The Federal Mental Health Parity Act of 2008 requires employers providing insurance benefits for mental or substance use disorders to provide “parity” between those benefits and benefits for medical and surgical care. The law prohibits more restrictive financial requirements for mental or substance use disorder benefits (including any out-of-pocket expenses) and prohibits more restrictive limits (including limits on number of visits, days of coverage, scope of coverage, and annual or lifetime dollars spent on treatment). Relative to the Federal Mental Health Parity Act enacted in 1996, the act of 2008 strengthened federal parity mandates in several important respects. The recent parity act applies broadly to financial requirements and limits of health benefit design, whereas the 1996 act applied only to annual and lifetime dollar spending limits. The recent act extends to self-insured employers, who were excluded from the 1996 act. And the 2008 act includes requirements of parity for substance use disorder benefits, whereas the earlier act extended only to benefits for persons with mental disorders. As with the 1996 act, small businesses with 50 or fewer employees are exempt from the requirements of the 2008 act. Moreover, plans demonstrating that compliance with the act increases their claims by at least 2% in the first year (1% in subsequent years) may request exemption from this act.
Opposition to parity legislation has focused on fears of rising health care costs. Research examining the effects of parity legislation on utilization and costs of mental health care has generally shown that fears of rising costs are not supported (
1–
5). The results from these evaluations of mental health parity mandates were initially surprising in light of evidence from the RAND Health Insurance Experiment, conducted in the 1970s, which showed increases in mental health care utilization when out-of-pocket costs to beneficiaries are reduced (
6). The absence of rising costs under parity is most readily explained by the extensive use of managed care organizations (MCOs) in current employer-based health insurance. These MCOs administer behavioral health benefits and contain costs by managing the delivery of care—for example, through negotiated reduction in fees with a network of preferred providers and review of appropriateness of services to eliminate unnecessary use. Managed care, however, also raises questions about whether these approaches to cost containment reduce access to or quality of care.
Although research evaluating effects of mental health parity mandates has undoubtedly helped to pave the way for passage of comprehensive federal legislation on parity in 2008, little research has been conducted on the effects of parity mandates for substance abuse treatment benefits (
7,
8). In 1999, under a presidential order, the Federal Employees Health Benefits (FEHB) program, covering 8.5 million enrollees, offered comprehensive parity for both mental disorders and substance use disorders, beginning January 1, 2001. An evaluation of parity implementation in seven large FEHB health plans showed few effects on utilization of mental health and substance abuse treatment services or on spending for these services, but reductions in beneficiary out-of-pocket spending were found in five of the seven plans (
9). Separate analyses of parity in the FEHB program found modest improvements in quality of care for depression, but these results were consistent with secular changes and were likely independent of parity (
10). Prior studies of parity implementation in the FEHB program have not examined parity's impact on utilization, spending, or quality of substance abuse services, independent of those for other mental disorders.
This article reports on further analyses evaluating the implementation of parity in the FEHB program. Using claims data, we examined the impact of parity on use and costs of substance abuse treatment and on indicators of quality of care of substance abuse treatment.
Methods
Study setting
In June 1999, when President Clinton ordered the Office of Management and Budget to implement parity in the FEHB program, he also mandated an evaluation to guide federal policy. Our analysis used data from that evaluation to examine the impact of FEHB program parity on use of substance abuse services, total spending, individual health out-of-pocket spending, and plan spending on those services. We also examined three indicators of quality of care for substance use disorders: identification of adults with a substance use disorder, initiation of substance abuse treatment, and engagement in substance abuse treatment.
In the initial evaluation, nine large FEHB plans were selected for study participation on the basis of location, type of plan (preferred provider organization [PPO] or health maintenance organization [HMO]), population size, and interest in participation. We restricted our analysis to six PPO plans. The two HMO plans were excluded because they were close to parity before the order was implemented. Further, one PPO plan was excluded because analytic resources were not sufficient to accommodate differences in the structure of the claims data. For the six PPO FEHB plans, we estimated differences in substance abuse treatment spending, utilization, and treatment quality indicators two years before and two years after parity implementation (1999–2000 and 2001–2002).
