified, or dysthymic disorder as defined by the DSM-IV-TR and it had been recorded in their chart; and were in treatment with a participating psychiatrist.
Psychiatrists were recruited through presentations and individual meetings. Patients were self-referred in response to a flyer or introduced to the study by their therapist or psychiatrist. Recruitment occurred between March 2005 and May 2008. The study was approved by the University of Pittsburgh Institutional Review Board, and all participants gave written informed consent. Patients who completed the study received a $10 gift card. Psychiatrists received no compensation.
Data collection
Before the appointments, research staff collected demographic information about the psychiatrists and the patients, the severity of the patients' depression, and psychiatric diagnoses recorded in the patients' charts. At the start of the appointment, research staff activated the recorder and left the office. Psychiatrists and patients saw the recorder being turned on. The recordings were sent to the Roter Interaction Analysis System (RIAS) communications laboratory at the Johns Hopkins Bloomberg School of Public Health, which prepared a coded analysis of the conversation. The data were merged with all other study data for final analysis.
RIAS is derived from social exchange theories that view the medical encounter as “a meeting between experts” in which dialogue shapes the therapeutic relationship and reflects patients' and providers' roles and obligations (
20–
25). Communications that convey a complete thought are coded as numbers or elements of speech in 41 discrete speech categories. These individual coded elements can be used in the analysis separately or grouped to form larger composites that comprise the broad conceptual communication domains of instrumental and affective behavior (
26).
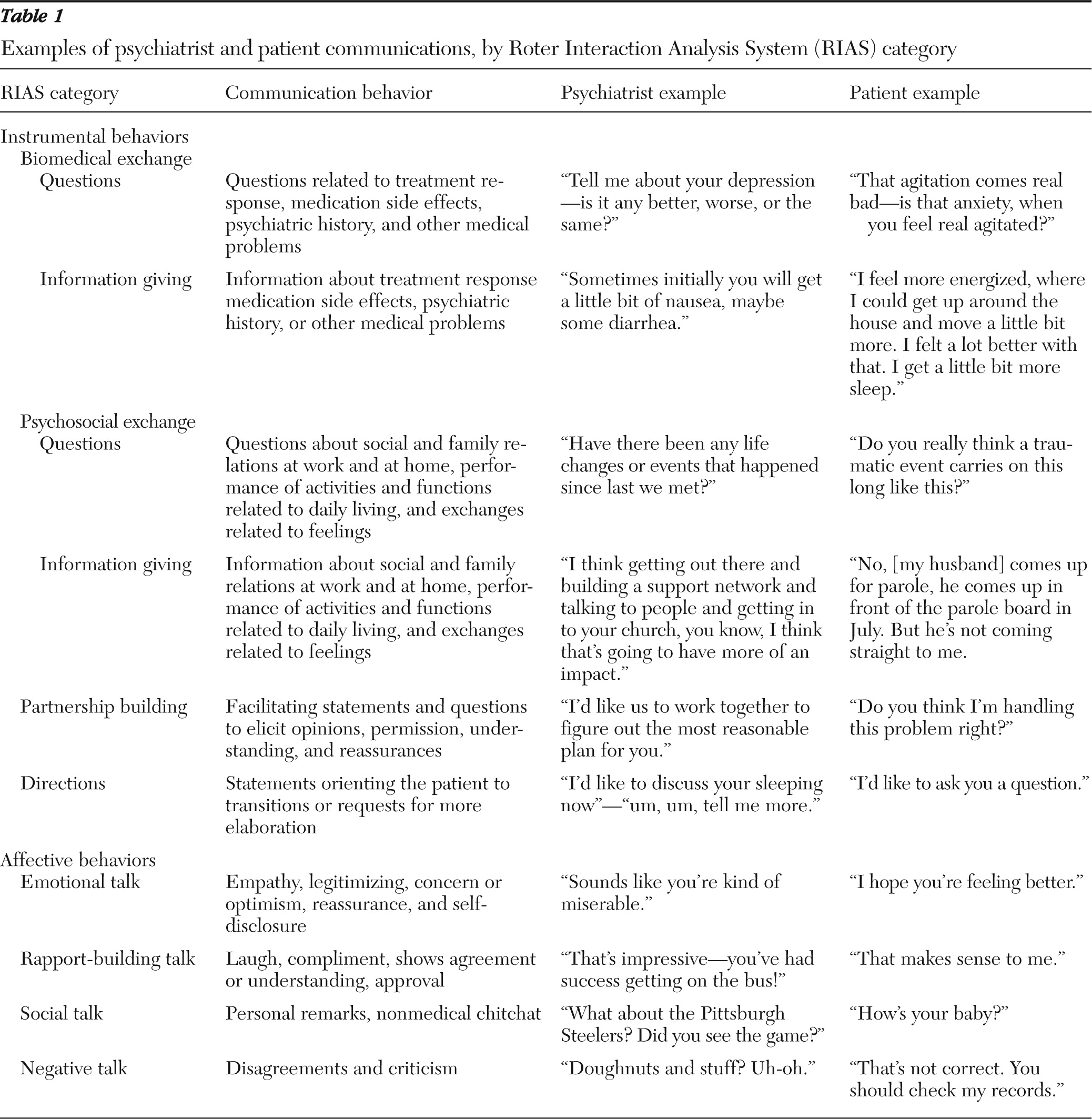
In this analysis, we constructed psychiatrist and patient communication profiles by creating four instrumental-domain and four affective-domain composites for both patients and psychiatrists. The instrumental-domain composites reflected biomedical exchange (RIAS codes for biomedical questions and biomedical information giving about psychiatric history, symptoms, and therapeutic regimen); psychosocial exchange (codes for psychosocial questions, information giving about social and family relations at work