Prevention in psychiatry is possible. A scientific base of evidence shows that we can prevent many mental, emotional, and behavioral disorders before they begin. This robust evidence is presented in the landmark 2009 Institute of Medicine (IOM) report titled
Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities (
1). In this article we highlight and expand key points from the IOM report. Using a developmental perspective, we discuss the effectiveness and implementation of prevention for mental, emotional, and behavioral disorders. With the possibility of reducing the human suffering of mental illness and the economic costs associated with it, psychiatry must act to implement preventive practice.
In our roles as psychiatrists, we see people after symptoms of a mental illness have emerged, after dysfunction has begun. We work hard to provide our best treatments to improve symptoms and outcomes for our patients. We take pride in stopping further symptom development, lessening episodes of illness, and facilitating recovery. Yet, how often do we work with people who do not show problems, in an effort to reduce their risk of developing future mental, emotional, or behavioral disorders?
There is an established and growing scientific body of evidence demonstrating methods to prevent mental illness before it starts. These preventive strategies reduce risk factors, enhance protective factors, and practice mental health promotion. They require using universal approaches that address the entire population, selective approaches for people at elevated risk, and indicated approaches for people showing early signs of an illness. Prevention requires a paradigm shift to implementing strategies before the onset of illness and treating the population before waiting for people to come to our door.
Evidence for prevention
The scientific evidence for prevention is growing. In 1994 the IOM released its first report highlighting models of prevention for selected mental disorders, titled
Reducing Risks for Mental Disorders: Frontiers for Prevention Research (
2). Primarily, this report challenged the mental health community to apply a risk factor model—as is used in preventing cardiovascular disease and injuries—to the prevention of mental illness. The report recommended increased research and implementation of effective programs for primary prevention of mental disorders. Moreover, it introduced the categories of universal, selective, and indicated prevention to encourage multiple primary preventive interventions toward groups with differing risks.
Since that 1994 report, research and evidence for prevention has accumulated at an increasing rate. Approximately 400 additional randomized controlled prevention trials for mental, emotional, and behavioral disorders have been published, and data have accumulated from other types of trials, such as natural experiments and time-series analyses (
