Depression is of high public health concern because it is the most common mental disorder and a primary cause of disease burden, disability (
1), long-term sickness, absence from work, and premature retirement (
2). Furthermore, it has been described as the most costly brain disorder in Europe (
3). In southern European countries, prevalence rates of depression and suicide are lower than elsewhere in Europe (
4,
5), and a recent study of depression in Spain, one of the largest southern European countries, found additional characteristics specific to this country, such as an earlier age at onset and higher rates of comorbidity and of chronicity (
5).
Health services are a crucial resource in reducing the suffering of persons with depression; however, studies have found large differences between countries in rates of depression treatment, with low overall rates (
6–
8). Although health care systems vary widely across the world, certain system characteristics, such as access to services, number of health professionals, and quality of care, contribute to the outcomes of depression treatment. Studies of service use for the treatment of depression are scarce and mostly limited to Western and Northern European countries. Although information from many countries, such as Spain, is available, it remains fragmented and incomplete.
The Spanish National Health System provides free and universal access to most types of health care. It is financed by general taxation and by out-of-pocket expenditures, including copayments for pharmacological treatments. The primary care sector acts as the gatekeeper to the system and therefore to specialized mental health care. Because administration of health care is decentralized and is the responsibility of the 17 Autonomous Communities, the number and quality of mental health services is not homogeneous across Spain. Frequently described deficiencies include lack of specific budgets for mental health, heterogeneous information systems, and insufficient coordination with primary care services (
9).
The objective of this study was to analyze service use in the past 12 months for a major depressive episode among respondents to the European Study of the Epidemiology of Mental Disorders (ESEMeD), in Spain. We estimated the level of use of services, determined the proportion of individuals using services who could be considered to have received minimally adequate treatment, and identified the sociodemographic and clinical factors associated with service use. We also compared these results with international data.
Methods
The ESEMeD-Spain study was a cross-sectional, general population, household survey conducted with a representative sample of the Spanish noninstitutionalized adult population. A detailed description of methods is available elsewhere (
10–
12).
Sampling methods
A stratified, multistage, clustered-area, probability sample without replacement design was used to guarantee the representativeness of all the regions in the country. The target population was noninstitutionalized adults (aged 18 years and older), who were identified from census tract data. The final sample included 5,473 respondents (including a random selection of 323 spouses of the married main respondents, who were also interviewed); the final response rate was 78.6%. Data collection was conducted from September 2001 to September 2002. Individuals provided informed consent to participate in the interview. Data for the individuals were weighted to account for the different probabilities of selection within households and among hard-to-reach individuals, as well as to reflect age, gender, and Autonomous Community distribution of the Spanish general population.
Interview and questionnaire
The survey instrument was the World Mental Health (WMH) Survey version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI 3.0) (
13), which is a fully structured diagnostic interview to assess disorders and treatment, as well as several additional variables, such as disease severity and disability. By means of computerized algorithms, the CIDI provides lifetime and 12-month diagnoses of mental disorders based on
DSM-IV criteria (
14). In establishing the diagnosis, CIDI rules about excluding organic mental disorders (direct physiological effects of a general medical condition, a drug, or a medication) were imposed. The CIDI was administered by trained lay interviewers using a computer-assisted personal interview.
Assessment of depression severity
Respondents were assessed for major depressive episode in the past 12 months. On the basis on researchers' consensus, individuals with the disorder were classified into three severity groups. The group with the most severe symptoms included those who had attempted suicide in the past 12 months, those who had a diagnosis of alcohol dependence with physiological dependence syndrome, and those who experienced severe role impairment (scores from 8 to 10) in at least two areas of the WMH-adapted version of the Sheehan Disability Scales (SDS). Individuals not classified as having severe symptoms were assigned to the moderate group if they had moderate role impairment in at least one domain of the SDS (a score of more than 4) or if they had alcohol dependence disorder without physiological dependence. All other individuals were classified as having mild symptoms.
Health and social services use
All respondents were asked about use of services for their “emotions or mental health problems” in the 12 months before the interview. Those reporting use of services were asked to select from a list all providers whom they visited, including psychiatrist; psychologist; general practitioner, other physician, or other health care professional; human services (outpatient treatment with a religious or spiritual advisor or with a social worker or counselor in any setting other than a specialty mental health setting); and a complementary-alternative medical sector (outpatient treatment with any other type of healer, participation in an Internet support group, or participation in a self-help group). Psychiatrists and psychologists constituted the specialized mental health category; general practitioners, other physicians, and other health professionals constituted the general medical care category; and both specialized mental health and general medical care constituted the health care sector.
