Residents in long-term care homes (nursing homes) have a high prevalence of dementia and behavioral symptoms, according to previous research (
1). Common mental health issues include major depression (
2) and complications from dementia, such as agitation and aggression (
3). The magnitude of these problems was explored in a systematic way by Brodaty and colleagues (
3), who attempted to quantify the prevalence of behavioral and psychological symptoms in dementia among residents in a nursing home in Sydney, Australia. The study concluded that over 90% of residents exhibited at least one symptom of dementia, with depressed mood, psychosis, and aggression being the most common symptoms expressed.
Although many programs have been put in place to address the psychogeriatric needs of residents within long-term care, few published studies have attempted to evaluate systematically the effectiveness of these programs. Draper and Low (
4) conducted a systematic review of psychogeriatric consultation to long-term care homes. They described four studies (
5–
8), only one of which was a randomized controlled trial (
7). Three of the four studies involved providing education and training to staff in addition to enhancing activity levels of residents and providing expert consultation (
5–
7). Measurable benefits in behavior were noted in only one study, which found that specialty consultation was associated with reduced frequency of medication use and hospitalization (
5). A fourth study (
8) looked at weekly consultation by a nurse and psychiatrist, and although it found no measurable behavioral effects, it did find reduced medication usage, fewer hospital admissions, and fewer general practitioner visits.
This study focused on the impact of developing and implementing a model of specialized psychogeriatric consultation in long-term care homes in the region of Toronto, a large metropolitan city located in Ontario, Canada. Long-term care homes in the region of Toronto serve patients with the highest needs and as such are distinct from retirement homes and assisted-living facilities. Before 2005 psychogeriatric services in long-term care homes in the city of Toronto were provided on an as-needed basis, with no formal systems in place. Some homes were supported by community teams, some by allied health personnel, and some by independent psychiatrists. In the absence of formalized services, patients often would be transferred to emergency departments or acute care when their mental status decompensated, resulting in increased expense. In 2005 Federal Health Accord Funds became available to the province of Ontario, and psychogeriatric services in long-term care were identified as a priority. A committee was developed that comprised representatives from health care, local government, and long-term care and was charged with the task of developing and implementing a model of specialized consultation to long-term care.
It was determined that funding would be used to augment existing services and create new specialized consultation teams where needed. All teams would be assigned a specific quota of long-term care homes so that all homes would have equal access to specialty teams. In the model described, teams consist at minimum of a psychiatrist and an allied health team member, who is usually a nurse. All teams are affiliated with hospitals, and patients with significant agitation are given priority. Most teams make five visits per day or 20 per week. In total, 13 teams were assigned to provide service to 84 homes (five existing teams, five newly funded teams, and three teams with enhanced funding). Most teams were operational by September 2006, and this evaluation was undertaken in the fall of 2007.
Methods
The study was retrospective in design. Surveys were administered to teams and long-term care homes, and retrospective data were extracted from team charts. Teams and homes were invited by e-mail to complete an online survey designed to assess satisfaction. Retrospective patient data were collected from team charts by a trained research assistant. The chart review of the patient population encompassed all new consultations from long-term care homes to teams within a four-month period (March 1, 2007, to June 30, 2007). A maximum of ten charts were selected from each team according to a predetermined protocol that minimized the variation between long-term care homes. Chart data were collected from the time of the initial assessment until the last documented note. To ensure data accuracy, we spot-checked data collected from team charts. Consent for the study protocol was sought and obtained from individual research ethics boards within each of the 11 hospitals in which the 13 teams were based (three teams were based at one institution) by using the Harmonized University of Toronto ethics application form. Note that the requirement for individual informed consent was waived by the research ethics board because this study entailed retrospective chart review only and reporting of only aggregated data results.
Results
All 13 teams (100%) responded to the team survey. Approximately half of the teams (N=6, 46%) were community based, and the rest were affiliated with academic centers. On average, most teams consisted of one full-time nurse and a half-time psychiatrist, social worker, or occupational therapist. All teams used standardized scales, although not all teams used the same ones, and 77% kept their own charts, separate from the homes' charts. Aggregated responses from teams indicated that 96% of homes (N=81) were utilizing their services and agreed that referrals were appropriate. They reported that their pharmacological recommendations were implemented by the long-term care home 76% of the time, whereas nonpharmacological recommendations were implemented only 55% of the time. On average patients were seen within two weeks of referral. Teams felt that the system could be best enhanced by adding beds for patients with behavioral problems and by reducing staff-to-patient ratios.
