For many low-income parents, primary care and family medicine practices are the main sources of psychiatric treatment for depression. Numerous studies have shown that children of depressed parents are significantly more likely than children of parents without depression to experience psychiatric disorders (
1,
2) and to have less favorable treatment outcomes (
3). Increasing evidence suggests that providing effective treatment for depressed parents is associated with a positive impact on child psychopathology and functioning (
4). Weissman and colleagues (
5) found that successful medication treatment of maternal depression was associated with reductions in children's diagnoses and symptoms three months after remission, whereas nonremission of maternal depression was associated with poorer child outcomes. Low-income, single, depressed mothers, however, tended to have the lowest rates of treatment retention and depression remission. Even when their depression remitted, their children tended to have the worst psychiatric outcomes (
6).
Given the lower retention and improvement rates among low-income, single, depressed parents and their children, treatment preferences and obstacles in these high-risk families need to be identified to facilitate the development of feasible and acceptable mental health services. Although these factors have been assessed among ethnically diverse, depressed primary care patients (
7,
8), no studies have focused specifically on depressed parents and their children. In addition, no studies have focused on subthreshold depression among parents attending primary care practices. This group is important to assess, because studies have found that subsyndromal depression is associated with later psychiatric disorders and clinical impairment (
9,
10). This report presents data from a systematic survey to assess treatment needs of parents with depression attending an urban family medicine practice primarily serving low-income, Hispanic families.
Methods
The survey was conducted at Columbia University's Center for Family and Community Medicine's Herman “Denny” Farrell, Jr., Community Health Center between January 2008 and January 2009. Approximately 10,000 patients attend this center annually. Patients are primarily Hispanic and on low income, approximately 70% of patients are female, and most patients are insured through Medicaid.
Eligible participants were aged 21 to 60, English or Spanish speaking, a parent of a child aged seven to 17 or a caregiver (that is, someone who lives with the child at least 50% of the time), and scheduled for an appointment; all had at least one prior visit to the center. Patients were excluded if they could not complete the survey.
The New York State Psychiatric Institute's Institutional Review Board approved this study. Informed, signed consent was obtained before participation. Fliers informing patients about the study were displayed in the waiting room. Patients were given a flier after signing in and, according to where they sat, were systematically approached to determine their eligibility. Overall, 3,216 patients were approached; 964 (30%) refused more information or did not complete the eligibility assessment. Of the 2,252 patients assessed, 1,616 (72%) were ineligible for at least one of the following reasons: not the parent or caregiver of a child aged seven to 17 who lived with the child at least 50% of the time (86%), not in the parental age range selected for the study (26%), not scheduled for an appointment (27%), and first visit to the center (13%). Two hundred forty-eight patients (11%) could not participate because they had previously completed the survey. Finally, 30 patients completed the survey more than once. We retained their first survey; 42 repeated surveys from 30 patients were removed.
Of 346 eligible parents, 282 (82%) provided written, informed consent. Four participants were excluded because they endorsed suicidal ideation. Five did not complete the study. Analyses are based on 273 of the 346 (79%) surveys.
Assessments were translated from English to Spanish and back-translated into English by bilingual staff. Participants completed the survey as an interview, self-report, or a combination, as requested. Demographic information was collected. The DSM-IV Primary Care Evaluation of Mental Disorders Patient Health Questionnaire was used to assess screening diagnoses of major depression, panic disorder, generalized anxiety disorder, and past-year alcohol use disorder. Past-year drug use disorders were assessed similarly. Participants received screening diagnoses of major depression if they endorsed five of nine symptoms (including depressed mood or anhedonia) for more than half the days or nearly every day of the preceding two weeks (if one of the five symptoms was suicidal ideation, it was included if it was present at any time during the two weeks). Subthreshold depression was defined as endorsement of two to four symptoms of depression for more than half the days or nearly every day of the two preceding weeks (including depressed mood or anhedonia) or more than five symptoms of depression for at least several days in the two preceding weeks (including depressed mood or anhedonia). Not having depression was defined as not meeting criteria for major or subthreshold depression. Social anxiety was assessed via the Mini-Social Phobia Inventory. Questions were included about lifetime and recent psychiatric treatment.