1). This evidence provided the basis for the family, school, community, and office interventions presented in the 2009 IOM report. In this article we discuss selected evidence most relevant to psychiatrists and elucidate key findings from that report to illustrate the science of prevention—core principles of prevention in mental health (see box on this page), risk factors and protective factors for mental illness, and the fundamental neuroscience underlying prevention science. We also issue recommendations and discuss building the infrastructure for effective prevention.
A developmental perspective
Prevention requires asking the question, “What does a child need one, three, and five years down the line?” It is inherently developmental in an effort to time preventive interventions to have their maximal impact, depending on the age and development of the child.
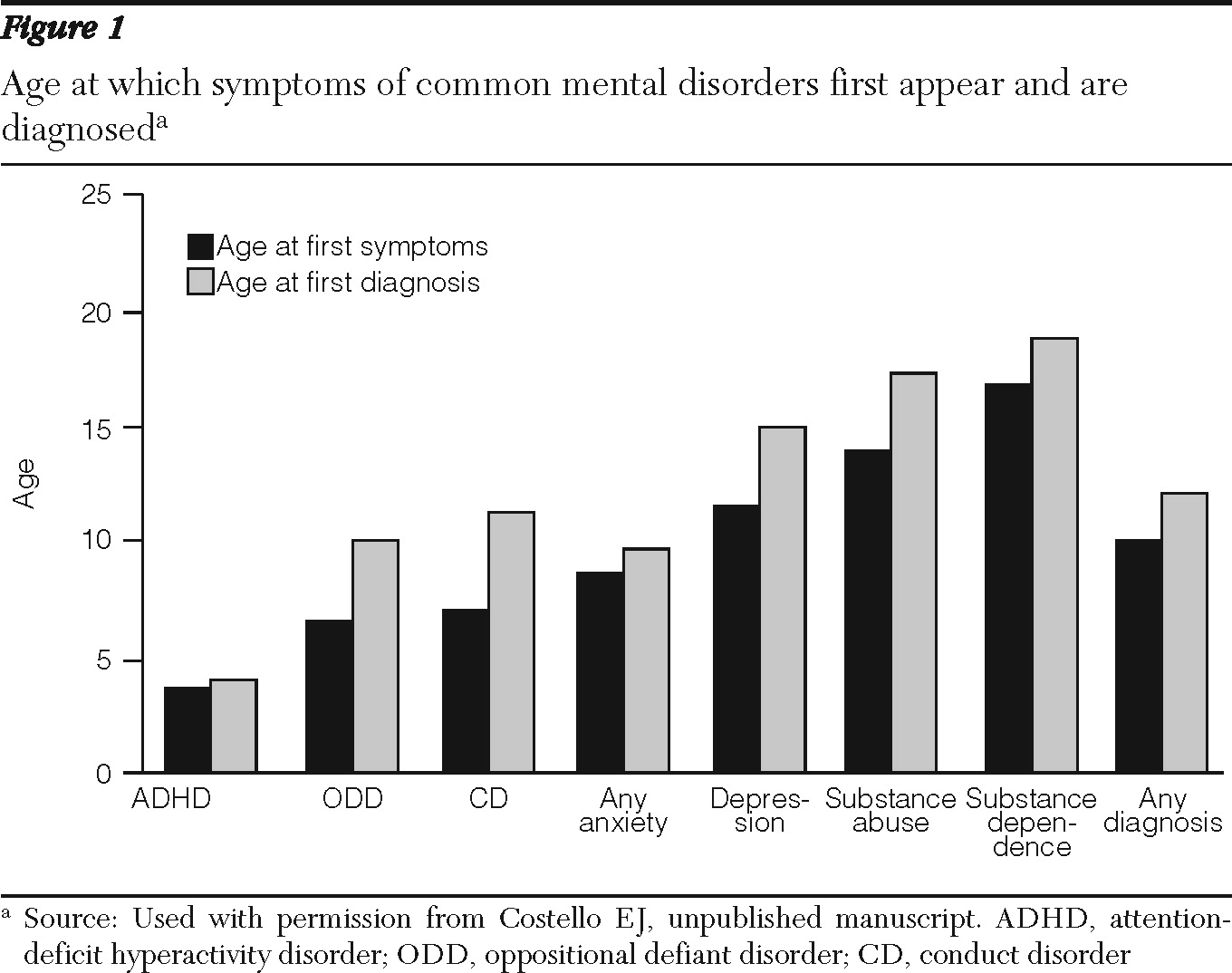
Prevention focuses on young people because half of all lifetime cases of mental, emotional, and behavioral disorders start by age 14, and three-fourths of disorders start by age 24 (
3). In addition, first symptoms typically occur two to four years before progressing to diagnosable disorders. This prevention window, depicted in
Figure 1, provides years of distinct opportunities for indicated preventive interventions as well as universal and selective interventions that could be used before symptoms arise (
1).
Risk factors and protective factors
The characteristic periods in which symptoms usually appear and a diagnosis is made likely represent key biological and psychosocial risk factors that occur at those ages (
4). Identified groups of risk factors, in addition to biological and genetic disease vulnerabilities, include socioeconomic disadvantage, family dysfunction, parental risk characteristics, and stressful life events. Knowing this allows us to better target risk factors and promote protective factors for different age groups. This emphasis on developmentally appropriate risk and protective factors was not a feature of the report in 1994 and represents a significant advance.
In addition, promoting developmental competencies is central to understanding the related concept of mental well-being. The IOM report positively defined mental health as an “ability to achieve developmentally appropriate tasks (developmental competence); a positive sense of self-esteem, mastery, well being, and social inclusion; and the ability to cope with adversity” (
1). Just as in physical fitness, where individuals may have better health than others, mental well-being exists on a spectrum regardless of whether individuals are symptomatic. Furthering developmental competencies improves mental health and simultaneously serves as a protective factor against the onset of mental illness (
5).