The type of treatment received by individuals who reported use of a service in the health care sector was assessed. Pharmacological treatment was defined as that prescribed by a psychiatrist, general practitioner, or any other physician or health professional in the previous 12 months. Psychotherapy was defined as having more than one session in the past 12 months of psychological counseling or therapy with a mental health professional (psychiatrist or psychologist) that lasted 15 minutes or longer. Individuals who received neither drug nor psychological treatment were classified as being in the group with no active treatment.
Treatment adequacy
The definition of minimally adequate treatment followed previous research that was based on recommendations from clinical guidelines (
15–
17). It was defined as receipt of antidepressant pharmacotherapy for at least two months plus at least four visits with a psychiatrist, a general practitioner, or any other physician or health professional or at least eight sessions with a psychologist or a psychiatrist lasting an average of 15 minutes or longer. Human services and complementary-alternative medicine treatments were not considered to constitute adequate care because of the lack of experimental data documenting the effectiveness of such treatments for major depression (
18–
22).
Chronic conditions and mental disorder variables
The variable for chronic conditions included eight groups: musculoskeletal (arthritis), chronic pain (neck or back pain or other somatoform pain), digestive (stomach or intestinal ulcer), respiratory (asthma, allergies, or any other chronic lung disease), neurological problems, cancer, cardiovascular (stroke, heart attack, heart disease, or high blood