Bipolar disorder is a chronic illness characterized by recurrent manic, hypomanic, mixed, and depressive episodes. Lifetime prevalence for bipolar disorder ranges from 1% for bipolar I to nearly 4% for bipolar II disorder and subthreshold or soft-spectrum bipolar disorder (
1). An early and frequently cited evaluation of cost was completed by Wyatt and Henter (
2) in 1991, estimating total direct costs for bipolar disorder in the United States to be greater than $7 billion. This cost paled in comparison with the indirect cost related to lost work productivity and overall economic burden of bipolar disorder that was estimated during the same year at $45 billion (
2,
3). More recent data have confirmed the substantial economic burdens of bipolar disorder.
Additional data come from employer-based databases. In several studies of employer-based data from 200,000 to >400,000 enrollees, bipolar disorder was identified as the most costly of the mental health disorders (
4–
6). Of the top ten most costly medical conditions in the Goetzel and colleagues' (
4) study, the top four were the chronic maintenance of angina pectoris, hypertension, diabetes mellitus, and mechanical low back disorder. If the costs from that same study for bipolar chronic maintenance, bipolar depression, and “severe” mania were combined, it would place bipolar disorder fifth in the list of the top ten most costly medical conditions (
4). In the same analysis, bipolar depression had the highest percentage (58%) of costs related to work absence or short-term disability.
There is increasing interest in directly comparing mental health care costs with medical costs. In a study by Simon and Unützer (
7), six-month use and cost data from patients with bipolar disorder enrolled for one year (1995–1996) in a health maintenance organization revealed that patients with bipolar disorder had higher costs, specifically mental health care and substance abuse services, than patients with depression or diabetes. Total health plan treatment costs for bipolar disorder in this sample were at a mean of $3,416. Total medical (non-mental health) costs were lower for patients with bipolar disorder ($1,850) in this sample than for depressed patients ($2,311) or diabetic patients ($3,034). The authors mentioned that the depression medical costs were affected by a few high-cost outliers. Although many of these studies have described total costs related to bipolar disorder or depression, little is known about the differences between bipolar disorder and depression in subtypes of cost and how these costs compare with other common chronic conditions.
The goal of this study was to retrospectively evaluate health care costs of bipolar disorder compared with other common chronic conditions. We placed a specific emphasis on patterns of health care utilization that might help explain the higher direct cost of care for patients with bipolar disorder and point to possible utilization targets when designing interventions to improve the delivery of health care for this population.
Methods
This study was approved by our institution's review board.
The population for this study was derived from a Midwestern, employer-sponsored, self-funded health plan serving approximately 80,000 enrollees in a defined geographic area. All preferred mental health and general medical providers are paid by salary, with no individual financial incentives tied to utilization or referral patterns. There was no copay for a primary care visit, whereas the copay for any specialist visit (including a psychiatrist) was $25. The enrollees were free to seek care outside of the preferred providers for a 30% coinsurance. Hospitalizations at the preferred hospitals required a 10% coinsurance, whereas hospitalization at other hospitals required a 30% coinsurance. This health plan was compared with similar plans as described in the
Employer Health Benefits 2000 Annual Survey (
http://www.kff.org/insurance/7672/upload/76723.pdf) and was found in regard to cost sharing to be typical of the majority of plans described.
The individuals included in the study population were all members of the health plan continuously enrolled from January 1, 2004, to December 31, 2007, and were identified with the National Committee on Quality Assurance's Healthcare Effectiveness Data and Information Set criteria for identification for each of the conditions (clinical diagnoses) of interest. This required at least two separate office visits, an emergency room visit, or an inpatient stay with a secondary diagnosis of the condition or one inpatient stay with a primary diagnosis for the condition. We identified members who met these criteria for each of the chronic conditions: bipolar disorder, major depression, asthma, coronary artery disease, and diabetes.
The small size of the primary group of interest led to the decision to categorize any patient with a bipolar diagnosis and a comorbidity as bipolar only. To address the possibility of misclassification of the bipolar cohort, we quantified the number of times those individuals were given a bipolar disorder diagnosis versus a depression diagnosis. Within this small group, a bipolar diagnosis was found, on average, 2.3 times as often as a depression diagnosis in the four years of study. Because of the difficulty in cost attribution, all other patients were categorized under their primary and secondary diagnoses. For example, a patient with depression and diabetes would have costs counted under both categories. The small sizes of comorbid groups made subgroup analysis difficult, except for those patients with both diabetes and coronary artery disease. Given the large sample size of patients with comorbid coronary artery disease and diabetes, this was identified as a separate subgroup. The criteria for identification of the study cohort were applied in the year before the first study time period (January 2004).
Costs of all health care services covered by the group health cooperative for the four-year period starting January 1, 2004, were reviewed. Data were extracted from medical and pharmacy claims that capture each unit of service paid for by the health plan (an outpatient visit, prescription, inpatient day). For each service, we used the paid amount (including both plan and enrollee component) to capture the costs utilizing the Berenson-Eggers Type of Service classification system (
www.cms.hhs.gov/HCPCSReleaseCodeSets/20_BETOS.asp), which was used by Medicare for attributing the services to each of the cost categories. These categories included outpatient visits, imaging, testing, procedures, inpatient care, emergency department, and psychiatric care. Additionally, all outpatient medication costs were attributed to the pharmaceutical category.