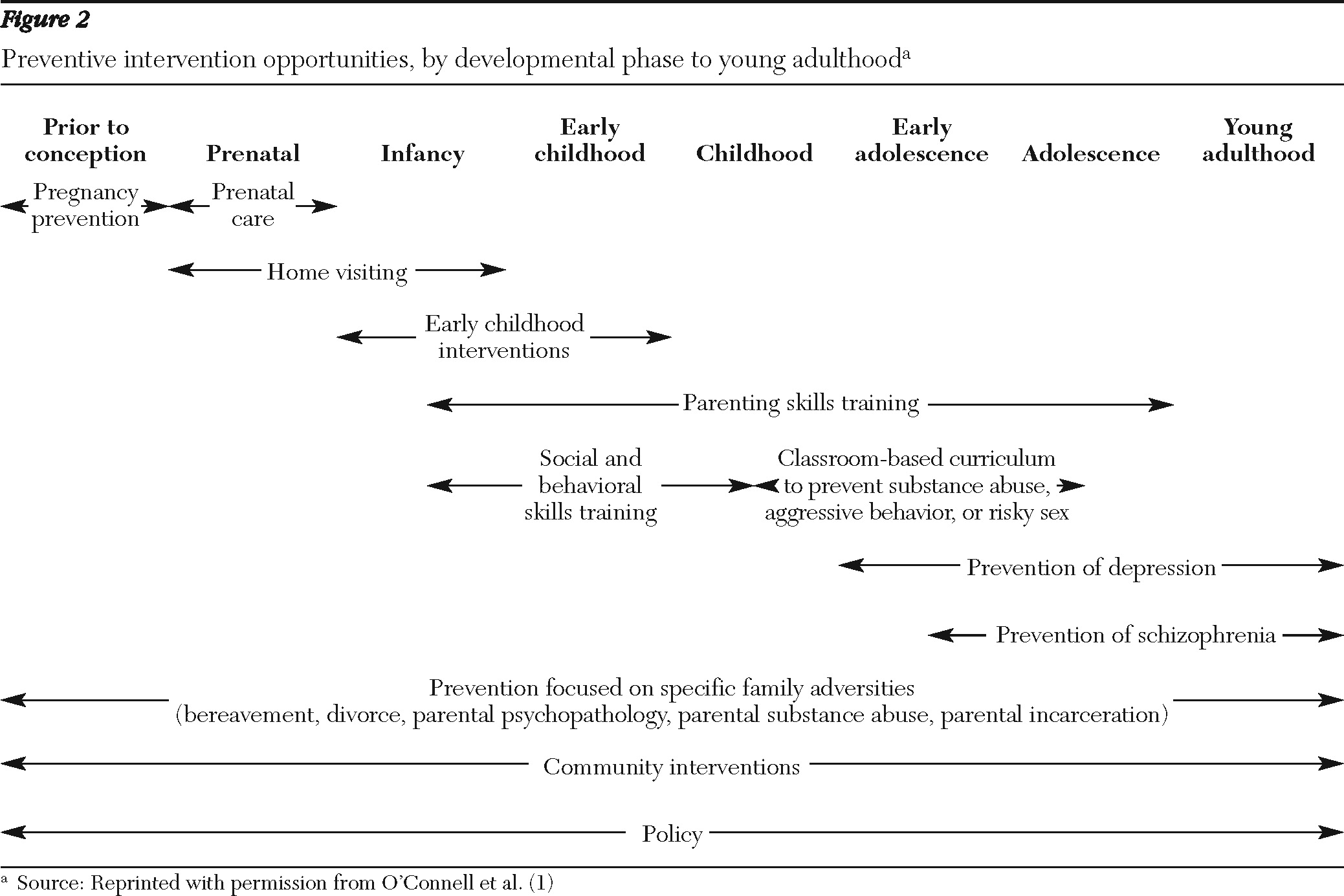
Preventive interventions
Considering these developmental risk and protective factors, we have multiple opportunities for preventive interventions through an individual's young adulthood (
Figure 2). Early in the course of development, there is evidence supporting interventions that are broad based and that foster strengths and skills within the family, the parents, and the child. These include high-quality out-of-home care and home visitation by a nurse, as well as interventions such as adequate nutrition during pregnancy (
6,
7).
During the school years, interventions that both foster academic development and cultivate social and emotional skills offer great promise (
8,
9). In adolescence, interventions targeted to more specific disorders are appropriate—in particular, substance abuse prevention and depression prevention (
10–
13).
