Major depressive disorder and milder forms of depression are disproportionately high among home health care patients, approaching 14% and 11%, respectively (
1). Although effective pharmacological (
2) and psychological (
3,
4) treatments exist for depression among older adults, depression remains undertreated in the home care setting (
1,
5,
6) for a variety of reasons, including patient reluctance to initiate and adhere to recommended treatments.
Examination of patient preferences for depression treatment may shed light on this reluctance and may identify subgroups of patients more likely to prefer certain treatments. The majority of research on treatment preferences has been conducted in primary care settings (
7–
16), and little is known about the mental health treatment approaches preferred by elderly home care patients. A pilot study found that prayer was the most preferred approach identified by elderly patients in long-term care (
17). However, personal experience with depression increased patient preference for medication or psychotherapy.
Using cross-sectional data from TRIAD (Training in the Assessment of Depression) of elderly patients newly admitted to home care (
18,
19), we examined the treatment preferences of this understudied population at high risk of depression. Previous work suggests that depression experience, namely having a diagnosis of major or minor depression or using antidepressant medication (
7,
12,
14,
17), is associated with preference for an active treatment, such as antidepressant medication or psychotherapy. We also explored the association between other sociodemographic and clinical variables and preference for an active treatment.
Results
The ages of the 256 patients enrolled in the study ranged from 65 to 96 years (mean±SD=78.2±7.1). A total of 158 patients (62%) were women, and 41 (16%) identified themselves as being from an ethnic-racial minority group. On average, clinical and functional measures indicated substantial medical morbidity and disability. The mean score on the Chronic Disease Score was 6.2±3.3. The mean number of reported limitations in activities of daily living was 1.4±1.5, and for instrumental activities of daily living the mean was 3.5±1.5.
Nineteen patients (7%) met criteria for major depression as assessed by the SCID, and 22 (9%) met criteria for minor depression. Of the 256 patients, 51 (20%) were currently taking an antidepressant, including five (26%) of the 19 patients with major depression, eight (36%) of the 22 patients with minor depression, and 38 (18%) of the 215 with no depression diagnosis. Twenty-one (8%) of the 256 patients reported previous but not current antidepressant use. No patient reported receiving psychotherapy on admission to home care, whereas 65 (25%) reported previous participation in psychotherapy.
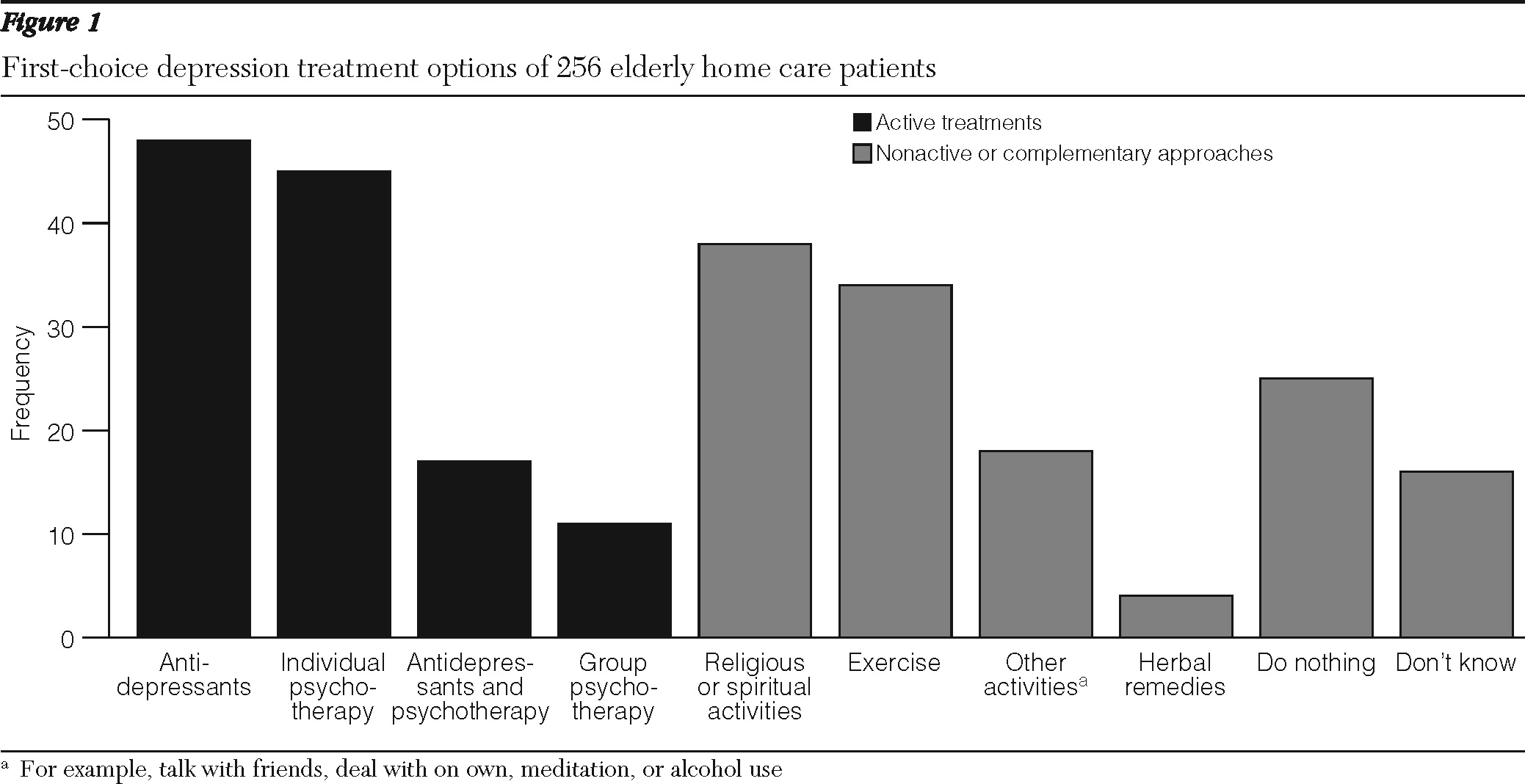
Figure 1 presents data on reported first-choice treatment options. Of the 256 patients, 121 (47%) preferred an active treatment as their first choice (antidepressant medication, psychotherapy, or a combination), and the remaining 135 (53%) preferred a nonactive or complementary treatment approach (such as religious or spiritual activities or exercise). As shown in
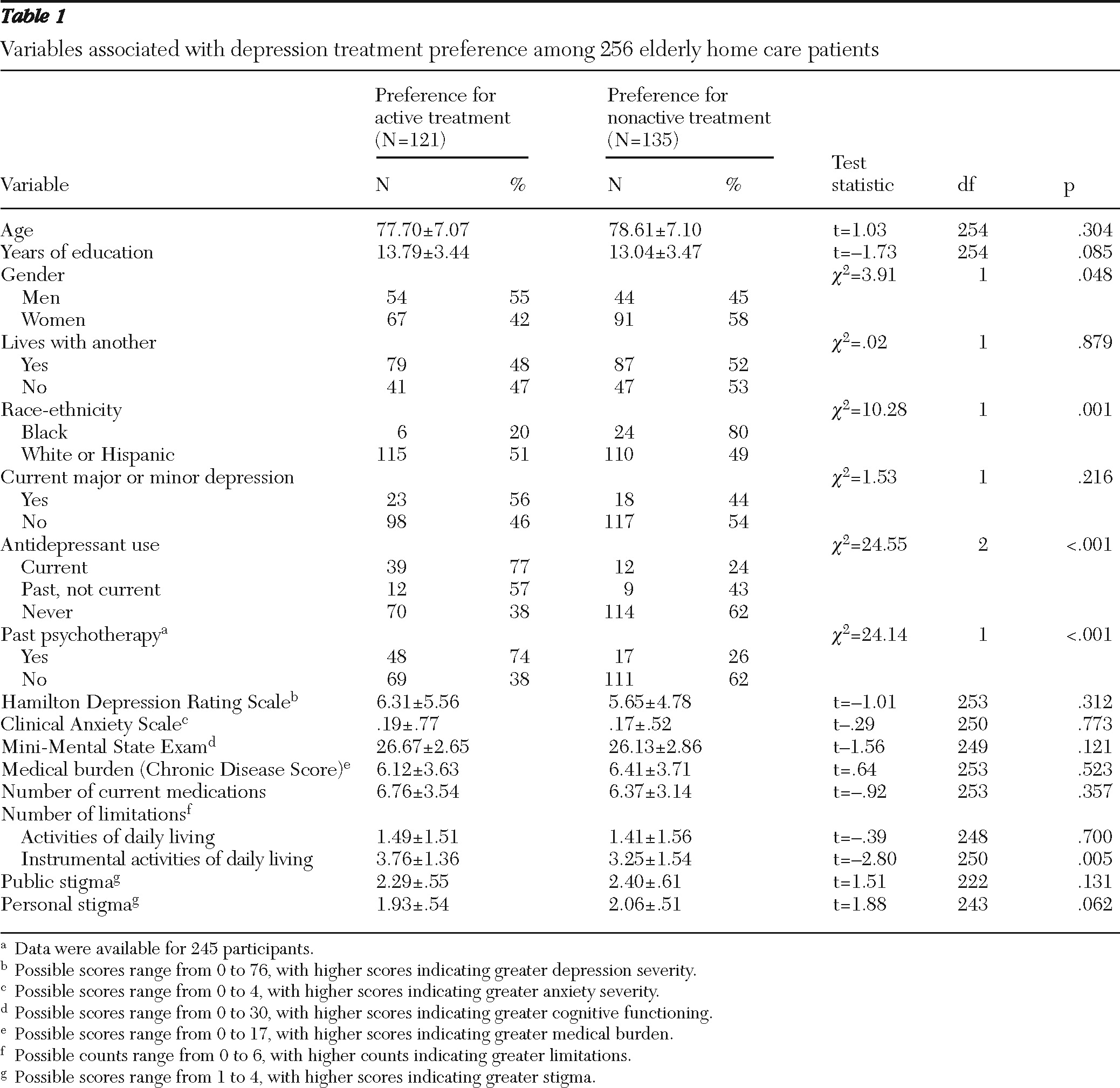
