The prevention and treatment of diabetes among individuals with serious mental illness has been a recent focus in part because of the reportedly direct relationship between antipsychotics and metabolic syndrome. Adults with developmental disability are also at high risk of diabetes because of their sedentary lifestyle, cognitive impairments, and deficits in adaptive behavior and are less likely than other vulnerable populations to receive appropriate diabetes care (
1). Some individuals with developmental disability also have serious mental illness. Whether they are at higher risk of diabetes than those with either serious mental illness or developmental disability alone has not been studied.
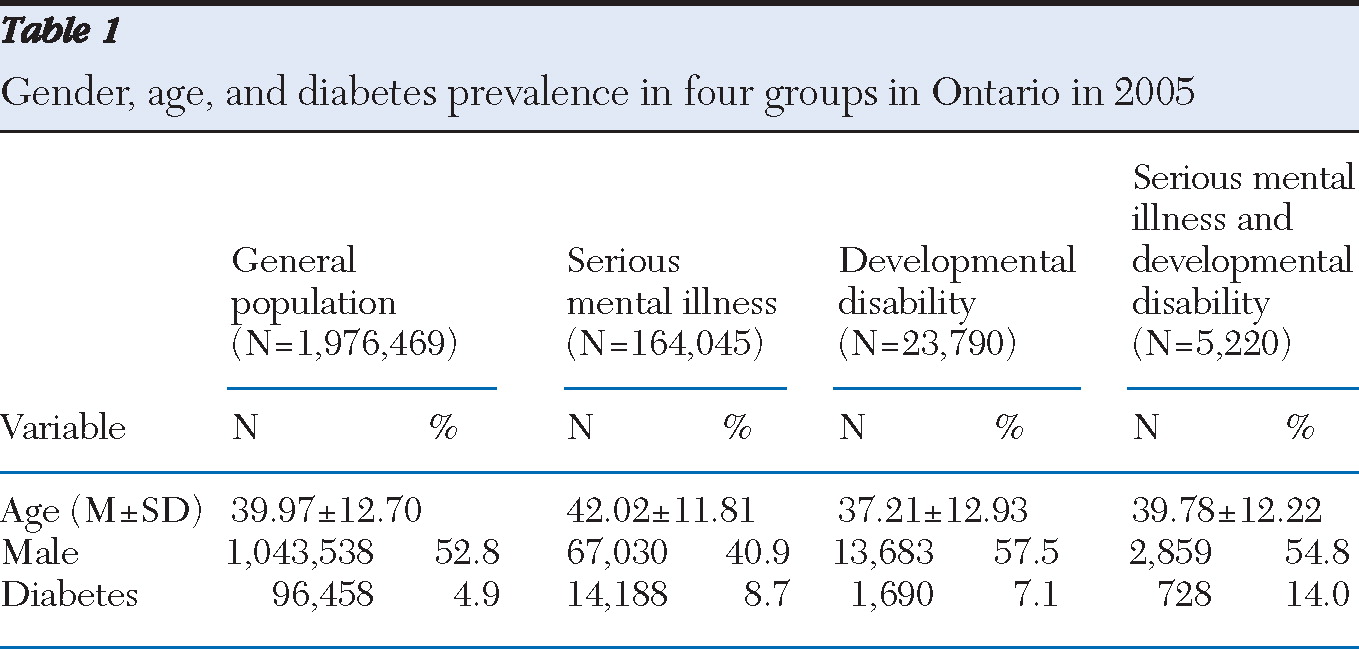
We compared the prevalence of treated diabetes in four groups of adults: with serious mental illness, with developmental disability, with serious mental illness plus developmental disability (“combined” group), and a random sample of the general population. We hypothesized that the combined group would have the highest diabetes risk.
Data for fiscal 2005–2006 were obtained from the Institute for Clinical Evaluative Sciences, which holds deidentified records of all physician billings and hospital visits made by Ontario residents. The four groups and those with treated diabetes were identified using ICD-9 and ICD-10 codes and the Ontario Diabetes Database, respectively.
Compared with the rate in the general population, diabetes rates were higher in the three groups (severe mental illness, developmental disability, and the combined group) (
Table 1). When age and sex were controlled for, the odds of having diabetes were 1.78 times higher (95% confidence interval [CI]=1.75–1.82) among those with severe mental illness and 1.84 times higher (CI=1.75–1.94) among those with developmental disability, compared with the general population. As hypothesized, the combined group had the highest likelihood of having diabetes (adjusted OR=3.63, CI=3.34–3.94).
Because we could not track medications, it is unclear what contribution, if any, use of second-generation antipsychotics made to rates of diabetes, and further research is required to determine what role they might play. Our data suggest that increased attention to persons in the combined group by monitoring their clinical symptoms and functioning levels and devising better ways to help them and their families manage their treatment would be useful, pending more definitive answers.
Acknowledgments and disclosures
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Additional support was from annual MOHLTC funding to the Centre for Addiction and Mental Health. The opinions, results, and conclusions reported here are those of the authors. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
The authors report no competing interests.