pressure), and diabetes. The variable for mental disorders included mood disorders (major depressive episode or dysthymia), anxiety disorders (panic disorder, specific phobia or social phobia, generalized anxiety disorder, posttraumatic stress disorder, and agoraphobia without panic), and alcohol abuse or dependence.
Data analysis
All analyses were performed with SASTM software, version 9.1, of the SAS System for Windows as well as SUDAAN, version 9.0, a statistical package used to estimate standard errors of data obtained from surveys with complex designs. Data analyses were carried out at the IMIM-Hospital del Mar in Barcelona, Spain, and at Harvard University in Boston.
Results
Lifetime prevalence of a major depressive episode in the overall sample was 10.6%, and 12-month prevalence was 4.0%.
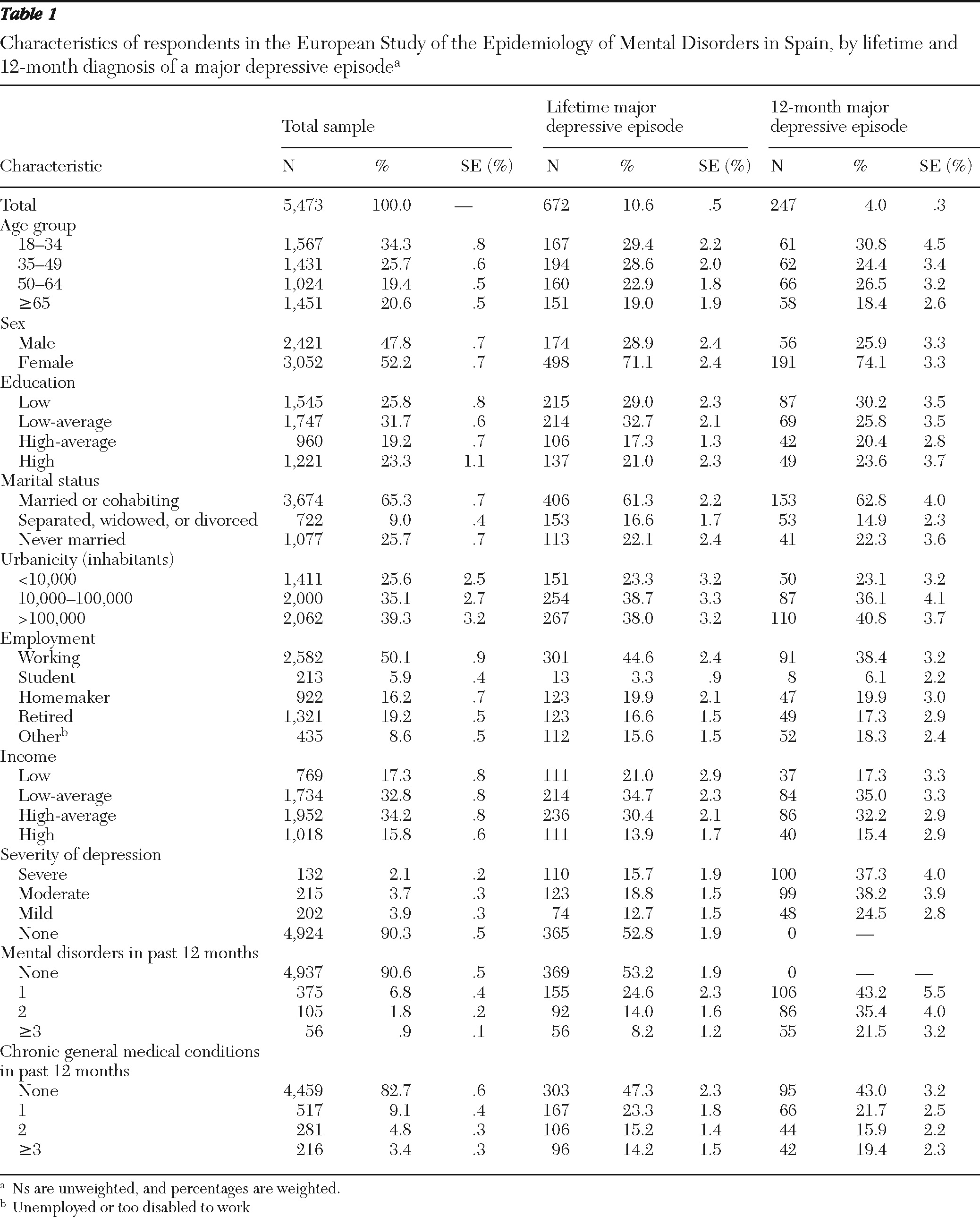
Table 1 presents data on sociodemographic characteristics of the total sample and of those with a lifetime and 12-month major depressive episode.
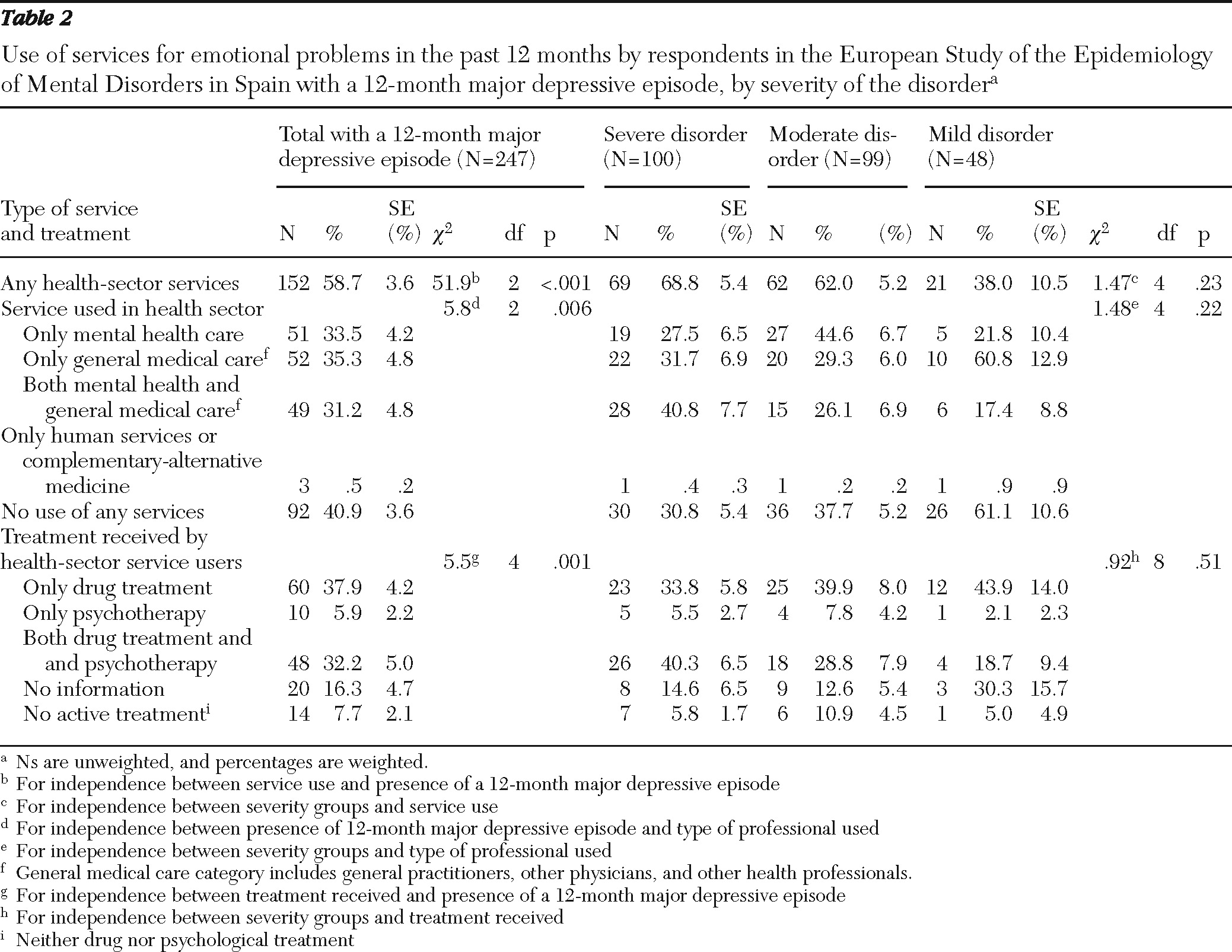
Among respondents with a depressive disorder in the past 12 months, 59.1% had used some type of service in the past 12 months for their emotional problems. As shown in
Table 2, the highest proportion of service users (58.7%) reported use of services in the health care sector (either general medical care or specialized mental health). Among those who used services in the health care sector, the highest proportion reported use only in general medical care (35.3%).
Among respondents who had used past-year services for emotional problems in the heath care sector, at least 76% received some type of active treatment: 70.1% reported receiving psychopharmacological treatment, either alone (37.9%) or combined with psychotherapy (32.2%). Receipt of no active treatment was highest among respondents with moderate major depressive episode (10.9%) and lowest among those with a mild disorder (5.0%).