and at home and performance of activities and functions related to daily living, and exchanges related to feelings and emotions); partnership building (codes for questions about opinions and beliefs, questions asking for clarification of fact, and questions that check for understanding); and directions (codes for transitions in the conversation and orienting patients to changes in the focus of the dialogue.)
The affective-domain composites reflected emotional talk (RIAS codes for empathy, legitimizing, concern or optimism, reassurance, partnership, and self-disclosure); rapport-building talk (codes for laughter, compliment, showing agreement or understanding, and expressions of approval); social talk (codes for personal remarks); and negative talk (codes for disagreements and criticisms).
RIAS coding reliability averages .85 for both patient and physician categories on the basis of Pearson correlation coefficients (
20). The RIAS has demonstrated predictive validity to physicians' malpractice experience (
27), physician satisfaction (
28), patient satisfaction (
29), patient recall (
30), and improvements in levels of emotional distress (
31) and concurrent validity between RIAS emotional and rapport building statements and total Vanderbilt Therapeutic Alliance scores (
32). Examples of participants' RIAS composite statements can be found in
Table 1.
Because emotions influence an individual's cognition and behavior and nonverbal behaviors often accompany words and offer meaning in context (
25), coders rated the global affect or voice tone of the psychiatrists' and patients' dialogue on a numeric scale—from 1, low or none, to 5, high—in 12 voice tone categories. Global Affect Ratings were recorded for both psychiatrists and patients for anger, anxiety, dominance, interest, friendliness, responsiveness, sympathetic, interactivity, and respectfulness. Also, we rated psychiatrists' expression of being hurried as well as patients' expression of distressed and depressed affects.
To assess the influence of the severity of a patient's illness on patient and provider communications (
33), patients were asked to complete the Patient Health Questionnaire-9 depression module (PHQ-9) (
34), a self-administered instrument in which each of the
DSM-IV depression criteria are rated on a 4-point scale, from 0, not at all, to 3, nearly every day. The total score can range from 0 to 27.