Forty of 84 eligible long-term care homes (48%) responded to the survey. The homes varied considerably in size, with about a third having fewer than 100 beds, a third having 100–200 beds, and a third having more than 200. Ninety percent (N=36) of long-term care homes that responded to the survey indicated that behavioral issues were a problem among their residents, with over one-third (38%, N=15) identifying behavioral issues as a major problem. Most long-term care homes that responded (80%, N=32) reported that they were using their teams regularly—twice a month or more. Eighty percent (N=32) were satisfied with both the timeliness of the consultation (90%, N=36) and the quality of the consultation (88%, N=35). Whereas responses from most homes indicated that the addition of teams and the assignment of teams to homes helped homes deal with disruptive residents (88%, N=35), a much smaller percentage (50%, N=20) indicated that these additions made homes better able to accommodate residents with significant behavioral issues. Long-term care homes generally agreed with teams that the two most important funding priorities were to increase frontline workers and to improve access to tertiary behavioral beds.
Patient chart review data were collected from 12 of the 13 teams and comprised 88 patient consults from a total of 48 long-term care homes. Only nine of the 12 participating teams were able to provide full population consultation data for the four-month study period. Fourteen of the 57 homes (25%) covered by these nine teams had no referrals during this period.
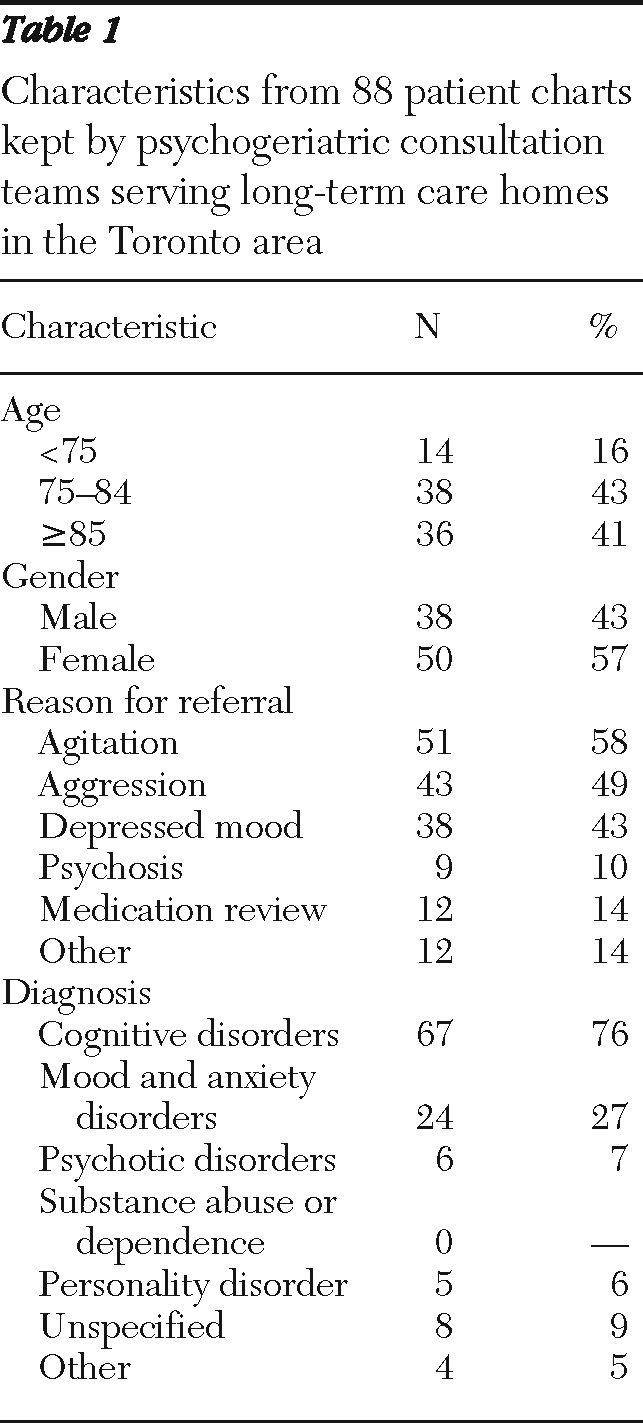
According to chart review findings, 41% of patients referred for assessment were aged 85 or older, and most were women (57%) (
Table 1). Approximately 90% of patients were referred for depressed mood, agitation, or aggression, with only a few being referred for other reasons, such as personality change or cognitive decline. There was wide variation in wait times, with 26% of the patients (N=23) assessed more than two weeks after the initial assessment. Most patients (61%, N=54) saw two types of professionals over the course of the full consultation (a psychiatrist and an allied health professional, most commonly a nurse).
