Day hospitals have had a long and checkered history in psychiatry. In many Western countries they were widely established as part of mental health care reforms beginning in the 1970s (
1–
3). Yet the term “day hospital” has been used for very different types of day services, ranging from drop-in facilities for long-term care to settings for crisis interventions (
4). Research provided little evidence for the effectiveness of long-term facilities, such as day-care centers providing ongoing vocational activities, and over time such services were challenged and frequently disappeared. At the same time, substantial research evidence suggests that day hospitals providing acute treatment as an alternative to conventional inpatient care may be effective. Systematic reviews and meta-analyses showed that treatment in acute day hospitals leads to symptom reductions similar to those achieved on conventional wards, that it may have more favorable outcomes in terms of patients' social functioning, and that it is often less costly than care on conventional wards (
5–
7).
Supported by this evidence base, day hospitals for acute treatment have been recommended by the National Institute for Clinical Excellence in the United Kingdom and have become a regular part of mental health service provision in other countries, such as Germany (
8,
9). However, day hospitals are not meant to replace conventional inpatient care completely, and they commonly exist alongside conventional ward settings. Thus, where day hospitals for acute treatment exist, clinicians have the option of admitting patients in need of acute treatment either to a day hospital or to a conventional hospital ward. Currently, there is no research evidence to guide decisions about which patients should be admitted to which setting.
In this study we explored whether patient baseline characteristics predict more favorable outcomes after treatment in either setting in order to provide information for more targeted admissions. Addressing this question requires a multivariate analysis of individual patient data that cannot be conducted in meta-analyses (
10). We utilized data from the European Day Hospital Evaluation (EDEN) study, a large randomized controlled trial that compared acute treatment in day hospitals and conventional inpatient wards in five European countries. EDEN assessed patients' psychopathology, social disability, and subjective quality of life as main outcomes over a one-year follow-up period. Consistent with other studies, EDEN found no difference between the two settings in the effectiveness of acute treatment for symptoms and subjective quality of life; however, patients' social disabilities were reduced after day hospital treatment (
11).
Several randomized controlled trials have compared outcomes in day hospitals and inpatient wards, and some of them systematically followed patients for at least six months (
4–
7). Of all patients included in these trials, the EDEN study included approximately 55% of the patients for whom psychopathology outcomes were reported, 71% of those for whom social functioning and disability outcomes were reported, and 100% of those with outcomes reported on subjective quality of life. The EDEN study therefore allowed us to address the research question in an analysis that used most of the patient data available in the world literature. Another advantage of using the EDEN data is that all patient characteristics and outcomes were assessed with identical instruments; thus there was no need to transform data, and the variance of the data for each individual could be fully utilized. We explored whether baseline characteristics of patients predicted a better response in either of the two settings. As potential predictor variables, we selected patient characteristics that may be assumed to be associated with a more or less positive response to day hospital treatment than to conventional inpatient care and that are available before admission: patients' age, gender, level of education, living status (alone or not), main psychiatric diagnosis, and symptom levels at admission. We tested whether these variables showed an interaction effect with the setting of acute treatment in predicting outcomes over one year in symptom levels, social disability, and subjective quality of life.
Methods
Study design
This exploratory study analyzed data from the EDEN study, a trial that compared acute day hospital treatment with conventional inpatient treatment that was conducted in 2000–2003 in centers in five European countries (Prague, Czech Republic; Dresden, Germany; Wroclaw, Poland; Michalovce, Slovakia; and London, United Kingdom). Details of the study methods, recruitment and patient flow, quality assurance measures for the randomization process, and main results have been described elsewhere (
6,
11–
16).