Data analysis
Two coders analyzed the recordings. Interrater reliability was assessed on a random sample of ten double-coded recordings (12%) for each RIAS speech category. Pearson correlation coefficients for high-frequency categories (categories containing more than two statements per visit) of psychiatrist talk ranged from .85 to .97 and of patient talk ranged from .67 to .99. Lower reliability was found for low frequency categories of criticism and disapproval (.36) and psychiatrists' (.4) and patients' (.1) orienting or transition statements. Coder agreement for both psychiatrists' and patients' voice tone ratings within 1 point on the Global Affect Rating scales ranged from 80% to 100%.
For statistical analyses we used SPSS software, version 17.0. Descriptive statistics, including measures of central tendency (such as means and medians) and dispersion (such as standard deviations and ranges), were computed for continuous data. Frequency distributions were used for categorical data.
To identify psychiatrists' communication patterns, we performed a two-step cluster analysis by using a log-likelihood distance measure designed for both continuous and categorical variables. Because cluster analyses limit the number of entered variables, we entered five RIAS composites representing psychiatrists' instrumental behaviors (biomedical and psychosocial questions, biomedical and psychosocial information giving, and partnership building), two representing patients' instrumental behaviors (biomedical and psychosocial information giving), and one representing patients' affective behavior (emotional talk) to reflect the reciprocal nature and principal elements of communication exchanges that occur during pharmacotherapy appointments.
To adjust for variation in appointment length, RIAS composites were transformed into proportions of total participant talk before entering them into the cluster analysis. Then the log-likelihood cluster analysis transformed the RIAS proportions of talk into standardized scores. To identify the possible influence of appointment length on cluster membership, we conducted t tests on the final cluster analysis. Thereafter, t test and chi square analyses were used to identify psychiatrist and patient RIAS composites and demographic variables associated with cluster membership. Bonferroni correction was employed for multiple comparisons of RIAS voice tone ratings.
Results
Site recruitment
Two sites other than the research clinic provided the majority of recordings (77%). One site provided services to white (70%) and African-American (30%) patients and was staffed with attending and resident psychiatrists. The other site provided services largely to African-American patients (95%); the other patients were white (5%). It was staffed by resident psychiatrists under the supervision of an attending psychiatrist. The psychiatrists' role in care was limited to pharmacotherapy in a split-treatment model. Master's-level clinicians provided psychotherapy at all sites.
Psychiatrist and patient recruitment
We approached 52 psychiatrists to invite them to participate; 41 (79%) consented, and 24 (46%) were recorded. Discomfort about being recorded was the primary reason for participation refusal. We approached 150 patients to invite them to participate; 130 (86%) gave signed consent, and 91 (70%) were recorded. Failure to keep the scheduled appointment was the primary reason that consenting patients were not recorded.
Six recordings were inaudible, and one recording was excluded from the analyses because the patient did not meet diagnostic criteria. Final analyses were conducted on 84 recordings, which represented 65% of the patients who consented to participate. The mean±SD number of recordings per psychiatrist was 3.0±2.2.
