An increase in dating violence has heightened public concern about intimate partner violence. Intimate partner violence is defined as any threatened, attempted, or completed physical or sexual violence and emotional abuse inflicted by a spouse, ex-spouse, current or former boyfriend or girlfriend, dating partner, or date (
1). Approximately 30% of all female homicides are committed by a male intimate (
2). The World Health Organization estimates that intimate partner violence costs the United States $12.6 billion or .1% of the gross domestic product annually (
3). Intimate partner violence accounts for 20% of nonfatal violent crimes against women and 3% of those against men (
4).
Accumulating evidence relates intimate partner violence to life-threatening and significant adverse physical health consequences. Furthermore, intimate partner violence is associated with depression, posttraumatic stress disorder, and substance abuse (
5,
6). The National Comorbidity Survey reported that 17.4% and 18.4% of women and men, respectively, were victims of intimate partner violence during the course of their current marriage or cohabitation (
7). Similarly, the National Comorbidity Survey Replication found that 15.2% of females and 20.3% of males had been victims of intimate partner violence during their current marriage or cohabitation (
8). National studies have examined the prevalence of psychiatric disorders among victims of intimate partner violence and the value of psychiatric disorders in predicting such victimization, but their cross-sectional design did not permit estimation of the effects of intimate partner violence on risk of incident or new-onset psychiatric disorders. By drawing on data from the second wave of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a large, nationally representative sample of adults in the United States, we sought to compare the 12-month incidence of psychiatric disorders among individuals who were or were not victims of intimate partner violence during the past 12 months and examine whether increased frequency of exposure to violent acts was associated with an elevated incidence of psychiatric disorders.
Methods
The wave 2 NESARC (2004–2005) design involved face-to-face reinterviews with participants in the wave 1 interview. Wave 1 of the NESARC was conducted in 2001–2002 and is described in detail elsewhere (
9,
10). The target population was the civilian population, 18 years and older, residing in households and group quarters such as boarding or rooming houses, college housing, and group homes. Face-to-face interviews were conducted with 43,093 respondents, yielding an overall response rate of 81.0%. Excluding respondents ineligible for the second interview (for example, those who were deceased), the wave 2 response rate was 86.7%, reflecting 34,653 completed interviews. The cumulative response rate for wave 2 is the product of the wave 2 and wave 1 response rates (70.2%). Weighted data on socioeconomic variables were then adjusted to represent the civilian population of the United States on the basis of the 2000 decennial census.
All potential NESARC respondents were informed in writing about the nature of the survey, the statistical uses of the survey data, the voluntary aspect of their participation, and the federal laws providing strict confidentiality of the identifiable survey information. Those respondents consenting to participate were interviewed after receiving this information. The research protocol, including informed consent procedures, received full ethical review and approval from the U.S. Census Bureau and the Office of Management and Budget.
Wave 2 of the NESARC included questions on intimate partner violence. Respondents in the NESARC who were married or living with someone as if married at the time of the interview and those who responded that in the past 12 months they had been married, dating, or involved in a romantic relationship constituted our study sample (N=25,626).
Sociodemographic measures included sex, sexual orientation, race-ethnicity, nativity, age, education, marital status, place of residence (urban or rural), and region of the country (Northeast, Midwest, South, and West). Socioeconomic measures included employment status, personal and family income, and health insurance type.
The diagnostic interview was the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV), wave 2 version. This structured interview was designed for administration by experienced lay interviewers and included questions about mood disorders, anxiety disorders, and substance use disorders. AUDADIS-IV methods to diagnose these disorders are described in detail elsewhere (
10).
History of intimate partner violence in the past 12 months was assessed with items from the Conflict Tactics Scale, Form R, a widely used, valid, and reliable measure of family violence (
11). Cronbach's alpha coefficients ranged from .69 to .88 for items on physical aggression. The questions were preceded by asking respondents if they were currently married or living with someone as married or if during the past 12 months they had ever married, dated, or been involved in a romantic relationship. Intimate partner violence was then assessed with questions about the respondent's spouse or partner. After being presented with an introductory statement that people handle disagreements in different ways, respondents were asked whether at least once during the past 12 months their spouse or partner had pushed, grabbed, or shoved them; slapped, kicked, bit, or hit them; threatened with a weapon (such as a knife or gun); cut or bruised them; forced them to have sex; or injured them enough to get medical care. A positive response to one or more items defined intimate partner violence. Respondents were also asked about the frequency of each of these behaviors during the previous year.
To minimize the possibility that associations between intimate partner violence and 12-month psychiatric disorders were due to psychiatric disorders preceding intimate partner violence, we estimated the incidence of psychiatric disorders. Incidence rates were calculated as the number of new cases of psychiatric disorder during the year preceding the wave 2 interview among all respondents who reported and did not report being a victim of intimate partner violence. The denominator for each disorder comprised the total number of individuals in the intimate partner violence sample with no prior history of that disorder at the start of the year. This incidence rate was expressed as a percentage.