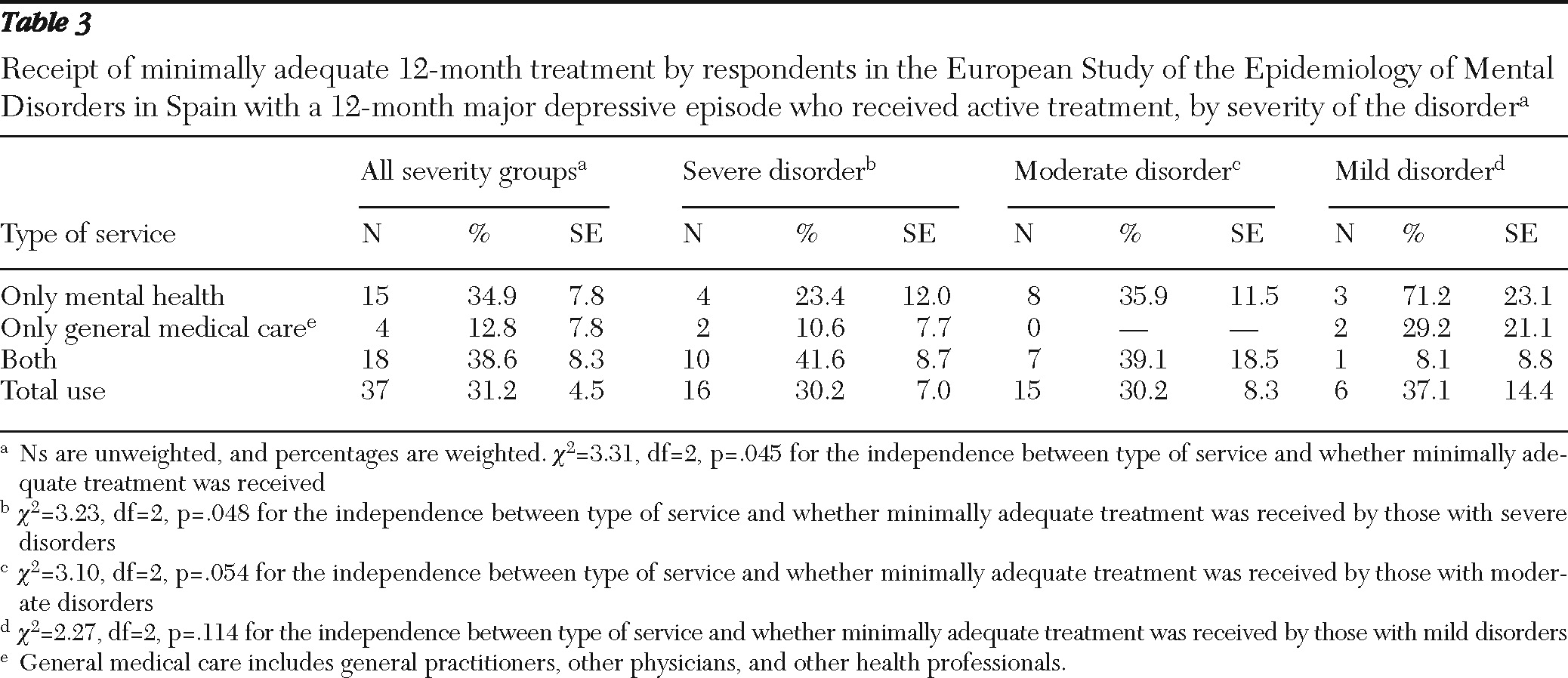
As shown in
Table 3, among respondents who had received active treatment in the past 12 months from providers in the health care sector, 31.2% received treatment that met criteria for minimal adequacy. In the overall sample, meaningful differences were found by type of health service used: respondents who received both specialized mental health care and general medical care accounted for the highest proportion of those receiving minimally adequate care (38.6%), and the lowest proportion was among those who received services in general medical care only (12.8%). These differences were also found among respondents with severe major depressive episode.
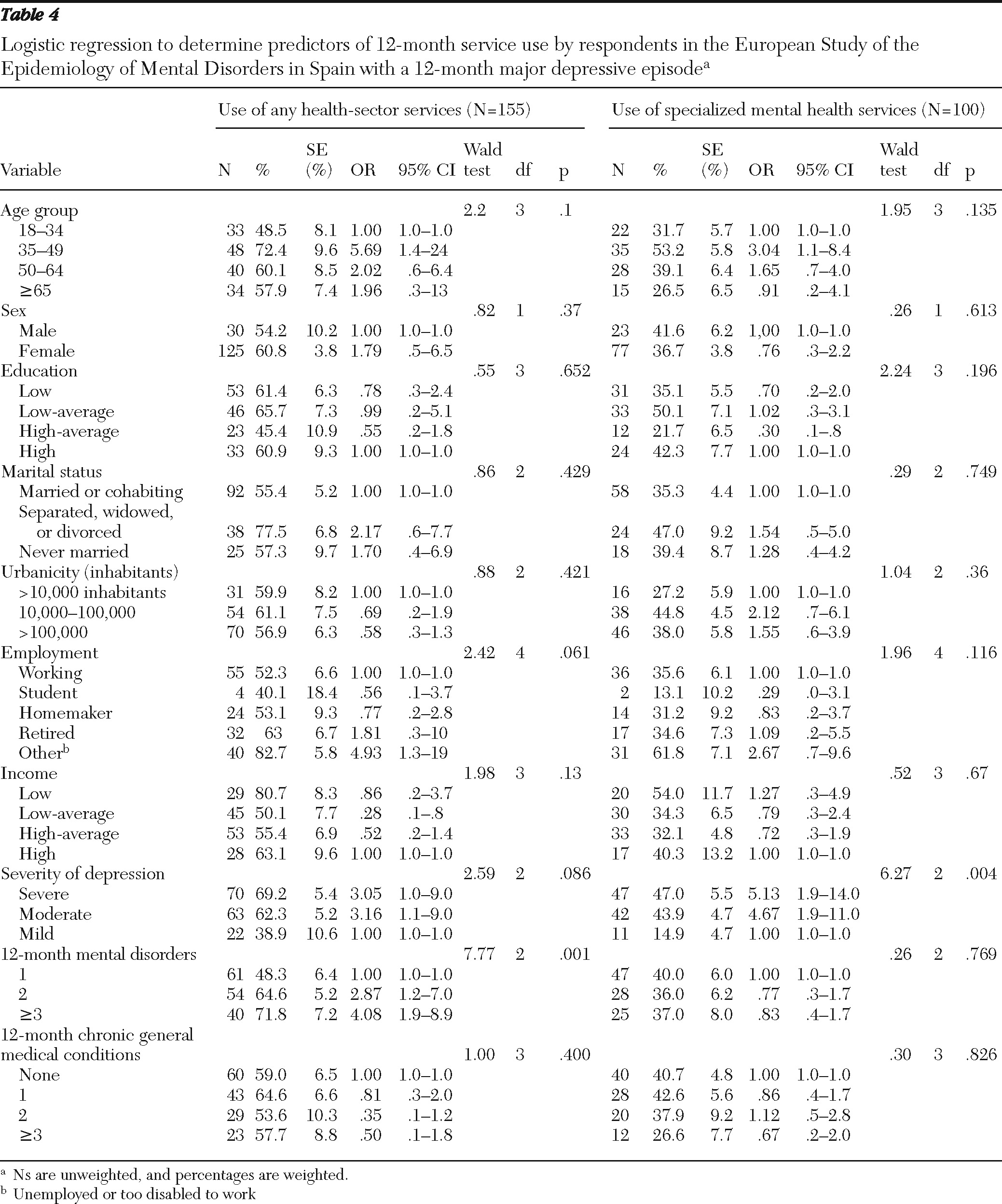
Results of logistic regression analyses of potential predictors of past-year service use among respondents with a 12-month major depressive episode are shown in
Table 4. Respondents in the group aged 35–49 years were more likely than those in the other age groups to have used any services for their emotional problems within the past year (OR=5.7). Service use was also more likely among those in the “other” employment group (unemployed or too disabled to work) (OR=4.9), compared with those who were employed. Respondents who had a moderate disorder were more likely (OR=3.2) than those in the other severity groups to have used any services. Respondents who had more than one 12-month mental disorder (that is, a mental disorder comorbid with their depression) were significantly more likely than those with depression only to use