Demographic information
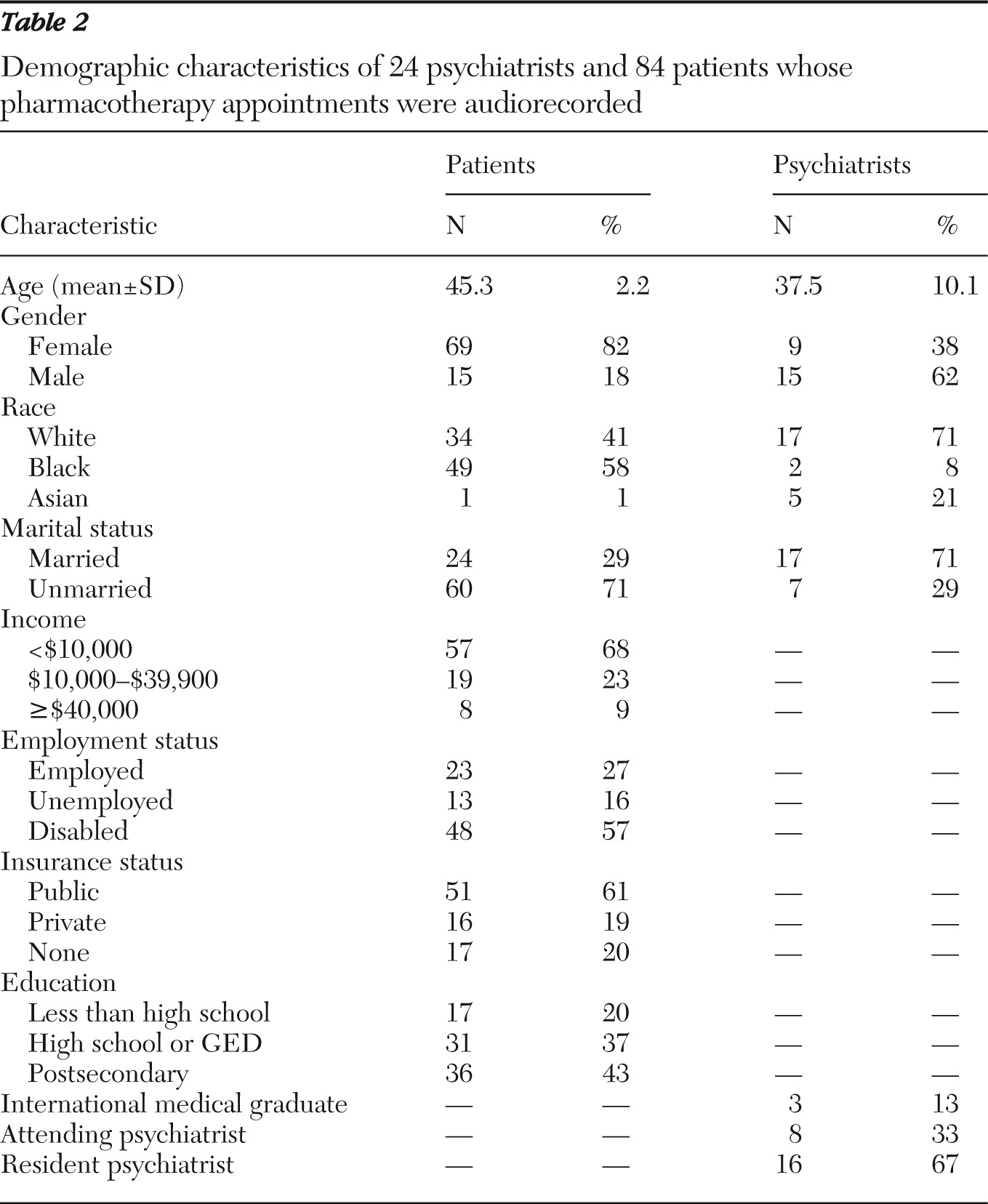
Psychiatrists were predominantly male (62%), white (71%), married (71%), and under 40 years of age (mean 37.5±10.1); 67% were residents (
Table 2).
The patients' mean age was 45.3±2.2 years, and a majority were African American (58%), female (82%), unmarried (71%), and insured through public programs (61%). The mean PHQ-9 score was 13.0±7.1.
The majority of patients were diagnosed as having major depressive disorder (62%), and 38% were diagnosed as having dysthymic disorder or depressive disorder, not otherwise specified. Co-occurring mental disorders included substance abuse or dependence (35%), posttraumatic stress disorder (13%), personality disorders (8%), anxiety disorders (20%), psychotic disorders (8%), and other disorders (8%).
Appointment length and speech dominance
The mean length of recorded appointments was 22.4+12.0 minutes. For speech dominance, a direct measure of psychiatrists' and patients' contribution to the conversation (
28), the overall ratio of psychiatrist to patient talk was 1:1.