To control for secular trends, we conducted the same analysis using a matched set of health plans without parity coverage or changes in mental and substance abuse treatment coverage from the MarketScan database. These plans were operated by large, self-insured Fortune 200 employers and were matched on the basis of location with the pooled sample of FEHB plans. Enrollees between the ages of 18 and 64 were included in the study. We restricted the analysis to individuals continuously enrolled in a plan for all four years of the study in order to control for population changes and selection effects and to provide an estimate of the effect at the beneficiary level.
The FEHB plans in total covered 364,816 beneficiaries (ranging from 21,374 to 107,875); all had the same benefit limits before parity (maximum of one 28-day inpatient substance abuse treatment per lifetime and 25 outpatient visits per year, 40% inpatient cost sharing, and $25 copayment for outpatient visits). Four of the FEHB plans carved out mental health and substance abuse benefits to managed behavioral health care organizations before implementation of parity, one implemented a carve-out arrangement concurrent with parity, and the remaining plan did not contract with a managed behavioral health care organization during the study period. The MarketScan plans had in total 47,758 beneficiaries. They had limits on both inpatient and outpatient substance abuse services (30 inpatient days and 30 outpatient visits per year) and variable cost sharing for the patients (range 0%–20% for inpatient services and 0%–50% for outpatient services). Between one-third and one-half of the MarketScan plans carved out mental health and substance abuse services during the period considered.
Data
For both the FEHB plans and the MarketScan plans, we examined four years of data on the benefit design, enrollment, and medical claims for two years before and two years after the implementation of parity for the FEHB program. We matched the two populations on the basis of enrollee demographic location as categorized by census regions, demographic characteristics (age and gender), and relationship to the policy holder. We sampled 45,000 people from the FEHB plans and the same number from MarketScan in proportion to the total number of beneficiaries in each state (for the FEHB plans) and in each region (for the MarketScan plans). The study received institutional review board approval.
Identifying substance abuse services
Using diagnosis codes, procedure codes, and provider type codes, we identified the inpatient and outpatient services associated with substance abuse services (a detailed description is available at
www.aspe.hhs.gov). Substance use disorders were defined as claims having
ICD-9-CM diagnosis codes 291, 292, 303, 304, and 305. Inpatient substance abuse services were identified if the last primary diagnosis and a majority of all primary diagnoses associated with an inpatient episode were for substance abuse. Outpatient substance abuse services were identified if any of the following were indicated: a substance abuse primary diagnosis, a procedure specific to substance abuse, or a face-to-face encounter with a provider or treatment at a facility that specialized in substance abuse care.
Statistical analysis
We estimated the association of parity with substance abuse treatment using a difference-in-difference approach. We calculated the average difference (before and after the implementation of FEHB) of the outcomes of interest in the comparison group subtracted from the average difference before and after the implementation of parity in the FEHB plans. With this approach we adjusted for any secular trend in the outcomes that was not associated with the implementation of parity. We used a two-part model to estimate spending associated with parity implementation. The first part used logistic regression to estimate the effect of parity on the probability that a person would use any substance abuse services. The unit of analysis was the person-year, and we adjusted for the demographic characteristics of the person (age and gender) and the person's relationship with the policy holder (employee or dependent). The predictors of interest were an indicator of the post- (versus pre-) parity period, an indicator for the FEHB plan (versus a comparison plan), and the interaction between the two indicators. Because we had four repeated measures per beneficiary, we used a generalized estimating equation approach to correct standard errors of regression coefficients for clustering. Moreover, because the logistic model was not linear, we calculated the average effect of parity on the probability of use with the predictions from 500 bootstrap samples, constructing 95% confidence intervals (CIs) (
11,
12). We used the SAS statistical package, version 9.1. Confidence intervals that exclude 0 indicate statistically significant results.
For the second part of the spending models, we assessed the effect of parity on both total substance abuse service spending and out-of-pocket spending among those who used any substance abuse services. Because out-of-pocket and plan spending are part of total spending, they were correlated with total spending. As in the substance abuse treatment utilization model, we had repeated measures (up to four per beneficiary, because each year an individual could have had positive or zero spending) and unbalanced data (for example, if there was no use of services, the dollar amount was not defined). Hence, we used the “seemingly unrelated regression” approach (in the Stata package), which clustered for beneficiary and year and permitted two correlated outcomes per beneficiary (total spending with out-of-pocket costs). For the conditional regressions in this second part of the analysis, we considered the entire sample of users and the unit of observation was the person-year. We used a normal model to characterize spending and the same predictor variables as in the first part, as well as indicator variables for the diagnosis for which the user received treatment. The coefficient of the interaction between the postparity indicator and the FEHB plan indicator allowed us to estimate any change in substance abuse treatment spending due to the parity policy, after accounting for the secular trend in such spending among users of substance abuse services.