Sample
All patients aged 18 to 65 who were in need of acute treatment in a psychiatric facility in one of the five centers during the study period were eligible to participate in the EDEN study. Exclusion criteria were admission only for diagnostic purposes, involuntary admission, likely requirement of coercive measures or consistent one-to-one observation, acute intoxication, a somatic disorder requiring inpatient care, direct referral from another hospital, homelessness, a one-way journey to the day hospital of more than 60 minutes or the need to be accompanied on the way to the day hospital, incapacity to give informed consent, or refusal to participate. Study participants were randomly assigned to acute treatment either in a day hospital or on a conventional inpatient ward. After complete description of the study, written informed consent was obtained from participants. Detailed written protocols of local procedures and clinical responsibilities were established at each center and approved by local ethics committees.
A total of 1,504 eligible patients were asked to participate. Of those, 1,055 patients (70%) were included in the final EDEN analysis of effectiveness. Because we aimed to have large but relatively clear-cut diagnostic categories as potential predictor variables in the study reported here, we further excluded patients with infrequent or unclear diagnoses. We therefore excluded patients with a main clinical diagnosis of an organic mental disorder (ICD-10 codes F00–F09, N=34), mental and behavioral disorders due to psychoactive substance use (codes F10–F19, N=19), and disorders of adult personality and behavior (codes F60–F69, N=89), as well as patients with an unclear diagnosis (N=33). Thus the final study sample comprised 880 patients, 454 of whom had been assigned to acute day hospital treatment and 426 to conventional ward treatment. In line with clinical practice at participating centers, clinical diagnoses were made on the basis of the ICD-10 classification system.
Outcome measures
For this analysis we used the three main outcome criteria of the EDEN study—psychopathology, social disability, and subjective quality of life—which were assessed at discharge and at three and 12 months after discharge. These were the outcomes analyzed in previous studies of the differences between the two settings.
Psychopathology was assessed with the 24-item version (version 4.0) of the Brief Psychiatric Rating Scale (BPRS) (
17,
18). The interrater reliability achieved in the training of researchers in the study was high (intraclass correlation coefficient [ICC]=.78). Social disability was observer rated on the Groningen Social Disability Schedule, second revision (GSDS) (
19). On the GSDS, disabilities are rated in nine social roles, with different dimensions for each role and a sum score based on overall ratings. The interrater reliability for the sum score was also high (ICC=.77).
As a patient-reported outcome, subjective quality of life was assessed on the Manchester Short Assessment of Quality of Life (MANSA) (
20). The MANSA contains 12 items on satisfaction with life in general and with various life domains, which are rated on a scale from 1, couldn't be worse, to 7, couldn't be better. The mean score on the satisfaction items was taken as a measure of subjective quality of life.
Predictor variables
Predictor variables were the center (location) and patients' age, gender, years of education, length of hospital stay, living status (alone versus with someone), baseline symptom levels (total BPRS score as assessed before randomization), and the main ICD-10 psychiatric diagnosis. Because a complete standardized diagnostic interview with all patients was impracticable before admission, we used the clinical discharge diagnosis in all cases. Main diagnoses were analyzed in three categories: schizophrenia, schizotypal, and delusional disorders (ICD codes F20–29); mood disorders (ICDcodes F30–39); and neurotic, stress-related, and somatoform disorders and behavioral syndromes associated with physiological disturbances and physical factors (ICD codes F40–59).
Procedure
Predictor variables other than clinical diagnosis were assessed by a researcher before randomization. Outcomes were assessed by an independent researcher at discharge and at three- and 12-month follow-ups after discharge. Researchers were not involved in patients' treatment; however, the treatment setting could not be masked because patients had to be interviewed in the given treatment setting at discharge.
Statistical analysis
The three outcome variables (BPRS, GSDS, and MANSA scores) were analyzed separately by a mixed-effects model to take account of repeated measurements of these outcomes during the follow-up. In this model, the baseline measurement of the given outcome, the treatment setting, the time points of the measurement, and the selected baseline characteristics of patients were introduced as fixed effects, and a random effect was included for patients. The number of patients for whom data on variables tested as predictors were missing was relatively small (ten for living situation, 50 for years of education, and one for length of hospital stay). These missing values were imputed by using their given distributions at baseline. During the trial, some patients dropped out, which resulted in incomplete observations for a given outcome variable. These patients were included in the analysis, and the incomplete observations were assumed to be missing at random in the mixed-effects model analysis.