Table 1, of the 51 patients currently using antidepressants, 77% preferred an active treatment, compared with 57% of the 21 patients with past use of antidepressants and 38% of the 184 patients with no history of use (p<.001). A current diagnosis of major or minor depression was not significantly associated with treatment preference.
Other sociodemographic and clinical variables associated with preference for active treatment at p<.10 were male gender, more years of education, previous psychotherapy, race (white or Hispanic versus black), greater impairment in instrumental activities of daily living, and less personal stigma (
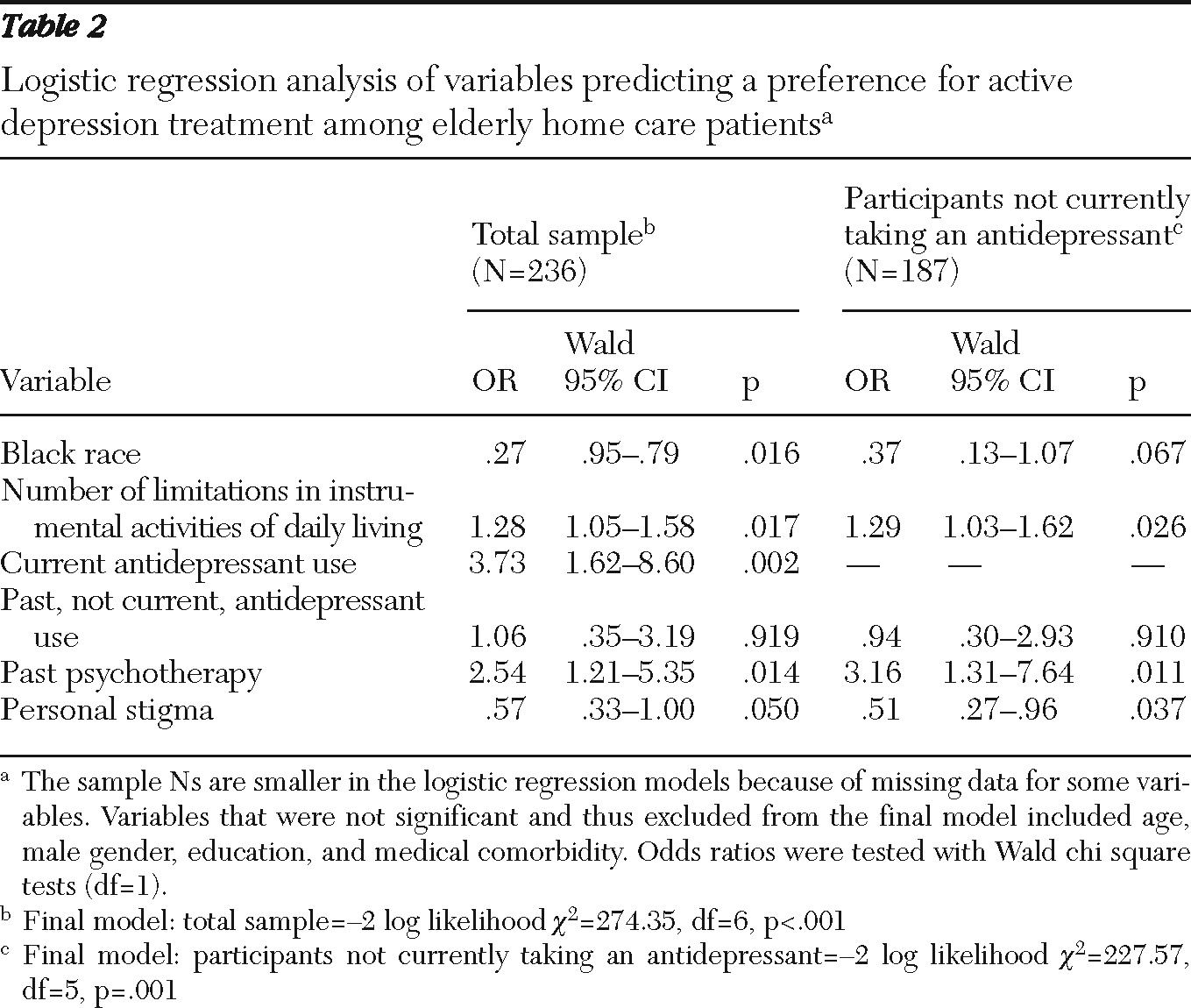
Table 1). The final logistic regression model indicated that current antidepressant use, previous psychotherapy, white or Hispanic race, greater impairment in instrumental activities of daily living, and less personal stigma were independently associated with a preference for an active treatment (
Table 2). When the sample was limited to participants who were not currently taking an antidepressant, the findings were similar (
Table 2).
Discussion
Elderly home care patients expressed a variety of first-choice preferences for depression treatment, ranging from active treatments, to religious or spiritual activities, to doing nothing. Similar proportions of patients preferred antidepressant medication (19%) and psychotherapy (18%). Smaller proportions preferred combined treatment (7%) or group psychotherapy (4%). The most commonly preferred nonactive or complementary approaches were religious or spiritual activities (15%) and exercise (13%). A number of patients (10%) preferred to do nothing in response to depression.
Forty-one patients had a current diagnosis of major or minor depression. Of these, 13 (32%) were currently taking an antidepressant and none were receiving psychotherapy. It may be that many of these patients were not receiving treatment either because they did not want to be treated or because no effort had been made to engage them in decisions about depression care. In addition, a sizable proportion (18%) of patients who were not currently depressed were taking an antidepressant, which may reflect appropriate maintenance treatment for depression or antidepressant prescription for reasons other than depression.
Our hypothesis that preference for an active treatment with either medication or psychotherapy would be related to depression experience was partly confirmed. Patients who were currently taking an antidepressant medication or who had taken one in the past were more likely than patients who had never taken an antidepressant to prefer an active treatment. Patients who were currently taking an antidepressant were nearly four times as likely as those not taking an antidepressant to prefer an active treatment. Previous experience with psychotherapy was also independently associated with preference for an active treatment. These findings are consistent with findings for primary care patients (
7,
12,
14) and long-term home care patients (
17). They suggest that the more experience patients have with treatment for depression, the more comfort or interest they have in pursuing (or continuing to pursue) such treatment.