The frequency with which individual items from the Conflict Tactics Scale were endorsed was determined overall and stratified by the respondents' gender. The 12-month prevalence of intimate partner violence was then determined overall and stratified by the respondents' sociodemographic and socioeconomic group.
A series of logistic regression models were fit to evaluate the effect of each background characteristic on risk of intimate partner violence. We also examined associations between frequency of each act of intimate partner violence and incidence of psychiatric disorders. Results are presented as odds ratios (ORs) with associated 95% confidence intervals (CIs). Weighted means, frequencies, and ORs of sociodemographic correlates and incident psychiatric disorders were also computed. Adjusted odds ratios (AORs) derived from multiple logistic regressions indicated associations between a specific outcome (such as psychiatric disorders) and sociodemographic and socioeconomic correlates that differed between those who did and did not experience intimate partner violence. We considered two percentage estimates to be significantly different from each other if their CIs did not overlap. ORs were considered significant if their CIs did not include 1. All standard errors and CIs were estimated with SUDAAN (
10) to adjust for the survey design characteristics.
Results
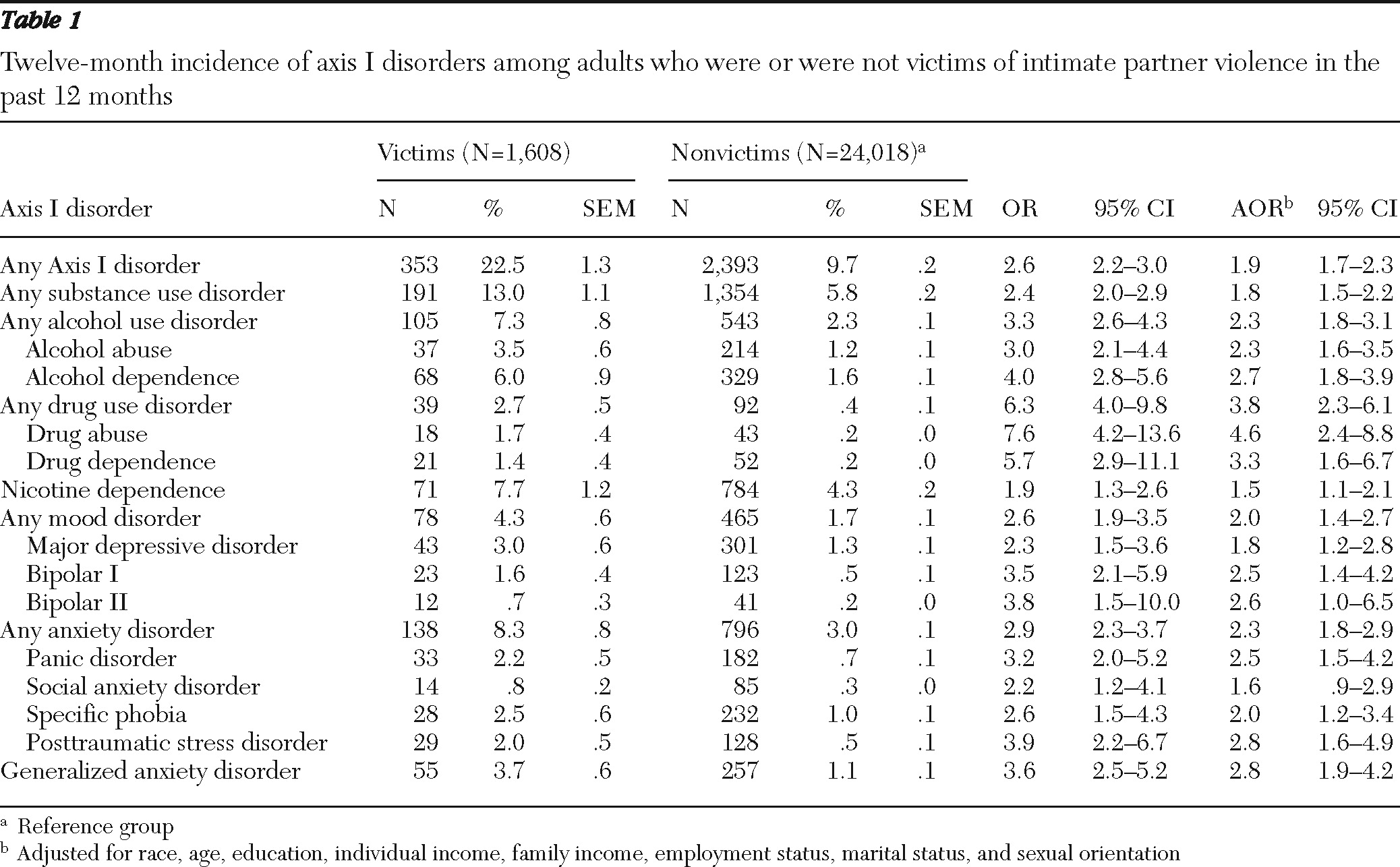
During the course of one year, 1,608 individuals reported being a victim of intimate partner violence, including 5.8% of men (N=718 of 11,783) and 5.6% of women (N=890 of 13,843). The overall odds did not significantly differ by sex. Approximately one in five (22.5%, N=353) respondents reporting intimate partner violence had an incident axis I psychiatric disorder during the 12-month period before the wave 2 interview (
Table 1). Victims of intimate partner violence had significantly greater odds than did nonvictims of meeting criteria for all measured incident psychiatric disorders, except for social anxiety disorder, in the adjusted analyses. Among victims, incidence rates were highest for alcohol dependence, nicotine dependence, generalized anxiety disorder, and posttraumatic stress disorder. The odds of meeting criteria for various psychiatric categories among those who had or had not experienced intimate partner violence were greatest for drug abuse and dependence, bipolar I and II disorders, alcohol dependence, posttraumatic stress disorder, and generalized anxiety disorder. The ORs remained significant after adjusment for sociodemographic and socioeconomic variables.