The analysis was conducted in two steps. First, we estimated a main-effect model with all baseline predictors. In the second step, the first-order interactions between treatment setting and each of the selected baseline variables were added to the main-effect model one by one if the interaction was significant at p<.05. The final models contained all baseline variables and significant interactions of baseline variables with treatment setting. We present the regression coefficients, their 95% confidence intervals (CIs), and p values for the main-effect model and for the model that includes the significant interactions.
An interaction effect between setting and a baseline variable means that the treatment effect depended on this variable or that the effect of this variable depended on the setting. The magnitude and statistical significance of interaction effects were taken from the final models. All statistical analyses were conducted with the Statistical Analysis System (SAS), version 9.1 (
21).
Results
The baseline characteristics of the sample that were tested as predictor variables are summarized in
Table 1.
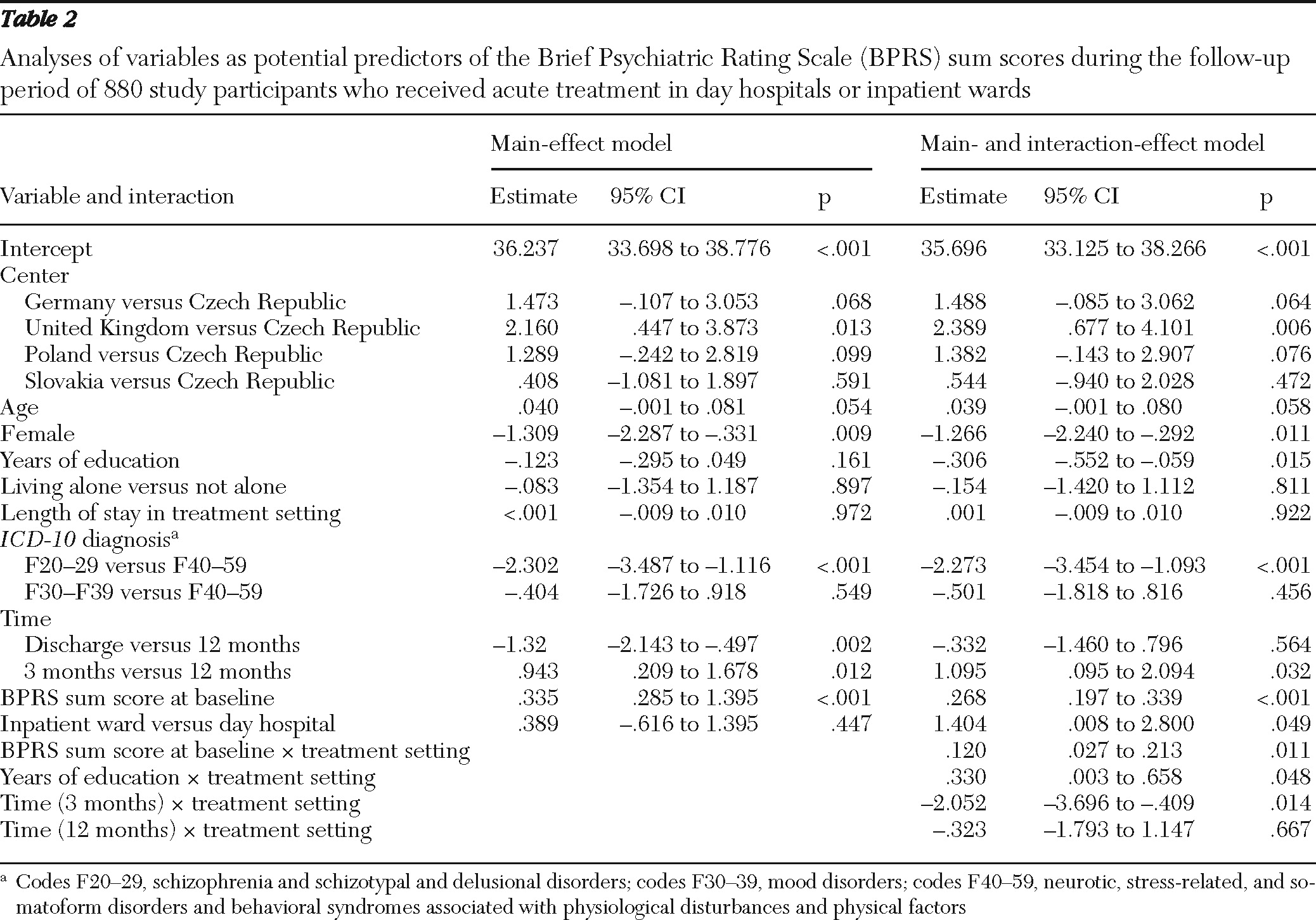