Psychiatrist communication profiles and voice tones
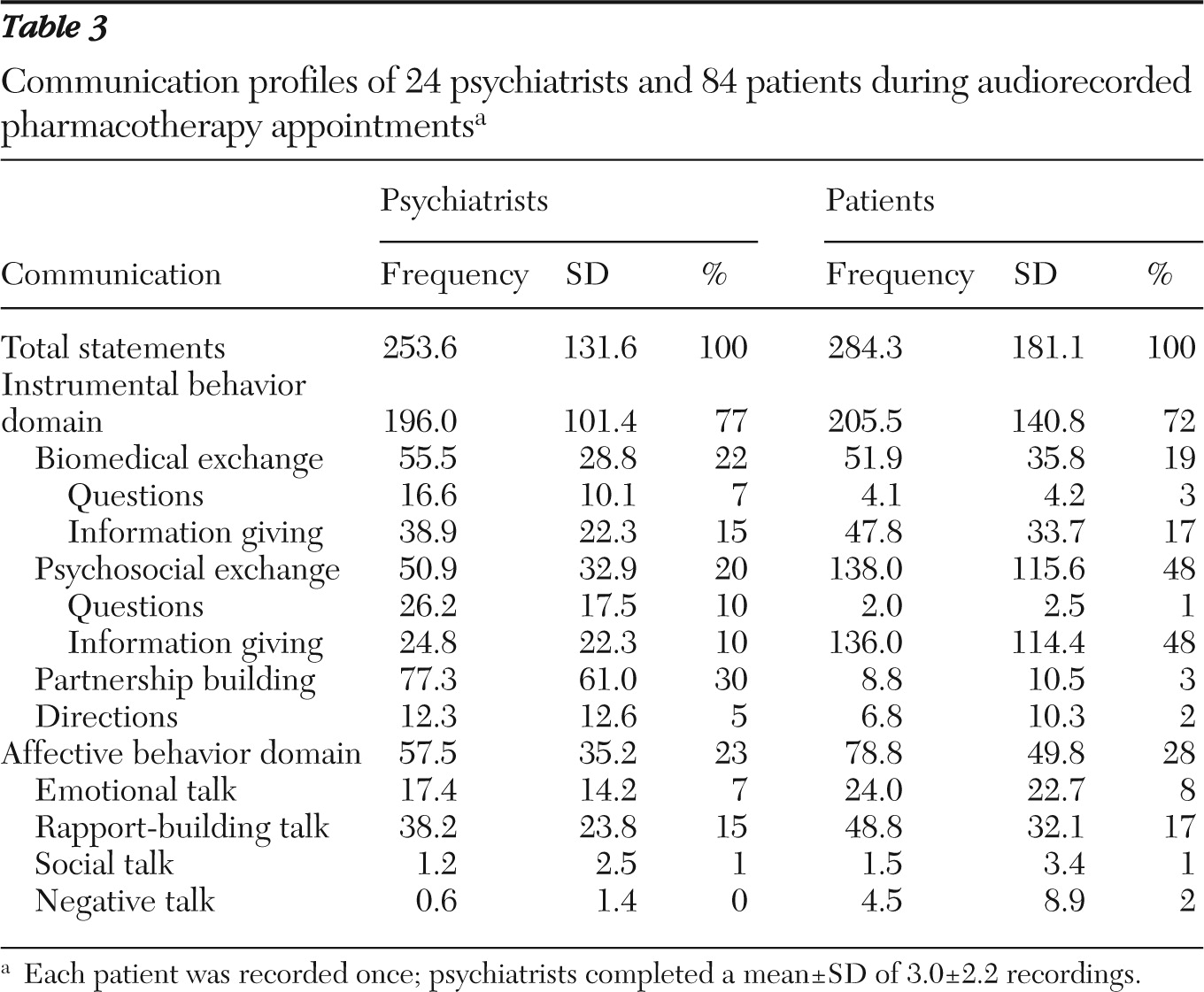
On average, instrumental behaviors accounted for 77% of psychiatrist talk; 42% of psychiatrist talk was devoted to biomedical (22%) and psychosocial (20%) exchanges, and 30% was devoted to partnership building. Affective behaviors contributed 23% of psychiatrist talk; 15% involved rapport building, and 7% was devoted to emotional talk (
Table 3).