For most of the violent acts, there was a direct relationship between the frequency of the acts and the incidence of a psychiatric disorder. [Tables summarizing demographic characteristics of victims of intimate partner violence, the types of violence reported, and the incidence of psychiatric disorders by type and frequency of violent act are available in an online appendix to this report at
ps.psychiatryonline.org.]
Women were significantly more likely than men to have been cut, bruised, or forced to have sex. By contrast, men were more likely than women to have been slapped, kicked, bitten, or hit. Men and women were roughly equally likely to have been pushed, grabbed, shoved, threatened with a weapon, or injured enough to seek medical help in the past 12 months.
Discussion
In a large, nationally representative sample of adults in the United States, roughly 5.6% of women and 5.8% of men reported being victims of intimate partner violence in the course of one year. As a group, these adults were at markedly increased risk for developing a wide range of psychiatric disorders. Moreover, increased frequency of the violent acts contributed to increased risk of developing a psychiatric disorder.
In accord with previous research (
12), the prevalence of intimate partner violence victimization did not significantly differ across genders. Although women in our study were more likely than men to be victims of sexual violence, they were equally likely to have been threatened with a weapon and to have sustained injuries leading to medical care. This pattern of victimization suggests that increased efforts may be needed to expand services to men who are victims of intimate partner violence. To our knowledge, specific treatment programs to address the needs of male victims do not exist, and existing services for men focus on decreasing their perpetration of violence.
Community-based advocacy and counseling services for intimate partner violence victims have shown promise in decreasing rates of repeated abuse, increasing service access, enhancing social support, and improving quality of life (
13). Identification of victims appears to influence outcomes of care (
14). Though more evidence-based studies are clearly still needed, enough information about interventions for victims of intimate partner violence is now available to provide useful clinical guidelines to health care providers (
14).
Approximately one-fifth of those victimized in the previous 12 months suffered from a new-onset psychiatric disorder, and the risk of new onset was related to the frequency of the violence. Intimate partner violence was associated not only with an increased risk of posttraumatic stress disorder, major depressive disorder, and substance use disorders, as previously reported (
5,
6), but also of bipolar disorder, panic disorder, and generalized anxiety disorder. Previous research indicates that a history of child physical and sexual abuse increases the prevalence of several disorders in adulthood (
15). Our results further documented that violence by intimates experienced by adults may increase the risk of new-onset psychopathology. Some of the mechanisms by which abuse in childhood is theorized to lead to increased rates of psychopathology, such as disruptions in the sense of self, inability to regulate reactions to stressful events, and other interpersonal and emotional challenges, may have analogues in adult interpersonal violence. Detailed clinical psychopathological research is needed to uncover the mechanisms that govern the associations observed between intimate partner violence and mental disorder onset among adults.
This study had several limitations. First, information on intimate partner violence was based on self-report and was not confirmed by collateral informants or criminal justice system records. Second, due to the chronic nature of intimate partner violence, some individuals who had been victimized in the past 12 months could already have developed a subsequent psychiatric disorder and thus not have been included among the incident cases. Their omission would have resulted in an underestimation of the affected population. However, even our conservative estimates using incidence rates demonstrated a significant and substantial association between intimate partner violence and incident psychiatric disorder. Third, our sample included individuals who experienced changes in their marital status, and it is not possible to determine whether these changes preceded or antedated the intimate partner violence.
Conclusions
Intimate partner violence is highly prevalent in the United States, affects both men and women, and is associated with onset of a broad range of psychiatric disorders. Physicians and other health care professionals may have opportunities to play a key role in identifying victims, helping them mobilize resources, extricating them from victimizing relationships, helping them to acquire the skills necessary to build social supports, reducing psychological distress, and lowering the risk of psychiatric disorder onset. Findings from this study highlight the urgency of expanding access to interventions that target the suffering from violence within intimate adult relationships.
Acknowledgments and disclosures
NESARC was sponsored by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and funded, in part, by the Intramural Program, NIAAA, and the National Institutes of Health (NIH). This study is supported by NIH grants DA019606, DA020783, DA023200, DA023973 and MH076051, P60 MD000206, R01 AA08159, K05 AA00161, and U01 AA018111 and the American Foundation for Suicide Prevention. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations or agencies or the U.S. government.
The authors report no competing interests.