Policy interventions that strengthen communities and support families throughout their children's developmental stages are preventive. In addition, many individual programs are preventive for children from families in distress, such as from divorce, parental depression, bereavement, or serious medical illness (
14,
15).
Neuroscience
Developmental neuroscience supports the possibility of prevention. The core construct of developmental plasticity complements the core premise of preventive intervention—that it is possible to intervene in the environments of developing children and their families in order to maximize development (
16).
Environmental influences are a factor in all stages of brain development. Early stages of brain development, including cell proliferation, differentiation, and migration, are primarily under the control of regulatory genes (
17). However, these stages can be disturbed by nutritional deficiencies, infections, toxins, and substance use, which predispose the individual to cognitive, behavioral, and mental health problems (
7,
18,
19). Thus, beginning in gestation, healthy maternal and prenatal care can facilitate proper brain development and the prevention of problems or illness.
From the early childhood years through the early adult years, synapse formations and neural refinement are responsive to stimulation and deprivation (
20,
21). Thus preventive interventions can enlist parents, families, and communities to provide nurturing care for the child or young adult. In the adult years, brain plasticity continues, which allows for changes in self-regulation or the establishment of protective factors like social support. A constant interplay of genetics and a person's environment governs mental disorders. The environment affects people differently, depending on their genetics, and particular genetic risks activate only with certain environmental influences (
22).
Evidence-based interventions
The following interventions are particularly relevant to psychiatrists because they either provide evidence about the prevention of specific diseases or focus on the social and emotional skills of parents, a regular clinical population group. Many other preventive examples are detailed in the IOM report.
Parenting programs
Parenting programs have evidence-based, preventive outcomes for children. These programs have been effectively used as primary prevention for children without symptoms (universal prevention), with elevated risk factors (selective prevention), and with subsyndromal symptoms (indicated prevention).
Most of these programs work with parents of preschool-age through middle school-age children to encourage noncritical, consistent disciplinary techniques and positive interactions with their children. Many also focus on social skills and emotional communication. The direct outcomes of these programs for parents have included increased competency in using parenting techniques, improved parent self-confidence, and improved communication within the family (
6,
23,
24).
Parenting programs have demonstrated long-term, decreased aggressive and antisocial behaviors (
24–
26), less substance use (
10–
12), and fewer arrests for the children of the involved parents (
27). As a group, parenting programs also demonstrated improved academic success and better classroom behavior of the children (
28,
29). The outcomes of parenting programs have been replicated in many settings, including different regions (
30), different countries (
24,
31), and different cultural groups, including African-American populations (
32).
These parenting programs work by two primary mechanisms. They provide caregivers with social and emotional skills to support youths, and they provide youths with an environment that cultivates the social and emotional skills necessary for healthy affect regulation (
33).
Prevention of depression
Another area that shows great promise is the prevention of depression. The preventive trials that have shown the strongest results have been with two high-risk groups: high-risk adolescents (
13,
34–
36) and pregnant women (
13,
37,
38). The most common methods of preventing the onset of depressive disorders are using cognitive-behavioral strategies and psychoeducational, family-based approaches.
Challenging negative assumptions in cognitive-behavioral groups has been shown in multisite trials to be effective for adolescents (
39) of various populations and cultural groups (
40). Using a cognitive approach delivered through the schools, the Penn Resiliency Program cut the rate of moderate to severe depressive symptoms in half (
41). This program has been shown to be adaptable and beneficial for Latino clients (
42).
Psychoeducational approaches involving parents and the family in conversations about depression have led to decreases in depressive symptomatology and overall increases in family functioning (
43). Similar results have been shown with inner-city, single-parent families in racial-ethnic minority groups (
44), Latino families (
45), and in settings like Head Start (
46,
47) and in a wide array of prevention programs in Europe (
48).
Two separate meta-analyses confirmed that parenting programs reduce depressive symptoms among youths (
49) and reduce the incidence of depressive disorders (
50). Some evidence has shown similar strategies to be effective in the prevention of anxiety disorders (
51,
52).