Participants were asked to indicate whether they wanted to receive help for a variety of described problems and to indicate their treatment preferences and obstacles to attending treatment by endorsing checklist items that were based on the National Comorbidity Survey-Replication. Participants were also asked to indicate whether their seven- to 17-year-old child or children had any of the listed internalizing or externalizing problems.
Descriptive statistics are presented for demographic and clinical characteristics. The sample was divided into three groups: participants with major depression, subthreshold depression, or no depression. These groups were compared on demographic and clinical variables with analysis of variance for continuous variables and chi square tests for categorical variables.
Chi square comparisons across the three groups were conducted for all outcome variables. When significant differences were found (p<.05, two-tailed), pairwise comparisons were conducted. The first pairwise comparisons assessed were between the major and subthreshold depression groups. These two groups were then consolidated into a combined depression group. Pairwise comparisons were conducted between the combined depression group and the group with no depression. For these pairwise comparisons, alpha was set at .01 (two-tailed). In addition, dichotomous variables were analyzed as dependent variables in binary logistic regressions, with dummy variables representing depression group status and potential demographic and diagnostic confounders simultaneously designated as independent variables. These results are presented as adjusted odds ratios with 95% confidence intervals.
Results
Most participants were women (N=237, 87%) and single (N=174, 64%). A total of 231 participants (85%) were Hispanic; 36 (13%) were non-Hispanic black; two (1%) were non-Hispanic white; and four (2%) were Asian, Pacific Islander, or other. A total of 158 parents (58%) completed the survey in Spanish. Overall, 152 parents (56%) reported making less than $12,000 a year.
The rate of current depression (major or subthreshold) was high (N=87, 32%); 24 (9%) met criteria for major depression, and 63 (23%) met criteria for subthreshold depression. A total of 107 (39%) met criteria for any mental or substance use disorder (including subthreshold depression). [A table with additional data on sample characteristics is available in an online appendix to this report at
ps.psychiatryonline.org.]
Gender, marital status, educational attainment, and household income were not significantly different across the three depression subgroups. However, the mean ages of the groups differed significantly: major depression, 45.1±8.4; subthreshold depression, 36.7±10.4; and no depression, 39.4±9.9 years (F=6.32, df=2 and 268, p=.002). Tukey B tests showed that parents with major depression were significantly older than parents in the other groups (t=2.99, df=269, p=.003).
No significant between-group differences were found in diagnoses of substance use disorders. The groups differed significantly in the frequency of anxiety disorders (χ2=70.34, df=2, p<.001). Compared with the group with no depression, the combined depression group had a significantly larger proportion of parents meeting criteria for any anxiety disorder (N=7, 4%, compared with N=39, 45%; χ2=68.30, df=1, p<.001). Parental age and any anxiety disorder were controlled for in the logistical regression analyses.
