Persons with serious mental illnesses, such as schizophrenia, schizoaffective disorder, bipolar disorder, and other psychotic disorders, have high rates of comorbid general medical conditions. Colocation of general medical services in the mental health setting might address the concern that undertreated medical conditions of patients with serious mental illness contribute to poor outcomes, including premature mortality (
1). Colocation could achieve this goal by improving access to care, continuity of care, and overall quality of care.
Ambulatory care-sensitive conditions are “conditions for which good outpatient care can potentially prevent the need for hospitalization or for which early intervention can prevent complications or more severe disease” (
2). Hospitalization for an ambulatory care-sensitive condition is an important outcome to consider in evaluating the quality of care because fewer admissions of patients with ambulatory care-sensitive conditions would indicate that good delivery of general medical services is preventing hospitalization. An analysis of New York State hospital discharge data found that persons with mental disorders had a higher risk of hospitalization for an ambulatory care-sensitive condition than persons without mental disorders and that their hospital stays also tended to be longer and more expensive (
3).
No previous studies have examined whether the colocation of general medical services in an outpatient mental health setting can reduce preventable hospitalizations. This study sought to examine whether Department of Veterans Affairs (VA) patients receiving care at VA mental health programs with colocated general medical care had fewer hospitalizations for ambulatory care-sensitive conditions than those receiving care in mental health programs without colocated general medical care.
Methods
This research is part of a study approved by the VA Ann Arbor Healthcare System Institutional Review Board. Data for fiscal year (FY) 2007 were obtained from the National Psychosis Registry and from the National VA Mental Health Program Survey, which was administered to all directors of VA mental health programs (N=133) in early 2007. Colocation of general medical services in the mental health program was determined by the response to a survey question that specifically asked about this arrangement. The Agency for Healthcare Research and Quality has published definitions of ambulatory care-sensitive conditions, along with a list of such conditions and associated
ICD-9-CM codes (
www.ahrq.gov/data/safetynet/billappb.htm) (
2). For this study, any hospitalization that listed one of these conditions as the primary diagnosis was counted.
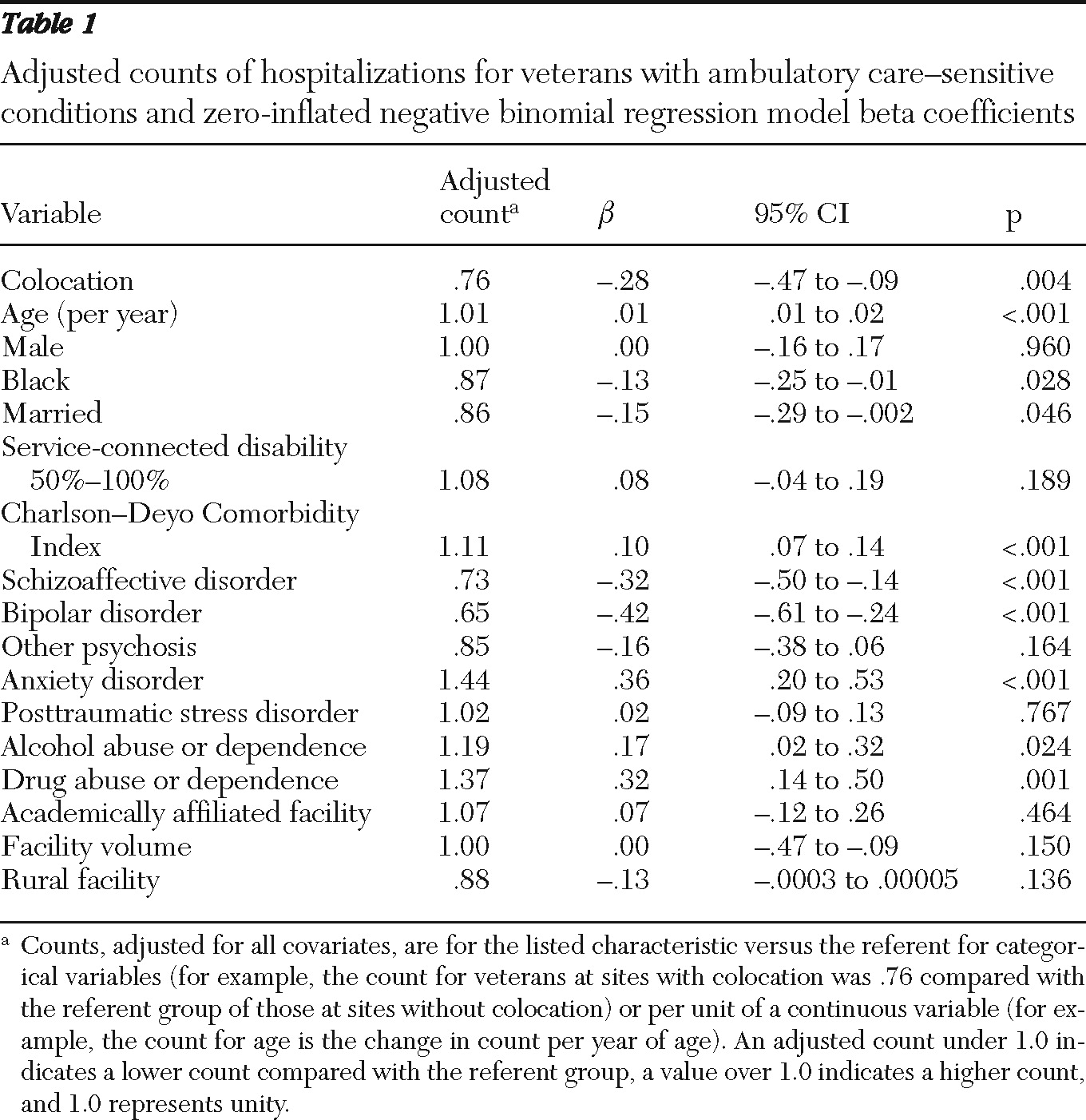