Evidence confirms the value of social and emotional skills training across the school-age years. Various school-based and other programs to foster social and emotional learning have shown significant increases in academic functioning and reduction in symptomatology (
53,
54). Some, including the Baltimore City Project, have shown that interventions delivered in first or second grade can have effects into late adolescence (
55). The PATHS program (Promoting Alternative Thinking Strategies) provides a particularly powerful example of how emotional understanding and regulation can reduce aggressive, disruptive, and depressive symptoms (
53,
56). There was also strong support for interventions that involve multiple sectors at once. For example, the Seattle Social Development Project delivered an intervention that involved parents, teachers, and schoolchildren simultaneously during the grammar school years. This intervention showed long-term positive effects on mental health more than a decade later (
57).
Savings and the interdisciplinary nature of prevention
These approaches highlight the substantial economic savings that can materialize with prevention. The cost of mental, emotional, and behavioral disorders for young people was estimated at $247 billion in 2007, with consideration of direct costs of mental health and health services, productivity, and crime (
1). This estimate did not consider indirect costs, such as the cost for a family to care for a child with mental illness or the additional cost for a school to educate him or her.
Prevention programs would save these costs. Aos and colleagues' (
58) cost-benefit analysis showed that savings from effective programs far outweighed their costs. For example, the Strengthening Families Program realized reduced drug use, reduced delinquency, and increased academic performance (
10–
12,
59,
60). It created savings for families, schools, the juvenile justice system, and the health and mental health care systems. These outcomes in such various systems highlight the interdisciplinary nature and savings of prevention, estimated at $8 for every $1 invested in this program (
58).
These benefits and outcomes have the potential to last many years, multiplying these savings over the lifetimes of the youths affected. Many parenting programs have documented multiyear outcomes (
15,
25,
59). In addition, the Seattle Social Development Project showed sustained interdisciplinary outcomes over at least 15 years after an elementary school intervention. Into their mid- to late-20s, program participants showed significantly fewer mental disorders, and they sustained positive directional patterns for 27 out of the 28 tracked outcomes across school, work, community, health, mental health, crime, and sexual behaviors (
57). An independent cost analysis estimated that this project returned $3.14 for every dollar spent (
58).
More than economics
Beyond the economic argument that billions of dollars could be saved in health care costs, practicing prevention supports the central mission of mental health promotion—to improve people's lives. Effective prevention reduces illness and its associated suffering. Currently, mental, emotional, and behavioral disorders create the largest burden of disease in the United States for any category of illness (
61) because of their early onset and length of morbidity. In youths aged 15–24, almost half of disability-adjusted life years lost are associated with mental, emotional, and behavioral disorders (
1). In addition to the morbidity, chronic mental illnesses are associated with up to 25 years of premature mortality (
62). Effective prevention alleviates this suffering and stops the impact of disability and disruptive behaviors of mental illness on the lives of individuals and families.
At the same time, the outcomes of the preventive interventions create more developmentally competent children with enhanced social and emotional skills, better academic achievement, and improved general health. Parents are more nurturing, and both children and parents have less mental illness. Fewer children are taken from their parents, families are more cohesive, and schools become better educational environments (
8–
13,
23–
34,
57).
Common risk factors
Addressing broader public and social risk factors provides another approach to prevent mental, emotional, and behavioral disorders. For example, poverty often entails “a range of material hardships, such as overcrowding, frequent moves (which often mean changes of school), poor schools, limited health care, unsafe and stressful environments, and sometimes lack of adequate food” (
1).
The IOM report strongly endorses the idea that poverty is a potent risk factor for many emotional and behavioral disturbances. It also endorses the position that poverty must be addressed: “One factor lurks in the background of every discussion of the risks for mental, emotional, and behavioral disorders and antisocial behavior: poverty. • Although not the focus of this report, there is evidence that changes in social policy that reduce exposure to these risks are at least as important for preventing mental, emotional and behavioral disorders in young people as other preventive interventions. We are persuaded that the future mental health of the nation depends crucially on how, collectively, the costly legacy of poverty is dealt with” (
1). Collective action on social and economic policies directed toward poverty and other common risk factors, such as exposure to violence, social isolation, and discrimination, is as important as other measures to the prevention of mental disorders.
Recommendations
We have two sets of recommendations—one for the individual psychiatrist and mental health clinician and the other for the mental health system.
For the mental health clinician
Our main recommendation for psychiatrists and practicing mental health clinicians is to think and act more preventively (see the box on this page for specific recommendations).