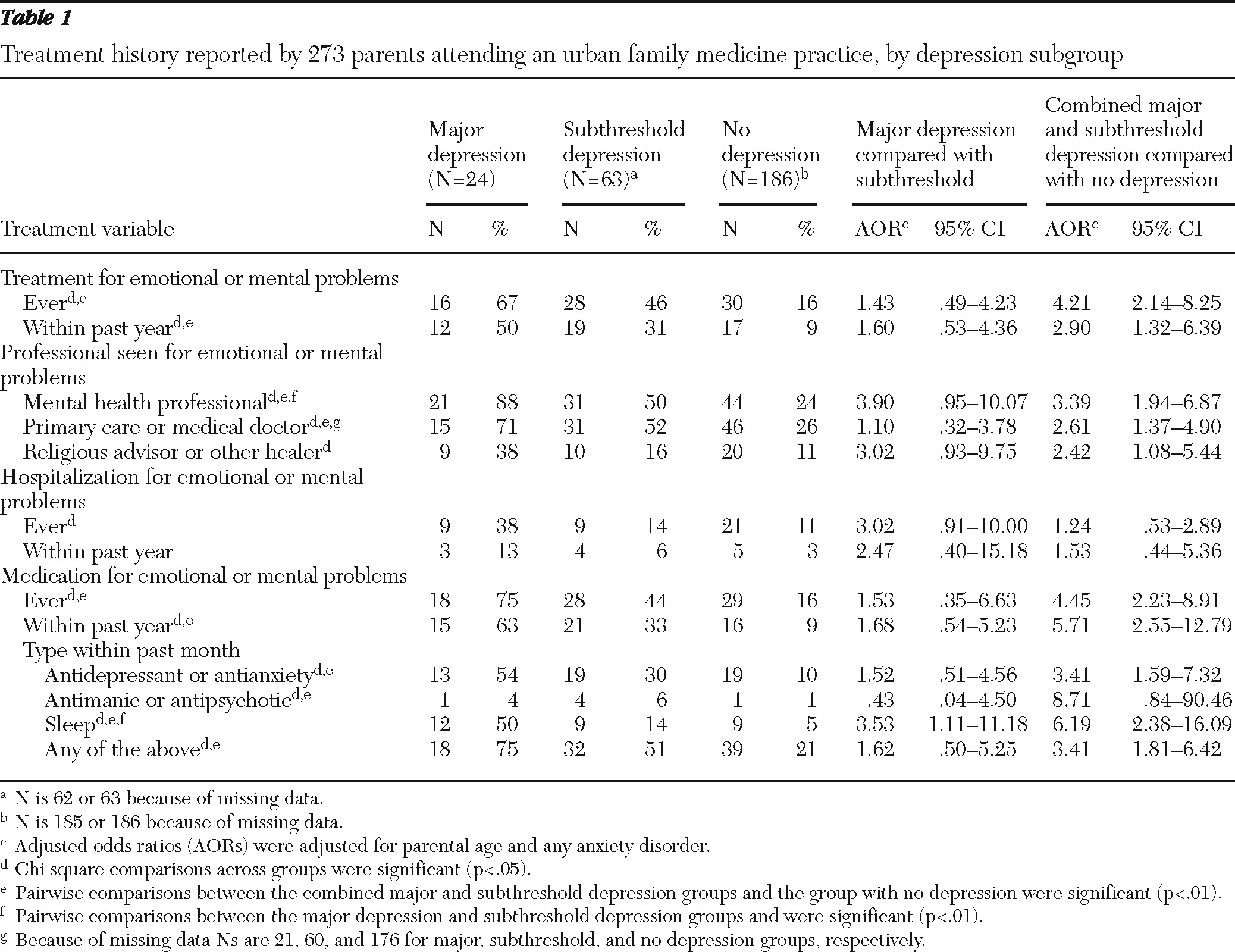
As shown in
Table 1, a larger proportion of the group with major depression (67%) reported a lifetime history of psychiatric treatment, compared with the subthreshold group (46%) and the group with no depression (16%). Few significant differences were found between the major depression and subthreshold groups; however, the adjusted odds of reporting a history of treatment were higher in the combined depression group than in the group with no depression for most variables.
In general, the major depression and subthreshold groups did not differ significantly in their interest in getting help, treatment preferences, treatment obstacles, or frequency of children's problems. However, the adjusted odds of being interested in help for several problems (for example, anxiety, sadness, and financial problems) were 2.05 to 6.66 times as high in the combined depression group as in the group with no depression, after controlling for parental age and any anxiety disorder. [A table in the online appendix at
ps.psychiatryonline.org presents detailed results on interest in getting help].