Clinical, nonpharmacological recommendations arising from the assessment consisted mainly of modifications to the existing care routines (61%, N=54) or the acquisition of additional in-house support (42%, N=37); in almost a third of cases, recommendations included referrals to additional outside services (30%, N=26). Pharmacological recommendations were also common (68%, N=60) and consisted mainly of the initiation of new medications or dosage adjustments. Verbal and physical assaults over the course of the consultation were documented in approximately one-third of cases; however, very few situations resulted in hospitalization. A large proportion of patients (57%, N=50) remained in care at the end of the review period, although a high percentage of patients (27%, N=24) were stabilized and discharged from team care.
Discussion
The aim of the study was to determine the impact of implementing a new model of specialized psychogeriatric consultation to long-term care homes in a large metropolitan city. Previous research focusing on the needs of staff in long-term care homes has highlighted the need for access to high-quality mental health services (
9). As a result of the team intervention, 88% of homes that responded to the survey indicated that they were better equipped to manage the patients' needs and behaviors, whereas only 50% suggested that they were more able to accept residents with psychiatric and behavioral issues. Although individual patient outcome data were not part of this study, our findings suggest some beneficial effects of psychogeriatric consultation, in keeping with previous studies (
4).
Although only 48% of long-term care homes responded to the survey, most homes that responded were satisfied with the quality of the consultations, their timeliness, and the relationship of outreach staff to long-term care staff. Another positive indicator was that homes appeared to be using the teams. According to responses to the team survey, 96% of the homes were using the teams, and according to the responses to the long-term care home survey, 80% of the homes that responded made more than one consultation per month. Furthermore, although pharmacological recommendations were implemented in 76% of cases, nonpharmacological recommendations, which are by nature more difficult to implement, were also implemented in 55% of cases, according to the responses to the team survey.
Given what is known about the demographic characteristics of long-term care homes, it is not surprising that patients tended to be quite elderly and that most were women. However, we found it somewhat surprising that more women were not referred, given that the proportion of women is much higher than that of men in long-term care homes in Ontario (75% versus 25%). This discrepancy might suggest that men, although making up a smaller percentage of long-term care residents, may tend to have more psychiatric issues than women or more issues that require consultation, such as agitation, aggression, and so on. Agitation, aggression, and depression were the most common reasons for referral. This finding conflicts somewhat with previous studies in this area (
10), which suggest that behavioral problems and agitation more commonly than depression result in referral, perhaps because depressive symptoms tend to cause less distress to staff.
This study has a number of limitations. First, conclusions are based on responses to survey questions, and it is possible that such responses were biased. For example, the extent to which homes used teams varied considerably, depending on whether the information was taken from the survey or patient chart review. Second, only the team charts were reviewed, and charts within the homes were not, so it is possible that documented information was not entirely accurate or may have been biased. Finally, the study took place shortly after the teams were implemented, so the conclusions may be somewhat premature.
Conclusions
Nevertheless, the preliminary conclusions of the study are encouraging. The surveys suggest that both specialized consultation teams and long-term care homes were satisfied with each other, which is the basis of a very good working relationship. Utilization of teams, although not 100%, is encouraging, especially because the teams were just recently implemented. The diagnostic profile of patients referred appears appropriate, and the use of combined approaches to care (pharmacological and nonpharmacological) is especially encouraging. It is clear from recommendations provided by teams and homes that although teams play an important role, there are other important interventions, such as increased access to specialty beds and improved staff-to-resident ratios, that may need to be implemented before the full impact of these teams can be realized. Future funding and research should focus on addressing these system issues in order to further enhance patient care and improve treatment outcomes.
Acknowledgments and disclosures
This study was made possible through funding supplied by the Ministry of Health and Long Term Care, Province of Ontario. This study in no way reflects the opinions or views of the Ministry of Health and Long Term Care.
The authors report no competing interests.