Voice tone analyses revealed mean ratings of 4.06±.65 for dominance, 4.23±.77 for interest, 3.64±.79 for friendliness, 3.76±.81 for sympathy, 4.37±.67 for responsiveness, 4.27±.70 for interactivity, and 3.2.±4.9 for respectfulness. Mean voice tone ratings for hurried (2.2±1.16), anxious (1.1±.33), and anger (1.05±.21) were low.
Patient talk and voice tones
On average, the majority (72%) of patient talk was devoted to instrumental behaviors; 19% involved biomedical exchanges, and 48% involved psychosocial or lifestyle information giving (
Table 3). Affective behaviors contributed 28% of patient talk; 17% was devoted to rapport building and 8% to emotional talk.
Voice tone analyses revealed mean ratings of 3.52±.75 for dominance, 3.52±.78 for friendliness, 4.13±.83 for responsiveness, 4.12±.83 for interactivity, 2.95±.26 for sympathy, 3.97±.81 for interest, and 3.08±.54 for respect. Mean voice tone ratings for anger (1.61±1.1), anxiety (1.85±1.23), distress (1.69±1.27), and depressed (1.82±1.29) were low.
Cluster analysis
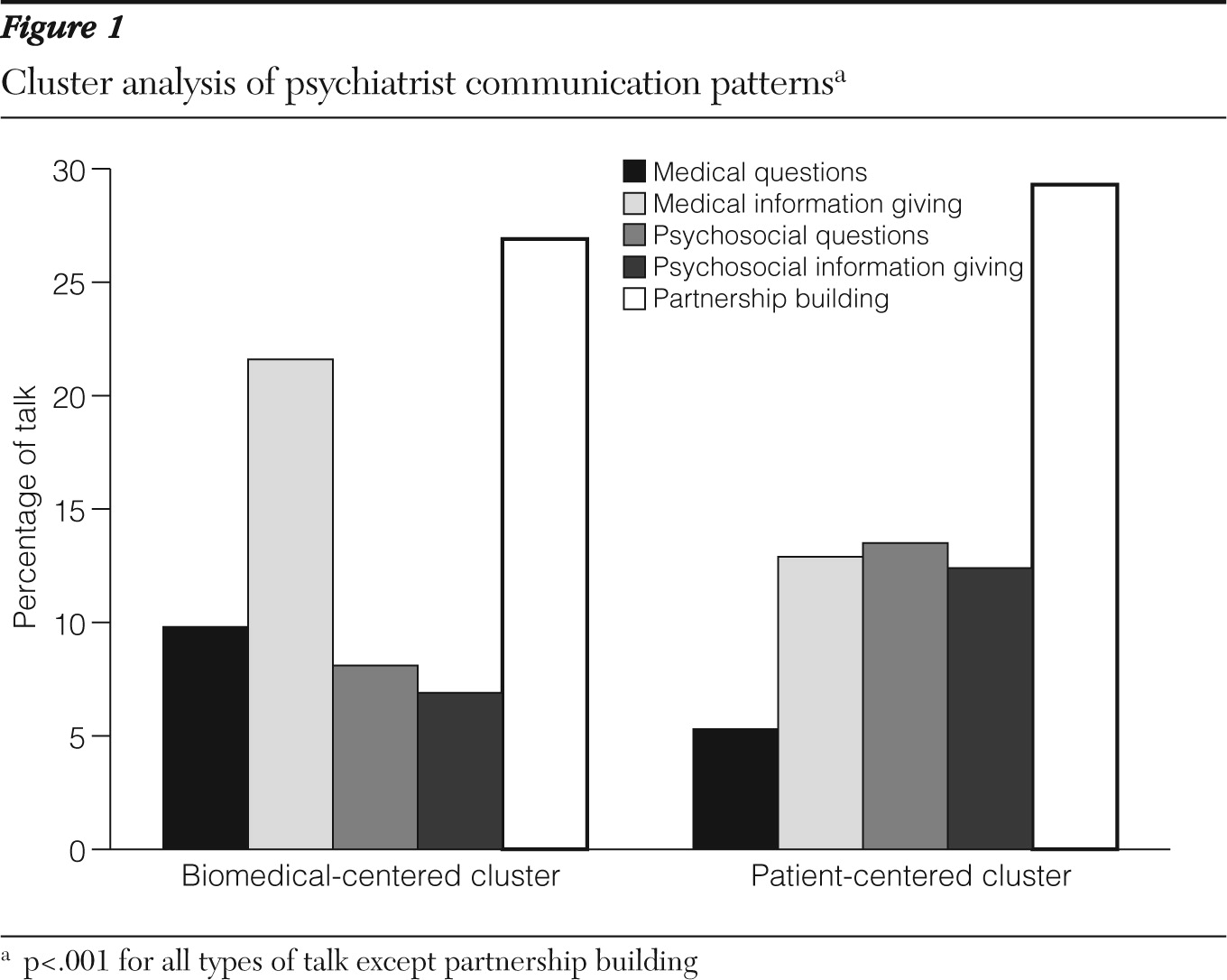
This analysis yielded a two-cluster solution with 42 recordings per cluster (
Figure 1). We named the clusters “biomedical centered” and “patient centered” to convey the distinguishing characteristics of each pattern. Sixteen psychiatrists contributed biomedical-centered recordings, and 18 psychiatrists contributed patient-centered recordings.
The biomedical-centered cluster was characterized by an emphasis on psychiatrist medical questions (η2=.22, df=82, p<.001) and information giving (η2=.20, df=82, p<.001). The patient-centered cluster was characterized by an emphasis on psychiatrist psychosocial questions (η2=.24, df=82, p<.001) and information giving (η2=.17, df=82, p<.001). Compared with the biomedical-centered cluster, the patient-centered cluster was significantly associated with patient verbal dominance (t=2.41, df=82, p=.018), and negative voice tones of anger, anxiety, distressed, and depressed (t=3.22, df=82, p=.002).