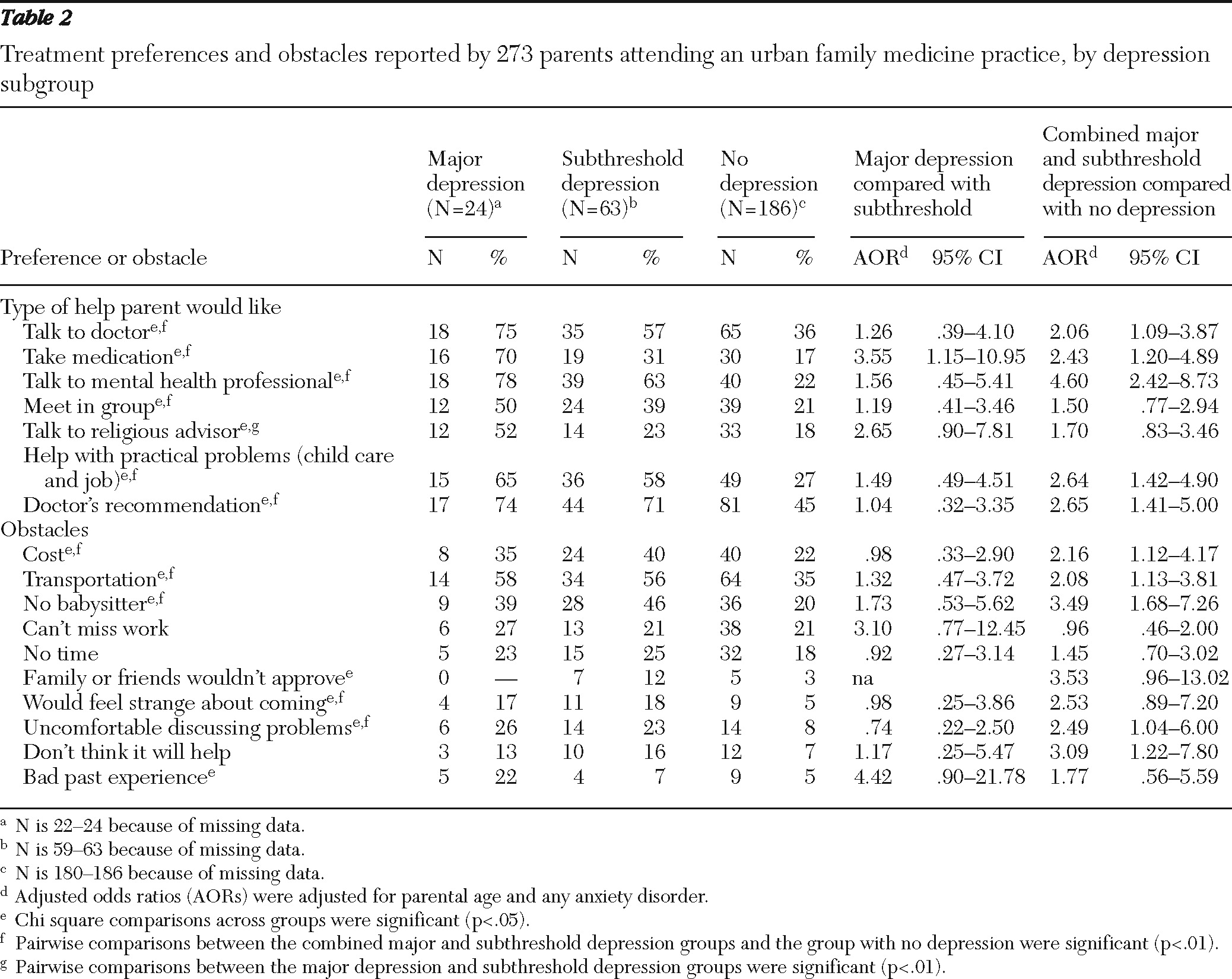
Results for treatment preferences and obstacles are shown in
Table 2. The adjusted odds of being interested in most types of help were 2.06 to 4.60 times as high in the combined depression group as in the group with no depression. Preferred treatment options included talking to their doctor or a mental health professional, taking medication, obtaining help with practical problems, and getting a doctor's recommendation. For many obstacles, the adjusted odds were 2.08 to 3.49 times as high in the combined depression group as in the group with no depression. Significant obstacles included treatment cost, transportation, child care, feeling uncomfortable discussing problems, and not thinking treatment will help.