any services (two mental disorders, OR=2.9; three or more mental disorders, OR=4.1). On the other hand, respondents with a low-average income were less likely than those with a high income to have used any services for their emotional problems in the past 12 months (OR=.3).
The regression analyses also examined use of specialized mental health services in the past 12 months (
Table 4). Respondents in the group aged 35–49 were more likely than those aged 18–34 to use these services (OR=3.0). Those with a severe or moderate disorder were significantly more likely to use these services than those with a mild disorder (OR=5.1 and OR=4.7, respectively). On the other hand, those with a high-average education level were less likely than those with a high level to use specialized services (OR=.3).
Discussion
The study found that 40.9% of respondents to ESEMeD-Spain with a 12-month major depressive episode reported not having used any type of service for their emotional problems in the past year. Moreover, 68.8% of those who received active treatment in the health care sector (specialized mental health or general medical care) did not receive minimally adequate treatment. Thus only 15.0% of all those with a 12-month major depressive episode had received appropriate care. Of particular concern is the 30.8% of those with a severe disorder who did not use any type of service for their emotional problems.
By far, psychotropic medication was the treatment most used, either alone or (less frequently) in combination with psychological treatment. Higher odds of any service use were found among respondents with a moderate disorder, those with a comorbid mental disorder, those who were unemployed or too disabled to work, and middle-aged respondents.
Study limitations and strengths
Our results should be interpreted within the context of some limitations. First, information about treatment was self-reported, which could have led to recall bias. Previous studies have found that self-reports of service use for some mental disorders may be higher than use documented in administrative records (
23,
24). The WMH Survey tried to reduce recall bias by excluding respondents who failed to say that they would think carefully and answer honestly. Furthermore, use of a 12-month time frame can further reduce the risk of recall bias. Second, some analyses consisted of small numbers of respondents, and this might have affected the reliability of results. Third, ESEMeD excluded several population groups, such as those who were institutionalized or homeless. Although service use patterns of these groups may be different, their relative size is small, and it could be argued that overall population estimates would not diverge considerably if they were included. Fourth, there is no consensus on criteria for defining minimally adequate treatment; however, to our knowledge, the relationship between various criteria and significant clinical outcomes has not been studied. Fifth, the Spanish National Health System comprises 17 regional systems whose management relies on each regional government. As a consequence, the level of development of the mental health network, the allocation of economic resources, and the population density of professionals vary across regions; these differences may influence the use of services. Because of limitations in sample size, it was not possible to perform a more detailed analysis that would offer a clearer picture of probable regional differences.