There were no significant differences between the biomedical- and patient-centered clusters in partnership-building talk (26.9% versus 29.3%, respectively, of total talk), appointment length (20.2 versus 24.5 minutes, respectively); psychiatrists' and patients' gender or race; psychiatrists' age or status as an international medical graduate; and patients' age, education, marital status, insurance type, total PHQ-9 score, or diagnoses.
Recordings by ten of the 23 psychiatrists were represented in both clusters. T test analyses revealed having recordings classified in two clusters was significantly and positively associated with mean recordings per psychiatrist (t=−2.43, df=21, p=.024), psychiatrists' age (t=−3.24, df=82, p=.002), and status as an attending psychiatrist (χ2=4.23, df=1, p=.04). No significant differences in cluster categorization were found with respect to psychiatrists' race, gender, status as an international medical graduate, marital status, or income.
Discussion
The psychiatrist communication profiles revealed an emphasis on promoting patient participation in treatment decisions by engaging in equitable communicative exchanges and devoting a substantial portion of their talk to partnership building, both essential elements of a working relationship (
25,
28,
35,
36). However, this finding alone is not enough to establish that effective partnering talk occurred, especially because the patient profile failed to show higher levels of biomedical question asking, psychosocial question asking, and partnering statements that would be expected in a partnership. Poor patient response to psychiatrists' partnership building statements could be attributable to patient-related factors such as depression severe enough to impair responsiveness to activating communications, psychological barriers to treatment adherence, such as stigma, denial, and shame (
37), and racial and ethnic differences between the psychiatrist and the patient.