Zero-inflated negative binomial regression analysis was used to examine the relationship of colocation to the number of hospitalizations per veteran for ambulatory care-sensitive conditions. A negative binomial distribution was specified because it is less prone than a Poisson distribution to overdispersion, and the two-part modeling approach was used because of the large number of patients who were not hospitalized for an ambulatory care-sensitive condition (
4). The model controlled for age, gender, race-ethnicity, marital status, service-connected disability, Charlson-Deyo Comorbidity Index score (
5), primary psychiatric diagnosis (schizophrenia, schizoaffective disorder, bipolar disorder, and other psychosis), and comorbid psychiatric diagnoses (posttraumatic stress disorder, anxiety disorder, alcohol abuse or dependence, and drug abuse or dependence). Some veterans had more than one diagnosis. The model also controlled for site characteristics: rurality based on rural-urban commuting area codes (
6) (characterized as rural or not), facility volume (number of unique veterans with serious mental illness receiving care at the facility), and academic affiliation of the facility (coded as affiliated or not). The model also adjusted for clustering at the level of the VA facility by using generalized estimating equations. In the final model, only factors that were significantly associated with hospitalization for an ambulatory care-sensitive condition were included in the inflated portion of the model.
Results
Of the 92,268 veterans with serious mental illness from 108 mental health programs who had complete survey data, 9,664 (10.5%) received care at ten sites with colocated general medical services and 82,604 (89.5%) received care from 98 sites that did not have a colocated program. At sites with colocation, 95.7% (N=9,249) of veterans did not have a hospitalization for an ambulatory care-sensitive condition, 3.2% (N=309) had one, and 1.1% (N=106) had two or more. At sites with no colocation, 94.9% (N=78,391) had none, 3.9% (N=3,222) had one, and 1.2% (N=991) had two or more. The final model included all covariates in the standard portion of the model; age, marital status, Charlson-Deyo score, schizoaffective disorder, bipolar disorder, other psychosis, and drug abuse or dependence were included in the zero-inflated portion of the model. Being at a site with colocation was associated with an adjusted count of hospitalizations for an ambulatory care-sensitive condition of .76 compared with patients at sites with no colocation (
β=–.28, 95% confidence interval=.47 to –.09, p=.004;
Table 1). A confirmatory analysis with logistic regression for no hospitalization for an ambulatory care-sensitive condition versus any hospitalization for such a condition yielded similar results, as did another analysis that specified a zero-inflated Poisson distribution. A test for an interaction between academic affiliation of the VA facility and colocation was not significant.