To examine changes in quality of substance abuse services, we used the Washington Circle performance measures, which have been adopted by the National Committee for Quality Assurance for its Healthcare Effectiveness Data and Information Set that tracks indicators of quality of care in health plans (
13,
14). These measures of performance in delivery of substance abuse services can be reported by health plans by using claims or encounter data and are intended to capture different stages of the continuum of care for substance use disorders. The three measures represent a floor of services that are necessary to provide sufficient treatment for enrollees with substance abuse problems, and they address the entire process of care, rather than just one aspect of it.
The first measure, identification of substance abuse services, was the proportion of adult enrollees who, over the measurement year, received any substance abuse treatment, defined as having at least one claim containing a diagnosis of substance abuse or dependence or a substance abuse treatment service. Because substance abuse is typically not detected and diagnosed among those with active disorders, increased rates of identification represent improved quality of care. The second measure, initiation of treatment, was the proportion of adults with a new diagnosis of substance abuse or dependence who over the measurement year had either an inpatient substance abuse treatment admission or an initial outpatient treatment service for substance abuse and any additional services within 14 days. A new diagnosis was defined as a diagnosis with no substance abuse-related claim in the previous 60 days. The third measure, engagement in treatment, was the proportion of adults with a new substance abuse or dependence diagnosis who over the measurement year received at least two additional substance abuse treatment services within 30 days after initiating treatment. This definition of engagement has been associated with improved substance abuse and criminal outcomes (
15,
16).
To examine effects of parity on these performance measures, we used logistic regression models for predicting the probability of identification, initiation, and engagement, and we used the same set of independent variables as used in the first part of the spending models. As with prior models, we calculated the change in the quality measures attributable to parity as the average of 500 bootstrap samples and associated 95% CIs.
Results
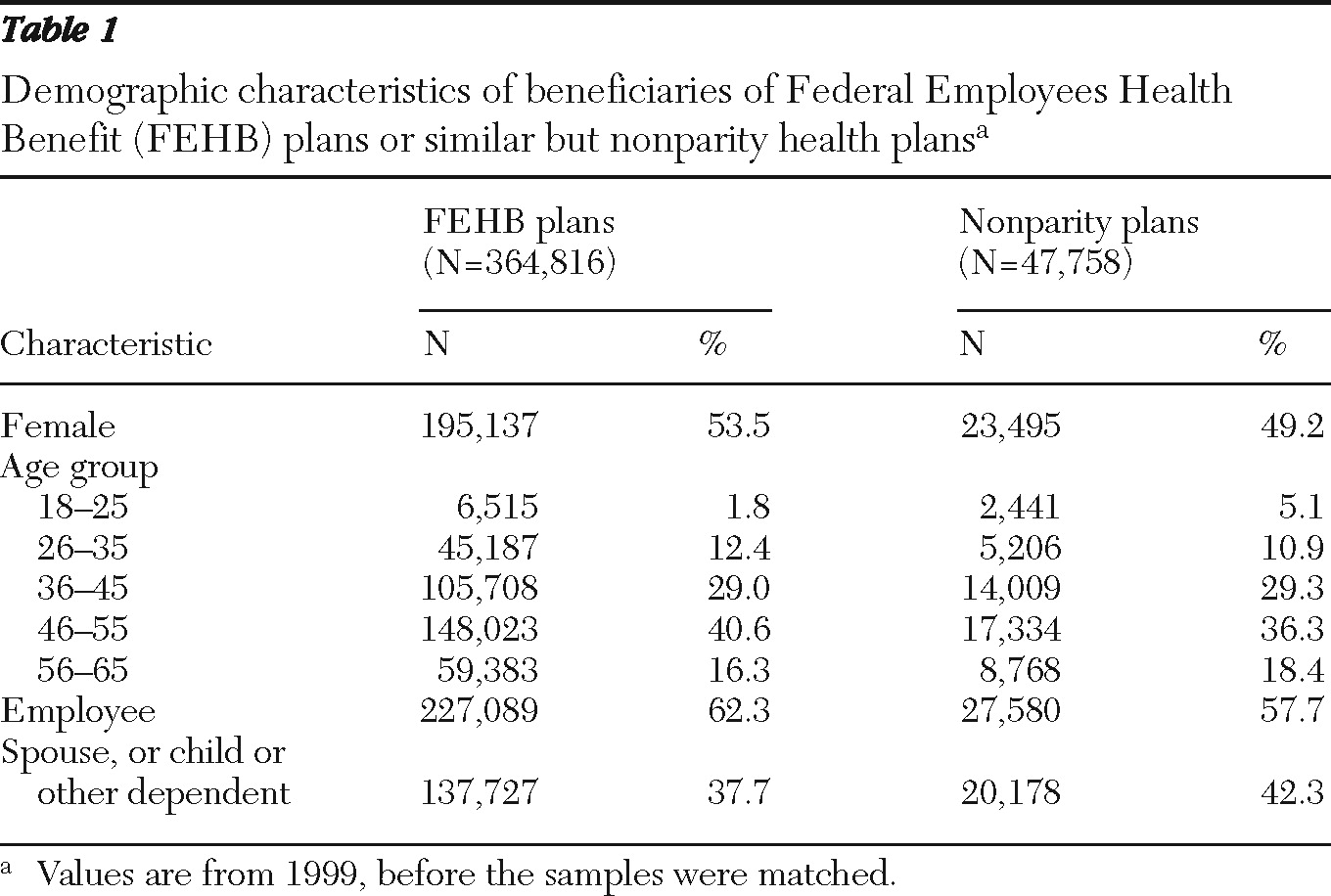
Table 1 reports descriptive data on the samples. In both populations, female beneficiaries accounted for about half of the sample, and employees' spouses accounted for about one-third. There were more dependents in the MarketScan sample, whereas the FEHB population was slightly older.
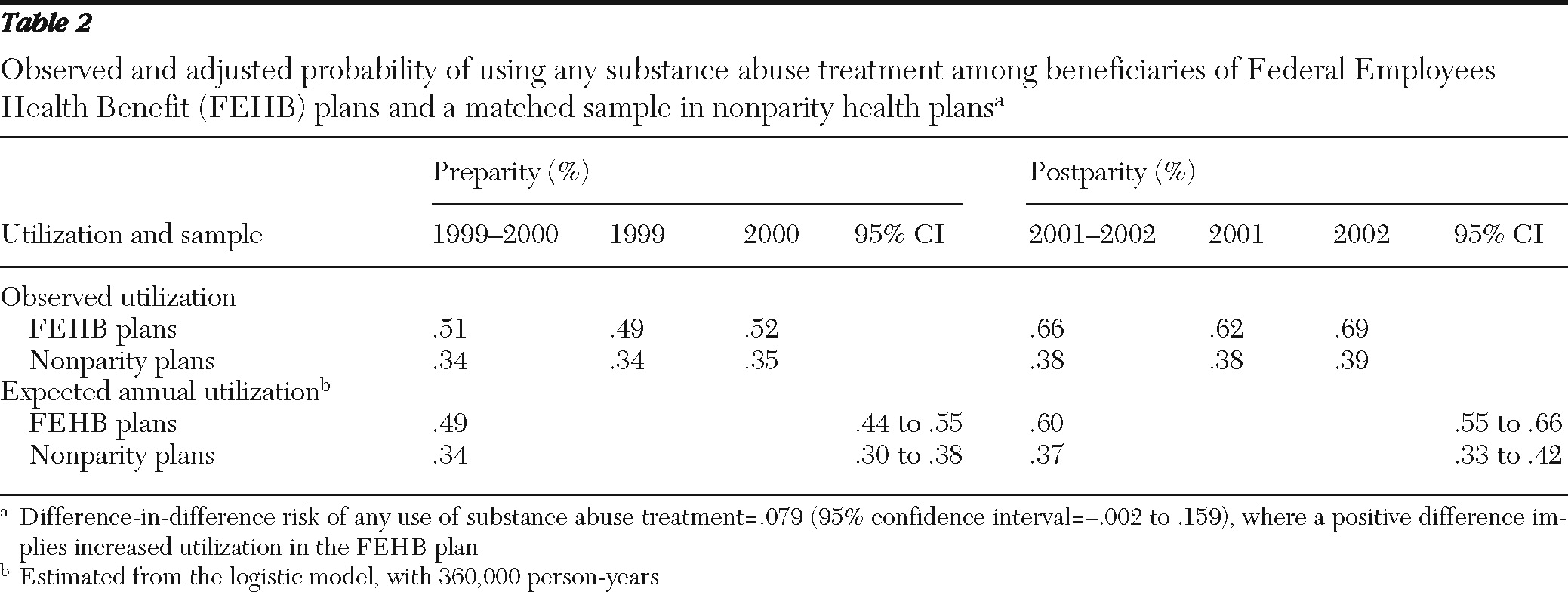
Table 2 presents the actual probability of any use of substance abuse services and difference-in-difference estimates. Any substance abuse treatment use increased over time for all plans; however, after accounting for secular trends, we found no statistically significant difference in the rates of increase between FEHB and non-FEHB plans at the .05 level.