Additionally, participating psychiatrists exhibited high levels of relationship-building talk, for example, emotional and rapport-building statements. Relationship-building talk has been shown to be positively and significantly associated with therapeutic alliance scores (
32), a process measure that is associated with pharmacotherapy treatment response among depressed patients (
38,
39).
We compared our profile findings to two RIAS studies of primary care providers in the United States. The first study was a comparison of RIAS profiles between U.S and Dutch primary care providers whose patients were hypertensive (
40). The second was a pooled analysis of 12 RIAS studies of U.S. primary care providers who were seeing patients with several different diagnoses (
25). The psychiatrists in this study devoted more talk to partnership building (30% versus 2%) and less to rapport building (7% versus 19%) and social talk (10% versus 0%) compared with the American primary care providers included in the Dutch study. They also devoted more talk to partnership and less talk to rapport building and social talk than did the primary care providers in the pooled analysis (11%, 15%, and 6%, respectively). Although we recognize the limitations of these comparisons, our findings are suggestive of differences in communication profiles between the two medical professions.
Our cluster analyses found that psychiatrists employed two communication patterns: a biomedical-centered pattern that emphasized assessment of treatment response, medication adjustments, and education and counseling and a patient-centered pattern that focused on understanding patients' social and familial world and offering recommendations to resolve problems. Consistent with our psychiatrist communication profile, we found high levels of partnership statements in each cluster. Findings of high levels of partnership statements are not unique to patient-centered communications (
41,
42), but they have not been found in biomedical-centered communications of other medical specialties (
26).
We also found that older and attending psychiatrists were more flexible in their use of these communication patterns than their younger counterparts and residents. One possible explanation for these findings could be that greater life or professional experience enhances a psychiatrist's ability to recognize and appropriately respond to a patient's emotional state. Having this ability might allow psychiatrists to shift between communication patterns when necessary to meet a patient's immediate emotional needs. However, because being represented in both communication patterns was associated with the number of recordings per psychiatrist, this proposition requires further study.
From an ethical perspective, the high levels of partnership-building statements by psychiatrists in each communication pattern suggested that their communications were consistent with medical ethicists' pleas to enhance patients' autonomy (
43–
48) and exercise of free will (
47). They appeared to be consistent as well with professional standards of care (
49,
50), including section A,1a, of the American Psychiatric Association practice guidelines for major depressive disorder (
51). However, we cannot say whether their communication efforts were sufficient to aid patients in making informed treatment decisions (
52) or to provide adequate emotional support and listen appropriately to patients presenting with significant emotional distress. Future studies should address these issues.
This study had limitations. First, a potential limitation common to all communications research is observation bias. The presence of a recorder during appointments alters the context of care and may affect how providers and patients communicate. However, several research studies of patient-provider communication have shown that videotaping of clinical encounters, a more intrusive technique than audiorecording, had no effect on physician and patient behavior (
53–
55). Therefore, this bias may have had limited impact on psychiatrist-patient communication behaviors reported by this study.
Second, the inclusion of psychiatric residents in our sample may have limited the utility of our findings for characterizing psychiatrist-patient communications in real-world settings. Third, the lack of more precise diagnostic assessment measures may have limited the effect sizes of our cluster analysis findings. Fourth, our findings were skewed toward psychiatrists with more recordings because we did not standardize the number of recordings per psychiatrist. Fifth, our communication findings may relate only to psychiatrists' communications with depressed patients who resemble the study population—predominantly African American and female.
Sixth, the communication profiles and patterns found in this study may not reflect psychiatrist-patient communications that took place in later appointments. How variation in communication behaviors over the course of a treatment relationship influences treatment outcomes is an important future research topic. Last, our findings may not be reflective of communication profiles and patterns in pharmacotherapy appointments alone. Future studies assessing differences between psychiatrist communications during pharmacotherapy appointments in the context of different types of care, such as consult-liaison, forensic services, and assertive community treatment services, could prove useful in isolating the core communication elements that should be emphasized during continuing education and psychiatric residency training.