Discussion
Colocation of general medical services in mental health settings was independently associated with fewer hospitalizations for an ambulatory care-sensitive condition in a national cohort of VA patients with serious mental illness. This finding suggests that such an approach may result in a lower rate of preventable hospital admissions. Furthermore, because we could not discern between veterans with serious mental illness who received colocated general medical services and those who did not, the finding of fewer hospitalizations suggests that the effect of having such a program may extend to all veterans with serious mental illness at the VA facility.
A 2006 literature review reported that colocation of medical services in the mental health setting was associated with improved access to and quality of care, as well as improvements in patients' health status; three such interventions were cost-neutral from the perspective of the health plan (
7). A previous VA study found that a colocated, integrated primary care program in the mental health setting was efficacious in a single-site randomized controlled trial; the program was associated with increased use of primary care and greater attainment of performance measures at no additional total cost (
8). Two more recent VA studies further supported colocated models. In a single-site study with a quasi-experimental design, colocated services for homeless veterans with mental illness improved access to primary care services and reduced emergency service utilization (
9). A colocated primary care clinic for veterans with substance use disorders increased primary care attendance and engagement in substance abuse treatment and was also cost-neutral with respect to VA health care costs (
10). A recent report demonstrated the benefit of medical care management in community mental health settings for persons with serious mental illness (
11).
Other findings with respect to factors associated with hospitalizations for ambulatory care-sensitive conditions deserve comment. The findings for age, medical comorbidity, alcohol abuse and dependence, drug abuse and dependence, and anxiety are consistent with results of other studies (
3,
12), but the finding that blacks had fewer hospitalizations for ambulatory care-sensitive conditions is not (
13). This finding may be specific to the study population of veterans with serious mental illness. Patients with a diagnosis of bipolar disorder or schizoaffective disorder had fewer hospitalizations for ambulatory care-sensitive conditions than those with schizophrenia. This may indicate that patients with schizophrenia have more difficulty navigating the medical system and do not receive timely care.
Our finding represents a relatively small impact in terms of the potential reduction in hospital admissions that could be realized from colocation of care because the absolute difference between sites with collocation and those without it was only .8%. However, a crude estimation suggests that the cost savings are potentially considerable. For example, assume that hospitalization in a VA acute medical service for an ambulatory care-sensitive condition occurred once a year for a patient with serious mental illness and lasted two days at a cost of $1,831 per day (based on the FY 2007 national VA average daily cost for an acute medical hospitalization). An .8% reduction in such hospitalizations in FY 2007 among veterans with serious mental illness at the sites with no colocation that were included in this study translates to approximately $2.4 million less spent nationally on hospitalizations for ambulatory care-sensitive conditions. Obviously, formal analyses of costs associated with colocation of care and hospitalizations for ambulatory care-sensitive conditions are needed, including evaluation of whether the savings offset the costs of colocated programs.
The study was cross-sectional, and causality cannot be inferred. Having colocated general medical services may be a marker for sites that provide higher-quality care rather than being the cause of fewer hospitalizations for ambulatory care-sensitive conditions. Being able to distinguish between veterans who received care from the colocated services and those who did not would help to address this question, but the available administrative data could not elucidate this issue. The study's scope was limited to those who received VA services; however, previous work has shown that veterans who use mental health services move infrequently between VA and non-VA care (
14). Because the entire VA health care system has some elements of integrated care, including proximity and shared use of the electronic medical record, the effect size reported could be an underestimate of the effects that could be achieved by colocation in other health systems. Alternatively, our findings may not extend outside the VA. Further work to examine colocation is needed that is longitudinal, compares veterans with serious mental illness who received these services to those who did not, uses more extensive measures to help account for the heterogeneity across sites with respect to characteristics and culture, and includes a formal detailed cost analysis.