Table 2 presents the results of the mixed-effects model analysis of BPRS score. Several variables were found to predict outcomes in both settings, but for the research question addressed in this study only the interaction effects were of interest. Significant interaction effects in the prediction of symptoms were found between baseline variables and time and the treatment setting. Baseline symptom levels and years of education each interacted with the treatment setting in predicting symptom levels during the follow-up period.
The direction of the interactions were as follows: higher levels of baseline symptoms were linked with greater symptom improvement in both settings, but this association was significantly stronger for treatment in a conventional inpatient setting (ward, coefficient=.394, CI=.328–.460; day hospital, coefficient=.263, CI=.192–.335).
The interaction between education and symptoms suggested that the effect of education on BPRS score differed between day hospitals and wards. The effect (that is, that more years of education predicted more favorable symptom change) was statistically significant in day hospitals (coefficient=−.306, CI=−.552 to −.059) but not significant on conventional wards. The negative value means that BPRS score was negatively associated with increased years of education in day hospital treatment—that is, patients with more years of education experienced greater symptom reduction after day hospital treatment. In addition, the difference between ward and day settings in symptom improvement was significant only at 12 months (coefficient=1.427, CI=.477–2.377).
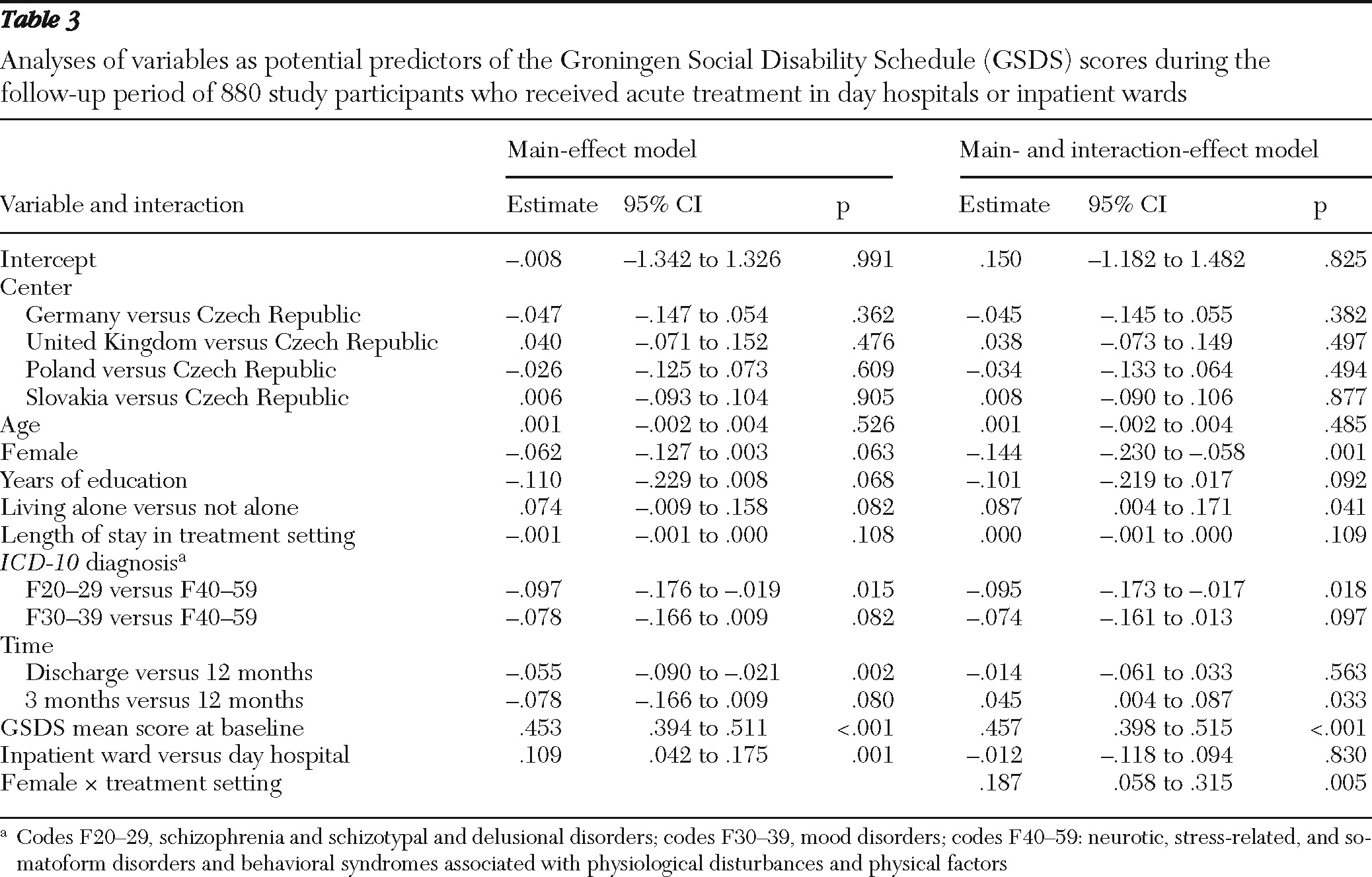
Results of the mixed-effects model analysis of GSDS score are shown in
Table 3. Findings on the interaction effect for GSDS score suggested that the treatment difference in GSDS score between ward and day hospital was significant only for female patients (coefficient=.175, CI=.095–.256) but not for male patients (coefficient=−.012, CI=−.118 to .094).
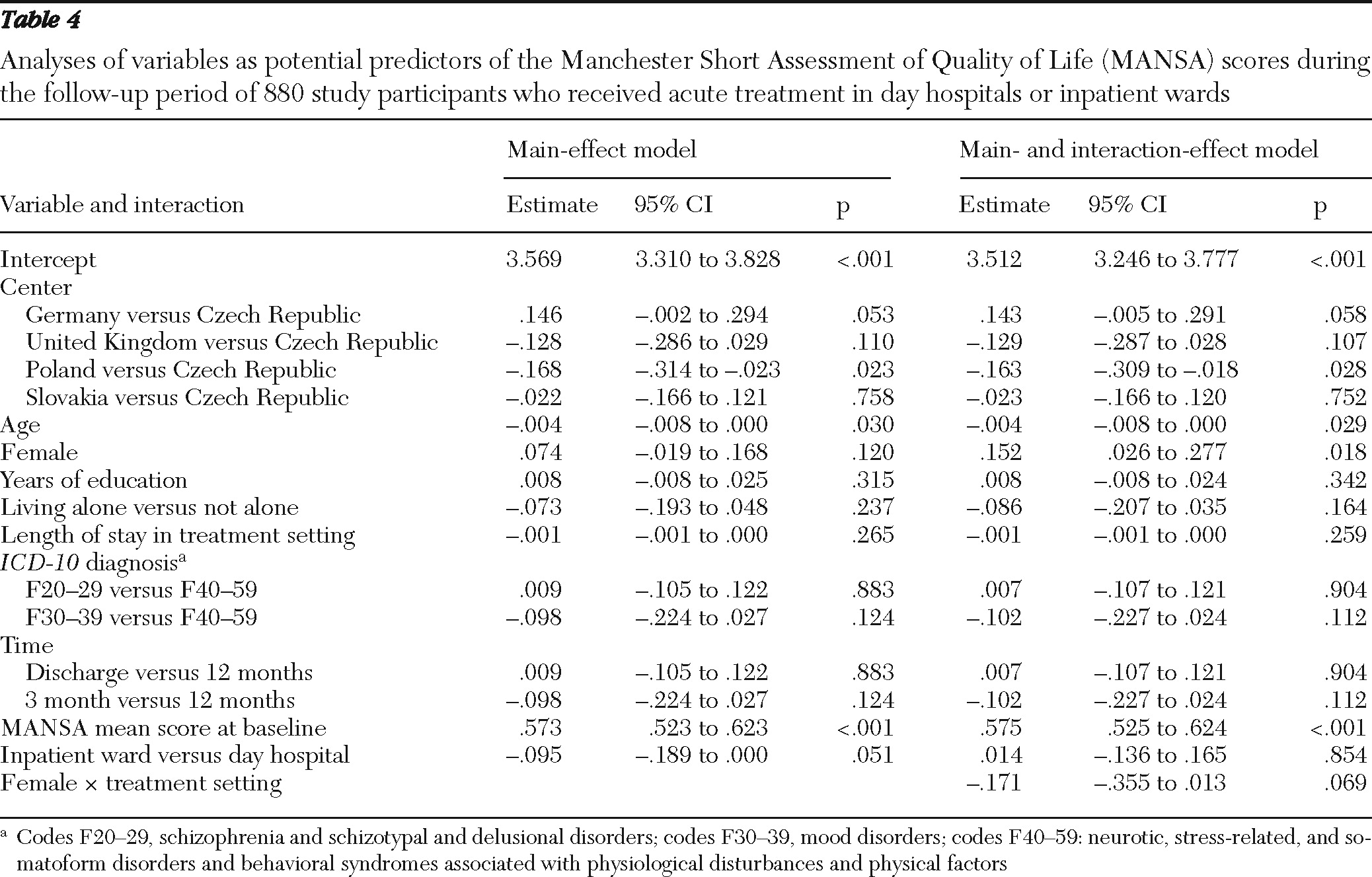
Finally,
Table 4 shows the results of the mixed-effects model analysis of MANSA score. Because no significant interaction effect was found between treatment setting and any of the patient baseline characteristics, only results from the main-effect model are presented.
Discussion
Main findings
The study identified patient characteristics that can be easily assessed in an acute situation and can predict whether patients may benefit more from treatment in day hospitals or on conventional hospital wards. Higher baseline symptom levels were more strongly associated with symptom improvements after treatment on a conventional ward, and more years of education were associated with greater symptom reduction after day hospital treatment. Female patients had more favorable social disability outcomes after day hospital treatment, whereas no difference between the two settings was found for male patients.
Thus patients with higher symptom levels might benefit more from acute treatment on conventional wards, and female patients and patients with more years of education may show more favorable outcomes in day hospitals. Patients' age, diagnostic category, and living status did not predict differences in outcomes between day hospitals and wards.
Strengths and limitations
This analysis used data from a very large and rigorous randomized controlled trial that included between 55% and 100% of the data that are relevant to the research question and that are available in the world literature. In the multivariate analysis we used full individual data without transformation and controlled for main effects, including possible effects of the treatment center that may have been attributable to the heterogeneity of national health care systems in the five countries or to other local factors.