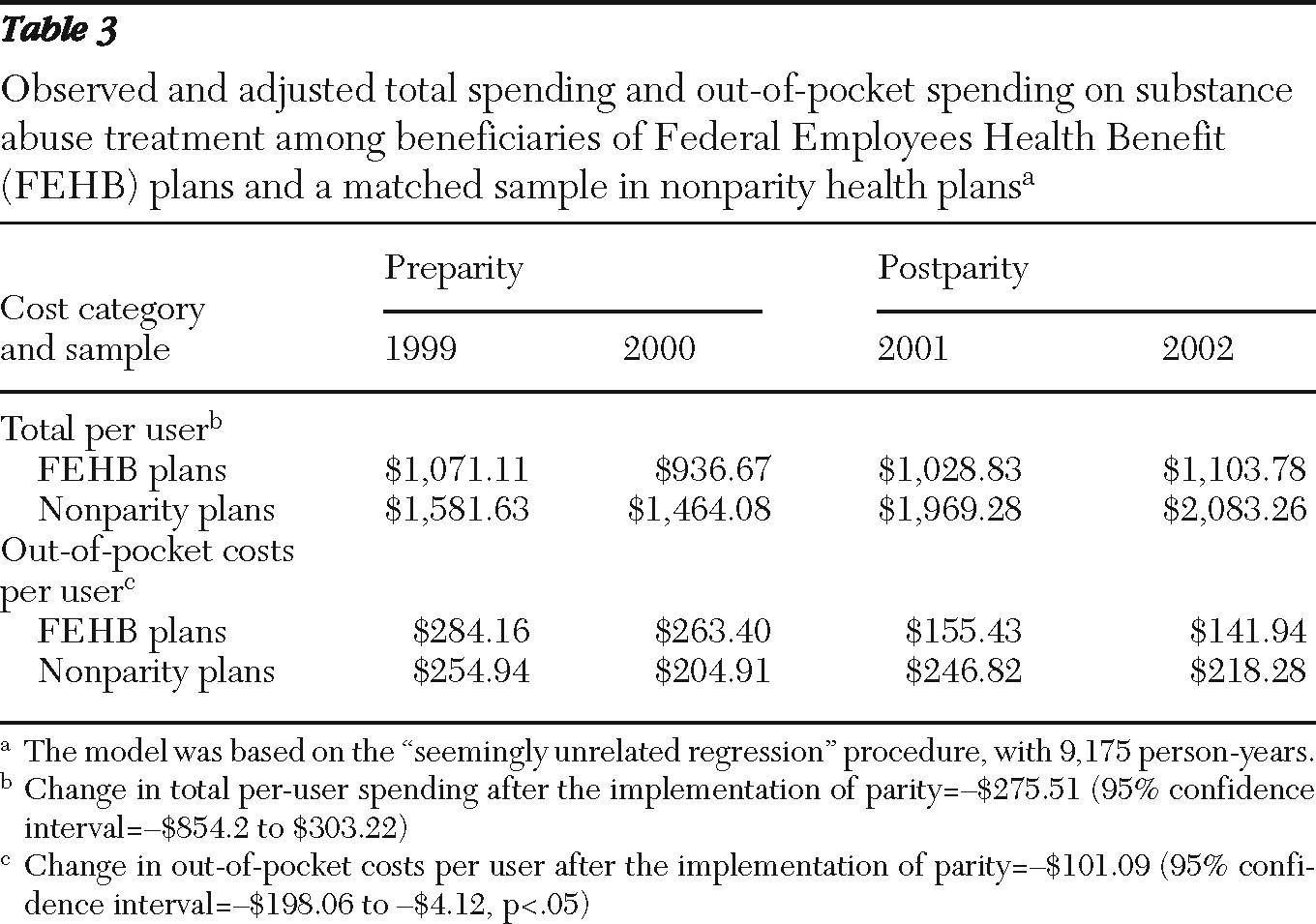
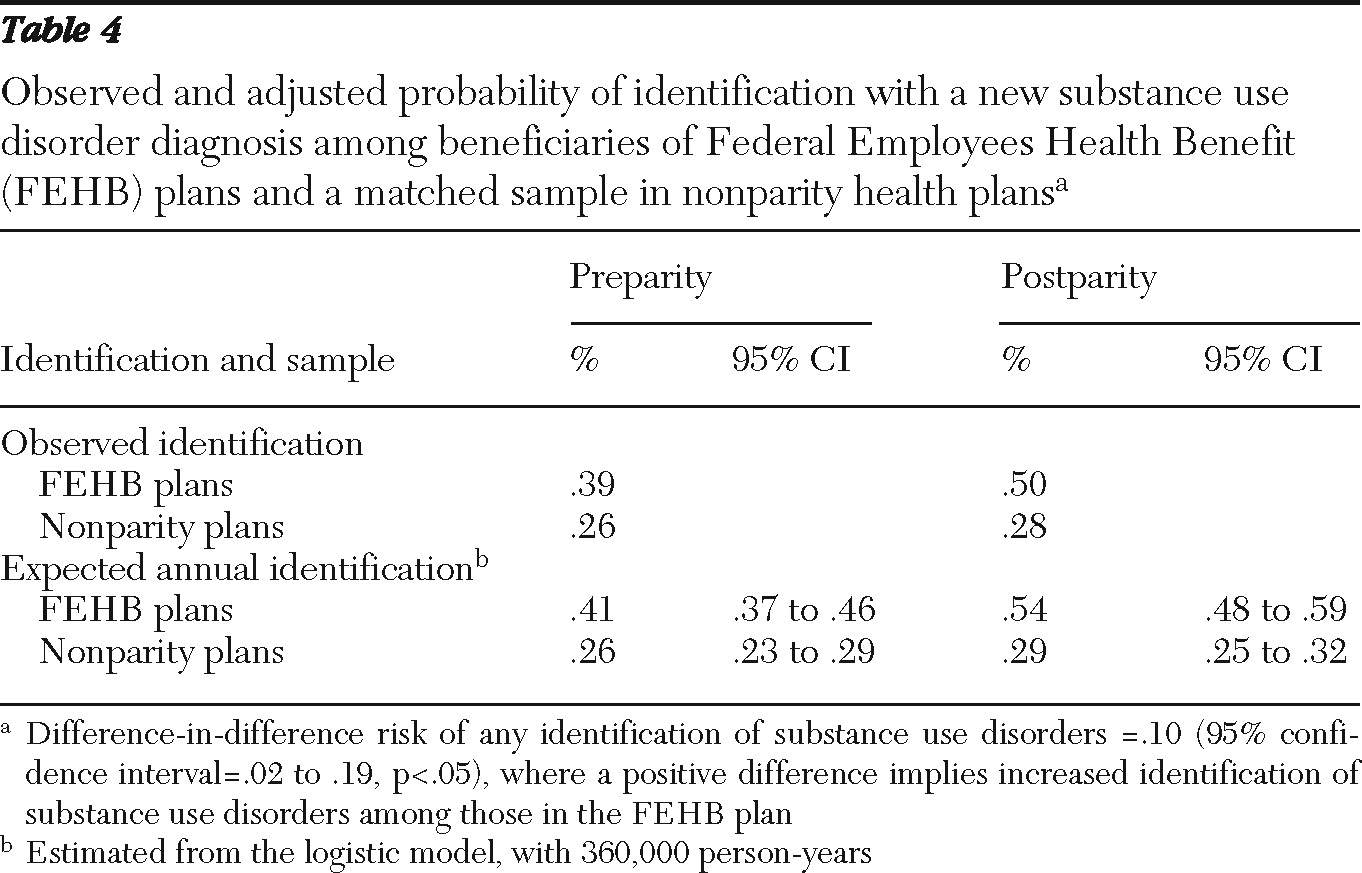
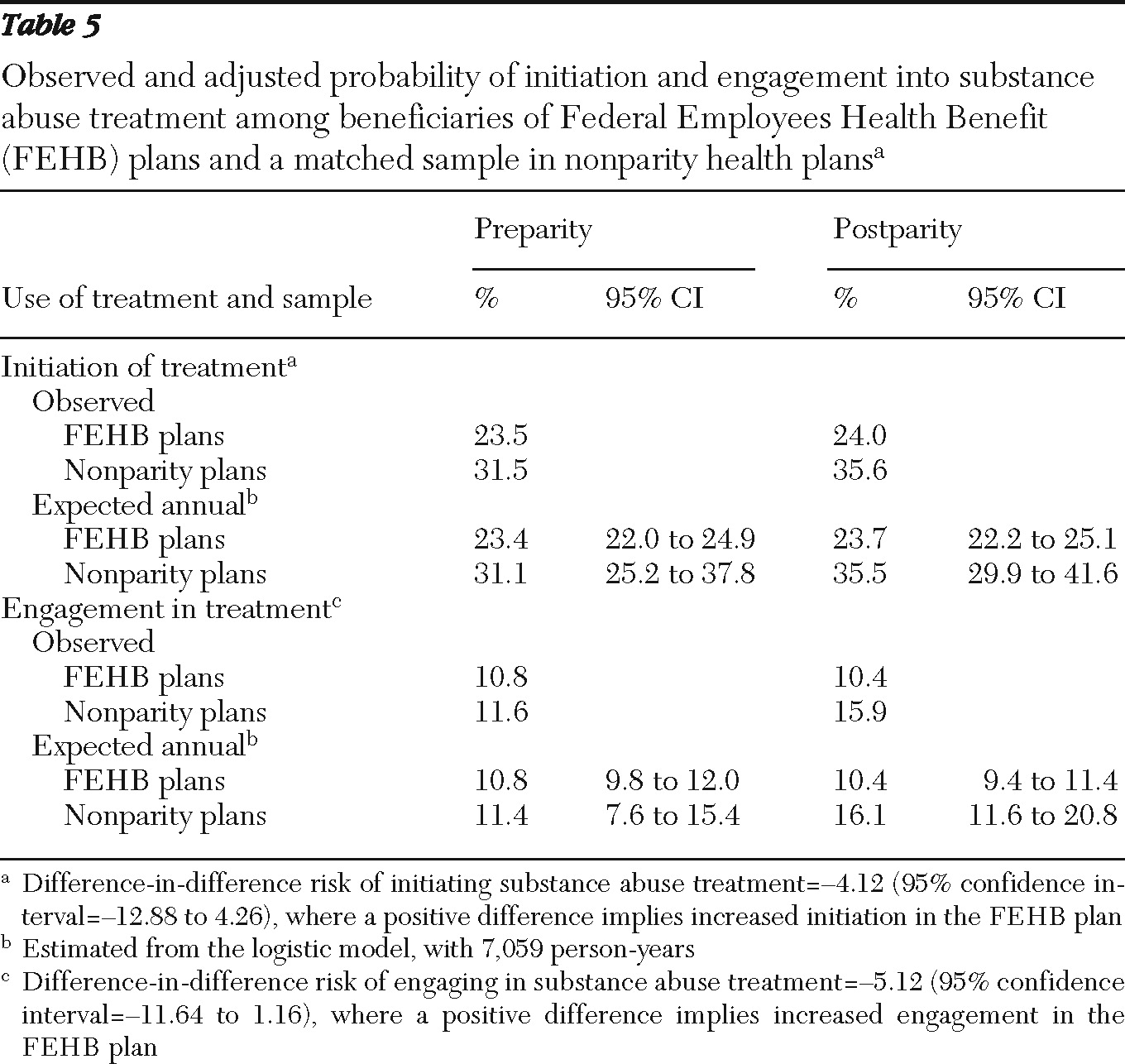
Table 3 presents the actual total and out-of-pocket substance abuse spending and the difference-in-difference estimates. Conditional on use, total substance abuse spending (as well as plan spending, data not shown) increased, but this increase did not differ by whether beneficiaries had parity coverage. However, the parity policy was associated with a significant reduction (p=.04) in average out-of-pocket substance abuse spending compared with non-FEHB plans. The difference-in-difference estimate for the probability of identification is presented in
Table 4 and indicates that with parity, more beneficiaries were identified with a substance abuse diagnosis after analyses accounted for secular trends (p<.05). No statistically significant differences were found for the probability of initiation and engagement in substance abuse treatment at the p=.05 level because both intervals included 0 (
Table 5).