Some approaches can be conducted in an office. For example, mental health clinicians can run groups for adolescents displaying subsyndromal depressive symptoms to prevent the onset of depression. Family sessions can be offered for depressed parents and their children without depressive symptoms (
34,
35,
43). Supporting parenting skills and treating depressive symptoms of parents to remission can prevent mental illness for their children (
63).
Mental health promotion should also be incorporated as a part of an individual's development. Encouraging a child to explore an interest in the piano may have a positive effect on mental health by developing competency and self-efficacy. Such a health promotion approach makes sense in any individual or group intervention (
64).
Because health promotion and prevention require action before the onset of illness, many intervention efforts occur outside of traditional health care agencies. Accordingly, psychiatrists can promote preventive examples in settings such as homes, schools, and community organizations.
Mental health professionals should support the parenting programs discussed previously for their many improved mental health and substance abuse outcomes. Children whose mothers were visited by nurses in home visitation programs showed more cognitive and social-emotional competence and were less likely to become involved in the juvenile justice system (
65). These nurse home visitation programs received $1.5 billion in the recent health care reform legislation (Patient Protection and Affordable Care Act) and deserve further advocacy and implementation support for their beneficial mental health outcomes.
Even the preliminary evidence that omega-3 fatty acids are neuroprotective (
66) and preventive of psychosis, with few major side effects (
67), can be a preventive nutritional recommendation in settings such as public school systems. Such evidence highlights the systemic need for further clinical and implementation research into preventive practices.
For the mental health system
As emphasized in the IOM report, the two central systemic recommendations are first, to make healthy mental, emotional, and behavioral development a national priority, and second, to coordinate and integrate prevention approaches across all federal and state agencies.
With the recent health care reform law, the National Prevention, Health Promotion, and Public Health Council has been created to better support preventive efforts. This council, whose establishment was recommended in the IOM report, has the potential to create more visibility for preventive efforts. Mental health advocates need to ensure that this council will include equal representation for the prevention of mental, emotional, and behavioral disorders.
The second recommendation is to coordinate prevention research and implementation efforts. The new council mentioned above should coordinate the interdisciplinary efforts of the Departments of Health and Human Services, Justice, and Education toward a comprehensive federal strategy to promote mental health and prevent mental, emotional, and behavioral disorders.
Similarly, states and communities need to develop a networked system for funding and coordinating prevention efforts. One idea is to dedicate funding in mental health block grants for prevention efforts, much as substance abuse block grants set aside funding for substance abuse prevention. Another strategy is “braided” implementation and research funding, which pairs funding for research with funding for implementation of preventive programs.
In addition, the National Institute of Mental Health should develop a comprehensive, long-term, preventive research plan. Research should emphasize programs with multiple beneficial outcomes, such as parenting programs and programs that show promise for high-prevalence disorders such as depression and anxiety. More research is also needed on effective implementation and dissemination strategies, including ways to effectively adapt interventions to different cultural backgrounds.
Envisioning the future
The scientific evidence for the prevention of mental, emotional, and behavioral disorders allows us to envision a better future. Imagine what our society, our schools, our communities, and our health care system would be like if organized by these preventive principles (see box on this page).
If we follow these preventive principles of promoting mental health and intervening early, our children and families would be supported in developing the skills they need to create happy lives free from mental illness. Our society could dedicate more of its resources to create vibrant schools, neighborhoods, and health care facilities. Our schools could promote appropriate developmental, self-efficacy, and communication skills. Our policies could address the common ills of poverty, violence, discrimination, and social isolation.
“The scientific foundation has been created for the nation to create a society in which young people arrive at adulthood with the skills, interests, assets, and health habits needed to live healthy, happy, and productive lives in caring relationships with others. This movement can be guided by a vision of a well-organized system of organizations, programs, and policies to ensure strong families and schools and nurturing neighborhoods” (
1).
The foundation is established; will we prioritize continued research and infrastructure? The evidence is here; will we practice its interventions? Prevention is possible—let's make it real.
Acknowledgments and disclosures
The authors thank A. Kathryn Power, M.Ed., of the Substance Abuse and Mental Health Services Administration and the members of the Institute of Medicine Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth and Young Adults: Research Advances and Promising Interventions.
The authors report no competing interests.