Contrary to our hypothesis, a current diagnosis of major or minor depression was not associated with patient preference for an active treatment nor was our measure of depression severity. We predicted that the more individuals personally felt the distress of depression, the more they would prefer an active treatment approach, particularly compared with patients without depression, for whom the hypothetical clinical scenario regarding depression treatment would be less salient. Our ratings of symptoms, however, may not have captured perceived distress, which has been shown to be a better predictor of treatment initiation and adherence (
30,
31).
Logistic regression revealed that white or Hispanic versus black patients, those with greater impairment in instrumental activities of daily living, and those with less personal stigma were also more likely to prefer an active treatment. Restricting the sample to participants who were not currently taking an antidepressant yielded similar findings. The finding on race is consistent with previous research showing that black individuals have negative attitudes and beliefs about antidepressant medication in particular (
7,
10,
32) and are less likely than white patients to adhere to depression treatment (
33,
34). The finding on impairment in instrumental activities may indicate a greater experience with and acceptance of standard medical treatments. However, neither medical burden nor number of medications was associated with preference for active depression treatment. Perhaps impairment in instrumental activities is a better indicator of distress or impairment associated with depression than other medical variables. Alternatively, those who acknowledge a need for help, as exemplified by reports of limitations in instrumental activities of daily living, may be more likely to recognize the value of active depression treatment.
Stigma concerns and negative beliefs about depression and mental health treatment may influence the perception of such treatment as unacceptable and may lead to preferences for nonactive or complementary approaches (
35) and to poor medication adherence (
28,
30). Personal stigma (an individual's attitudes toward depressed individuals) was associated with a preference for active treatment, whereas public stigma (an individual's beliefs about society's attitudes) was not. A study of older adults who were receiving home-delivered meals found that personal stigma may be particularly meaningful for individuals whose functional disabilities result in a smaller social sphere and less concern with society's attitudes (
36). Also consistent with this finding, self-stigma but not public stigma was associated with attitudes about mental health treatment among diverse community-dwelling older adults (
32). The sociodemographic determinants of stigma among older adults and their impact on the treatment engagement process are promising areas for future investigation.
Limitations of the study include assessment of treatment preferences with a hypothetical question among patients who were not currently depressed. Also, we do not know whether patients who were depressed considered themselves to have a “serious” depression (which was the term used in the hypothetical question) and whether this belief would be related to treatment preference. In addition, actual treatment decisions, initiation, and adherence may differ when patients are presented with real-life treatment choices. Moreover, opportunities for home health care patients to engage in treatment consistent with their preferences may be constrained by practical issues, such as the availability of particular treatment approaches in this setting.
Another study limitation is that the prevalence of depression was relatively low compared with rates in other studies in home care (
1); this was partly the result of the aim of this study, which was to collect data for purposes of an intervention rather than to determine prevalence. Our sample from 2004 also had a low rate of antidepressant use (20%) compared with the rate in a more recent home health sample from 2007 (34%) (
37). Our rate, however, is higher than that found in a study five years earlier (11%) (
1), which reflects an increasing trend over time. Therefore, the distribution of patient preferences in this study may not be generalizable to the current home health care population. Findings on variables associated with treatment preferences, however, should not be affected by the potential sample biases. Another study limitation is that we did not have statistical power to separately examine factors associated with a preference for antidepressant medications and for psychotherapy. Our findings reflect preferences for active treatments in general. Finally, we did not have data on history of depressive disorders, and thus our findings are related to the impact of current depression and previous treatment experience.
Acknowledgments and disclosures
This study was supported by grants R24-MH64608, K23-MH069784, R01-MH084872, and R01-MH082425 from the National Institute of Mental Health. The authors thank the nurses, other clinicians, administrators, and support staff at their partnering agencies: Dominican Sisters Family Health Services, Visiting Nurse Association of Hudson Valley, and Visiting Nurse Services in Westchester.
Dr. Meyers has received research support from Forest Laboratories and has received honoraria from and has been a consultant to Corcept, Forest Laboratories, Pfizer, and Organon. The other authors report no competing interests.