With these limitations in mind, we note that this is the first study that provides information about the use of services for a major depressive episode in Spain that is based on a nationally representative sample and that used a standardized methodology that allows for international comparisons. Previous research was restricted to specific regions and population subgroups (
25,
26) or clinical samples (
27) or used mixed methodologies, which provided an incomplete picture of service use for depression.
Use of services
Our findings show that almost half of respondents with a major depressive episode did not use services in the health care sector for their emotional problems in the year before the interview. Although concrete and easily comparable data are lacking, some studies have found lower use of health services for mental disorders in certain southern European countries, such as Spain and Italy, compared with other European countries, but the rates are still higher than those found in many low-income American samples or in Asian countries (
6,
28). Comparable data on service use by individuals with major depression are even scarcer, but studies have shown that use is higher in Spain than in countries such as Italy and Germany (
29) and lower than in some northern European countries, such as Finland, Ireland, and the United Kingdom (
30).
Although underrecognition and undertreatment of common mental disorders are frequent in most countries, substantive cross-national differences in treatment rates have been described. Treatment rates ranging from 50% to 79% in high-income countries have been reported, with rates typically lower in low-income regions (
6). Reasons for these differences are not well known, but several factors have been proposed. They include factors that predispose patients to seek treatment, factors related to the type and amount of services available from the health care system, and factors related to health care professionals' ability to provide an adequate response to the need for treatment (
6,
31–
35). The effect of social networks and support, which might be stronger in Spain than in other European countries (
36), has also been discussed in the literature as either reducing service use by helping an individual to cope with stress or increasing service use by supporting treatment seeking (
37). Although an extensive review of these factors is beyond the scope of this article, the relevant findings are summarized below.
Patient-related factors.
A personal level of comfort and confidence about consulting with professionals has been considered the most important factor in help seeking for depression, together with personal understanding and self-evaluation of the problem and the anticipated or experienced reactions of family and friends (
31,
32). Attitudes toward seeking mental health care seem to be more positive in Spain than in other European countries, and Spaniards seem to place greater trust in treatments provided by health care professionals (
38). In regard to stigma, a well-known cultural barrier to help seeking for mental disorders (
32), two recent studies showed that stigma may be less prevalent in Spain than in other European countries (
39,
40).
Health system-related factors.
The ability to access professional care is a key feature of health systems and also influences service use for mental disorders. Access to services is free and universal in the Spanish National Health System, as is the case in many other European countries, where treatment rates are, however, higher. A link between a country's overall spending on health care and the rate of treatment for mental disorders has also been described (
6), and available data show that the amount spent in Spain is lower than the European average; this is also true of spending on mental health, which remains around 5% of Spain's total health care budget—one of the lowest spending rates in the European Union (
41–
43). The availability of services and of professionals is another relevant determinant that has also been linked to the use of services for depression. Studies have shown that regions with the lowest resources often have lower rates of consultation with health care professionals (
44). Spain has fewer psychiatrists and psychologists and fewer available mental health services than many other countries with the same level of development, and differences are even greater for psychiatric nurses and social workers (
9,
42,
43).
Factors related to health care professionals.
The Spanish National Health System is based on primary care, and referral from a general practitioner is usually required to gain access to specialized mental health services. Thus general practitioners act as gatekeepers of the system and have a key role in the correct detection and early management of most cases of depression. This is especially relevant in light of the high prevalence of major depression in primary care (
45) and the evidence linking poor recognition of depression in primary care with worse short-term outcomes (
46). In fact, underrecognition of depression in primary care has been extensively reported (
47–
49), and a recent meta-analysis that included more than 50,000 international patients showed that correct identification of depression by general practitioners occurred in only 47.3% of cases (
50). This worrying situation has also been described in Spain (
51,
52), but international comparisons are scarce.
Roles of general practitioners and mental health specialists
Our results show that the proportion of respondents who sought service in the general medical care sector was only slightly higher than the proportion who visited mental health specialists. This finding is in contrast to other European countries and regions of the world, where general practitioners are clearly the professionals most frequently involved in the treatment of depression (
6,
44). This difference might be partly explained by the higher rates of referral to mental health specialists by general practitioners that have been described in Spain (
44). These higher referral rates could be considered an attempt to improve the efficiency of a short-resourced health system. Additional factors, such as the relative delay in mental health care reform in Spain, may help explain why individuals with mild disorders were more likely to receive specialized mental health care.