Discussion and conclusions
Implementation of parity in these large FEHB plans was not associated with significant increases in the probability of using substance abuse services, after the analyses accounted for secular trends. Even though increases in total and plan substance abuse spending were smaller in FEHB plans relative to non-FEHB plans, this finding was not statistically significant. However the rate of decrease in out-of-pocket spending was significantly larger for FEHB plans. Although parity was associated with a higher probability of identifying adults with a substance abuse or dependence diagnosis, there were no measurable impacts on initiation or engagement in substance abuse treatment among those identified with a substance use disorder. These findings are generally consistent with other studies examining the effects of parity on mental health and substance abuse treatment utilization and spending when behavioral health benefits are administered by an MCO. FEHB rates of initiation and engagement were much lower compared with the rates for commercial plans nationwide (in 2004, 45.9% and 15.5%, respectively) (
17).
It is also notable that parity was associated with improved substance abuse identification rates but did not improve substance abuse treatment initiation and engagement. Our results are consistent with the FEHB parity evaluation on the quality of major depression care (
10). The results were not surprising given that quality improvement literature demonstrates that improvement typically involves concerted efforts and interventions that rely on multiple methods and approaches to result in practice change aimed at improving treatment quality (
18). The more complex the goals for practice change, the more effort is required on the part of the organization (
19,
20). More generous benefits, however, may promote improved detection of substance use disorders.
Administrators of FEHB plans were encouraged to use managed care tools, and all of the plans (except one) that we studied had carved out the management of their FEHB behavioral health benefits to a behavioral health MCO either before or concurrently with the implementation of parity. It is possible that managed behavioral health care contains the costs of substance abuse service use when out-of-pocket costs borne by beneficiaries are lowered through parity mandates. It is also possible that an adult's decision to use substance abuse treatment services is not as sensitive to price as the decision to use mental health services. Costs associated with parity for the single FEHB plan that did not utilize managed behavioral health care were not significantly different from those of the other plans we studied, and other research has suggested that substance abuse treatment is less price sensitive than mental health treatment (
21).
Our study has several limitations. Diagnoses of substance use disorders are surely underreported in claims data, resulting in an undercount of total substance abuse services. Although we used substance abuse-specific procedure codes and diagnoses and multiple methods for identifying the use of substance abuse services, we likely did not identify all enrollees with a substance use disorder. In addition, we were focused on the beneficiary, and thus our analytical strategy was aimed at detecting effects on the individual beneficiary rather than on the health plan; hence we limited our analysis to enrollees who were continuously enrolled before and after the parity implementation and to only six FEHB plans. Therefore, this analysis likely excluded persons with the most severe disorders who might have lost their job because of relapse. It focused on the average effect of parity, not on the parity effect for those who are sicker and high users of substance abuse services. However, the health plans included in the analysis varied in their managed care arrangements and represented more than three million beneficiaries in the United States and more than 300,000 continuously enrolled adults. Although all of these plans were PPOs and the generalizability of these findings beyond PPO plans may be limited, the regions represented by the plans are large. Although we didn't have complete information on the level of benefit management, three of the FEHB plans, covering one-third of the sample, carved out to the same managed behavioral health care organization.
In summary, this study suggests that benefit parity in the FEHB program reduced out-of-pocket costs of substance abuse treatment for beneficiaries. Although parity had no detectable impact on the probability of utilizing treatment services, it was associated with improvement in one of three indicators of quality of substance abuse treatment services.
Acknowledgments and disclosures
The data were originally collected in a study funded by the Department of Health and Human Services (HHS-100-00-0025). This study was funded by grant P-50-DA-010233 from the National Institute on Drug Abuse through the Brandeis-Harvard Center for Managed Care and Drug Abuse Treatment. The authors thank Katya Zelevinsky, B.A., for analytic file preparation and analysis and Alisa Busch, M.D., and Dominic Hodgkin, Ph.D., for helpful comments on the manuscript.
The authors report no competing interests.