However, the study also had some limitations. The data are from centers in five European countries, and although the findings were adjusted for a potential center effect, the findings may have been influenced by the varying context at the five study sites. Various potentially important predictor variables, such as patient preference and social networks, were not assessed, and we tested only a small number of potential predictor variables. We used rather crude diagnostic categories, and the diagnoses were clinical and not research diagnoses based on standardized instruments. Studies using more precise and specific diagnostic groups might reveal differences in outcomes between the two settings that were not identified in this study. Data are from a trial with strict inclusion criteria, and the findings may not apply to groups that were excluded, such as homeless patients. Also, the study was exploratory, and the results need to be confirmed in further hypothesis-driven research.
Relevance of predictor variables
Patients with higher symptom levels appeared to respond better to treatment on a conventional ward. They might especially benefit from the more containing and structured environment of a ward and from supervision of their medication adherence, which may be more intensive on a ward than in a day hospital.
Female patients and those with more years of education benefited more from day hospital treatment. We can only speculate about the reasons because potentially mediating processes were not assessed in the study. Both groups may engage better with the treatment approach of day hospitals, which can be very different from conventional inpatient treatment. Commonly, day hospitals provide more activities and discussions in groups, require more patient involvement, and leave more autonomy to the patients, who return home every evening. This may appeal more to women and patients with higher education levels, who at the same time might struggle to cope with the restrictions and tensions that often characterize the atmosphere on acute wards (
24,
25). Better engagement during acute treatment may have led to more positive outcomes over the one-year follow-up.
Women had better outcomes in regard to social disabilities after day hospital treatment. Compared with wards, day hospitals usually provide more social activities and have a stronger focus on verbal interactions and functioning in groups (
4,
25). Such a setting may facilitate more positive learning processes among female patients and enable them to acquire confidence and skills to improve their functioning in different social roles after treatment.
The study did not find evidence for the importance of the other tested predictor variables, although their clinical relevance could be hypothesized. For example, it may have been assumed that patients with diagnoses of schizophrenia might benefit more from the structured atmosphere on wards, that the 24-hour provision of care on wards is better for people who live alone, and that the more flexible and less tense setting in day hospitals would be more therapeutic for older patients and those with depressive disorders. However, when the analysis controlled for other relevant factors, these variables did not show significant interaction effects with treatment setting in predicting outcomes.
Conclusions
The findings suggest that targeted referrals to acute treatment in day hospitals and conventional wards are possible. The associations found are not very strong and are based on multivariate analyses that controlled for various other factors. Thus the predictor variables will not override other important clinical considerations that may favor admission to one of the two settings for a given patient. However, in the absence of other criteria—and all other things, including patient preference, being equal—they are factors to be considered when deciding on the most appropriate setting for acute treatment: higher symptom levels can be seen as a reason to admit a patient to a ward, and female gender and higher education may be seen as reasons to admit a patient to a day hospital (
25–
27).
These results were found in a study that randomly assigned patients to the two settings without regard to symptom level, gender, or education. If the findings lead to more targeted admissions, day hospitals may end up with more patients who have lower baseline symptoms, are female, and have a higher level of education, whereas patients who are male, have more baseline symptoms, and less education may be concentrated on wards. Such a result may affect the therapeutic atmosphere in the two settings, which may or may not be welcome and which may eventually change the associations found in this study.
Future research should explore qualitatively and quantitatively the processes behind the associations found here and identify specific treatment methods and patient experiences that explain the different outcomes. Baseline symptoms, gender, and education levels need to be controlled for in trials, and these characteristics may be used to stratify samples that are allocated to different settings of acute treatment.
Acknowledgments and disclosures
The study was funded by grant QLG4-CT-2000-01700 from the European Commission. Additional national funds were received from the Roland-Ernst Foundation for Health Services (Germany), the National Health Service Executive Organsiation and Management Programme (United Kingdom), the National Committee of Scientific Affairs (Poland), and the Ministry of Education (Slovakia). Pfizer supported travel and accommodation for project meetings.
The authors report no competing interests.