Sociodemographic and clinical correlates of use
The likelihood of use of services for depression has been linked to a variety of sociodemographic factors, such as middle age, female gender, higher education and income level, and not being married (
6,
16,
53,
54). However, our results support only a few of them. Of special concern is our finding that women were no more likely than men to seek treatment. This finding should receive attention because the higher prevalence of depression among women compared with men in Spain was found to be much higher than in many other countries (
5,
55,
56).
Symptom severity is another major determinant of service use (
30,
57,
58), and monotonic relationships between severity and the probability of service use have been previously described (
6). Our results show that among individuals using any health sector services, those with a moderate disorder had higher odds of receiving treatment than individuals with mild disorders. Further research should be undertaken to confirm these findings—in particular, the role of severity and of gender in help seeking. Also, the finding that 31.7% of those with a severe disorder received care only from a general practitioner raises some concern about possible misallocations of scarce specialized resources, especially when the misallocations affect patients with higher risks of serious complications.
Minimally adequate treatment
In our study 31.2% of the patients with a major depressive episode who received active treatment from general medical or mental health specialty care received minimally adequate treatment, a rate considerably lower than in other European countries (
17). Consistent with previous studies, our study found low overall rates of treatment adequacy (
6,
59) and more adequate treatment in specialized settings (
16,
60). Reasons for the low rate of treatment adequacy are unclear, but they presumably involve provider factors, such as inadequate training and failure to adhere to guidelines (
16). Inadequate treatment has significant health and economic consequences, because treatments that meet clinical guidelines are more cost-effective and have been shown to decrease the number of years lived with a disability (
61).
Conclusions
Taken together the results offer a complex picture of patterns of service use for a major depressive episode in Spain. They include a less clear influence of disorder severity, a less relevant role for general practitioners than for mental health specialists, varying effects of sociodemographic factors, and a lower overall rate of minimally adequate treatment. Low rates of service use for major depression in a country such as Spain, with free and universal access to mental health care and a population with more positive attitudes toward help seeking for mental health problems, are worrisome and should call for a more proactive attitude of the health system. In particular, rates of comorbidity and of chronicity are higher in Spain than in other European countries (
5), and both are a possible consequence of inadequate treatment and a possible cause of increased costs of major depression. Potential country-specific barriers to treatment, such as lower availability of services and of professionals and lower health care spending for mental health, may contribute to the low rates of service use. Although there are many budgetary constraints and competing priorities, reducing these barriers to treatment should be seriously considered to improve access to mental health care in Spain.
Efforts should be made to enable general practitioners to better detect and manage depression, which may involve changes in their training and more effective development and dissemination of clinical guidelines. In addition, the fact that no gender differences were found in the likelihood of receiving treatment should stimulate specific actions aimed at increasing treatment rates among women as a high-risk population group. This is also true for the youngest cohorts, especially considering that the age at onset of depression is lower in Spain (early 30s) than the European average (late 30s) (
5) and that early intervention can improve the prognosis of this often chronic and highly disabling disorder.
Acknowledgments and disclosures
The ESEMeD project (
www.epremed.org) was funded by contracts QLG5-1999-01042 and SANCO-2004123 from the European Commission; the Piedmont Region of Italy; grant FIS 00/0028-02 from the Fondo de Investigación Sanitaria (FIS), Instituto de Salud Carlos III, Spain; grant SAF 2000-158-CE from the Ministerio de Ciencia y Tecnologáa, Spain; Departament de Salut, Generalitat de Catalunya, Spain; and by other local agencies and by an unrestricted educational grant from GlaxoSmithKline. ESEMeD is carried out in conjunction with the WHO WMH Survey Initiative. The authors thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by grant R01MH070884 from the U.S. National Institute of Mental Health; the John D. and Catherine T. MacArthur Foundation; the Pfizer Foundation; grants R13-MH066849, R01-MH069864, and R01 DA016558 from the U.S. Public Health Service; grant FIRCA R03-TW006481 from the Fogarty International Center; the Pan American Health Organization; the Eli Lilly and Company Foundation; Ortho-McNeil Pharmaceuticals, Inc.; GlaxoSmithKline; Bristol-Myers Squibb; and Shire. The funding institutions had no further role in study design; in collection, analysis, and interpretation of data; in report writing; or in the decision to submit the report for publication.
The authors report no competing interests.