The adjusted odds of reporting a child problem were 2.25 to 3.69 times as high in the combined depression group as in the group with no depression. The most prevalent child problems were losing his or her temper, being inattentive, and disobeying rules at home. [A table in the online appendix at
ps.psychiatryonline.org presents detailed results on child problems endorsed.]
Discussion
Results indicate that almost one-third of these predominantly low-income, Hispanic parents had either major or subthreshold depression. These parents reported high rates of past or current treatment and psychotropic medication. They also expressed interest in getting help for many current problems. Treatment preferences often involved interpersonal contact with professionals, and a large proportion wanted help with practical problems (such as child care and jobs). Given that many of the participants were in treatment and continued to report depressive symptoms, their desire for treatment beyond medication seems justifiable. Other research also indicates that depressed, Hispanic patients in primary care are likely to prefer psychotherapy over medication (
7). These findings are in sharp contrast to the current national trend of decreased use of psychotherapy in favor of antidepressant medication (
11). Psychotherapy is an important option to consider, particularly for parents with mild depression who experience functional impairment but do not benefit from medication (
12).
Depressed parents were significantly more likely than nondepressed parents to cite a number of practical obstacles and concerns about discussing problems. Solutions to practical problems, such as fee reimbursements and child care, seem most salient, as does a focus on engaging parents in discussions of their attitudes about help seeking. Depressed parents were also more likely than nondepressed parents to report children's problems, which is consistent with findings from numerous studies (
1,
2). Arranging for parents and children to see the same provider may enhance the opportunity for effective family intervention.
The study had several limitations. First, we did not collect information on reasons for attending the practice, such as medical problems that may have been related to depression. Second, many patients refused to be assessed for the study, and their eligibility is unknown. We also did not include parents with children younger than seven. Third, we utilized a screening self-report rather than a diagnostic interview. Fourth, checklists regarding treatment needs may not reflect actual concerns, which may be elicited with qualitative interviews. Fifth, direct interviews with children may have reduced potential biases in the reports of depressed parents. Sixth, we did not follow up with families to determine whether parents who reported interest in help actually sought services. Future studies should explore differences in treatment needs among single and married depressed parents.
Conclusions
These findings highlight the need to develop affordable, accessible, personalized interventions that are effective for low-income, Hispanic parents with depression and their children attending urban family medicine practices. Strategies have been developed to engage depressed primary care patients in mental health services and reduce their symptoms. Specifically, evidence has been found for the effectiveness of telephone and face-to-face engagement interventions (
13), collaborative care provided by trained depression care managers and primary care doctors (
14), and a combination of evidence-based treatment and case management (
15). Feasible and acceptable mental health services targeting depressed parents and their children will most likely include a combination of these strategies. Finally, the similarities found between parents with major and subthreshold depression in their rates of problems and interest in treatment emphasize the importance of addressing depression among parents even when full diagnostic criteria are not met.
Acknowledgments and disclosures
This research was supported by National Institute of Mental Health (NIMH) grant P30MH071478 and in part by NIMH grant MH082255 (Dr. Weissman, principal investigator). Dr. Vidair was supported by NIMH grant T32MH016434. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIMH or the National Institutes of Health. The authors thank Ruth Chapas, B.A., Raashida Edwards, B.A., Ilene Hollin, M.P.H., Genevieve Izzo, M.A., Luz Marte, B.A., Stacy Pena, B.S., Annie Rabinovitch, B.A., Kimberly Savino, B.A., Kimberly Soto, B.A., and Timothy Soto, M.A., for conducting the survey; Laura Mufson, Ph.D., Moira Rynn, M.D., and David Shaffer, M.D., F.R.C.P., F.R.C.Psych., for assistance with study conceptualization; Prudence Fisher, Ph.D., Ronald Kessler, M.D., and Harold Pincus, M.D., for assessment consultation; Daniel Pilowsky, M.D., and Monica Sianez, M.P.H., for translations; Phil Adams, Ph.D., and Marc Gameroff, Ph.D., for data management; and Ardesheer Talati, Ph.D., for manuscript review.
The authors report no competing interests.