Health care cost data typically show a highly skewed distribution due to high-cost outliers. For categories showing an approximately lognormal distribution, including total cost and total general medical cost, statistical tests were conducted on the log scale. For categories with a large number of nonusers—such as costs for specialty mental health and substance abuse services—tests were based on rank transformation with the Mann-Whitney test. Finally, all adjusted models were based on generalized linear models using a gamma distribution and a log link (
8). The models were adjusted for age, sex, and comorbid conditions with the Charlson Comorbidity Index (
9). The results are presented as predicted means with bootstrapped confidence intervals. Using logistic regression and adjusting for age, sex, and comorbid conditions, we compared characteristics of bipolar disorder patients whose costs were in the top 20% of spending with those whose costs were in the lower 80% group.
Results
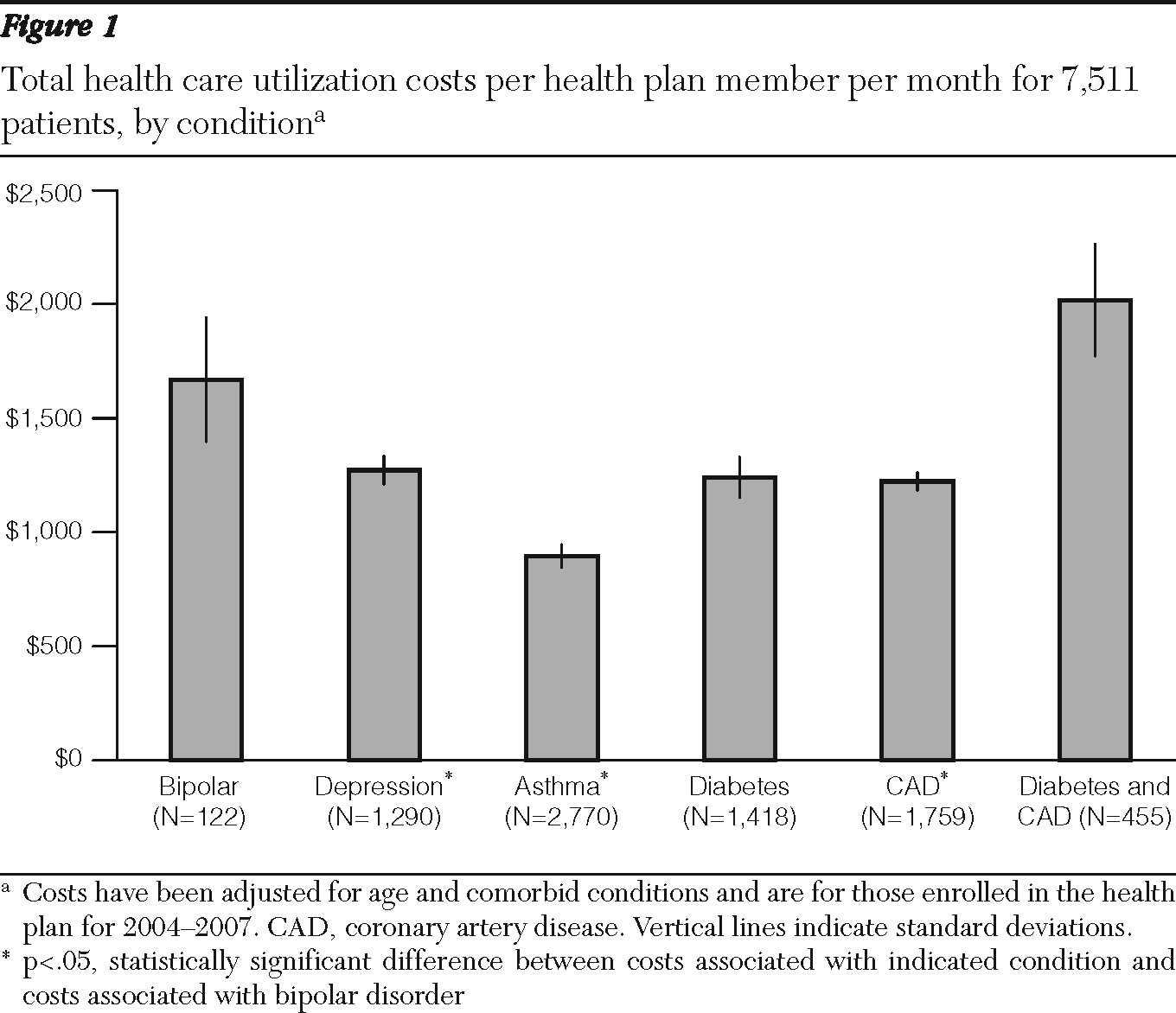
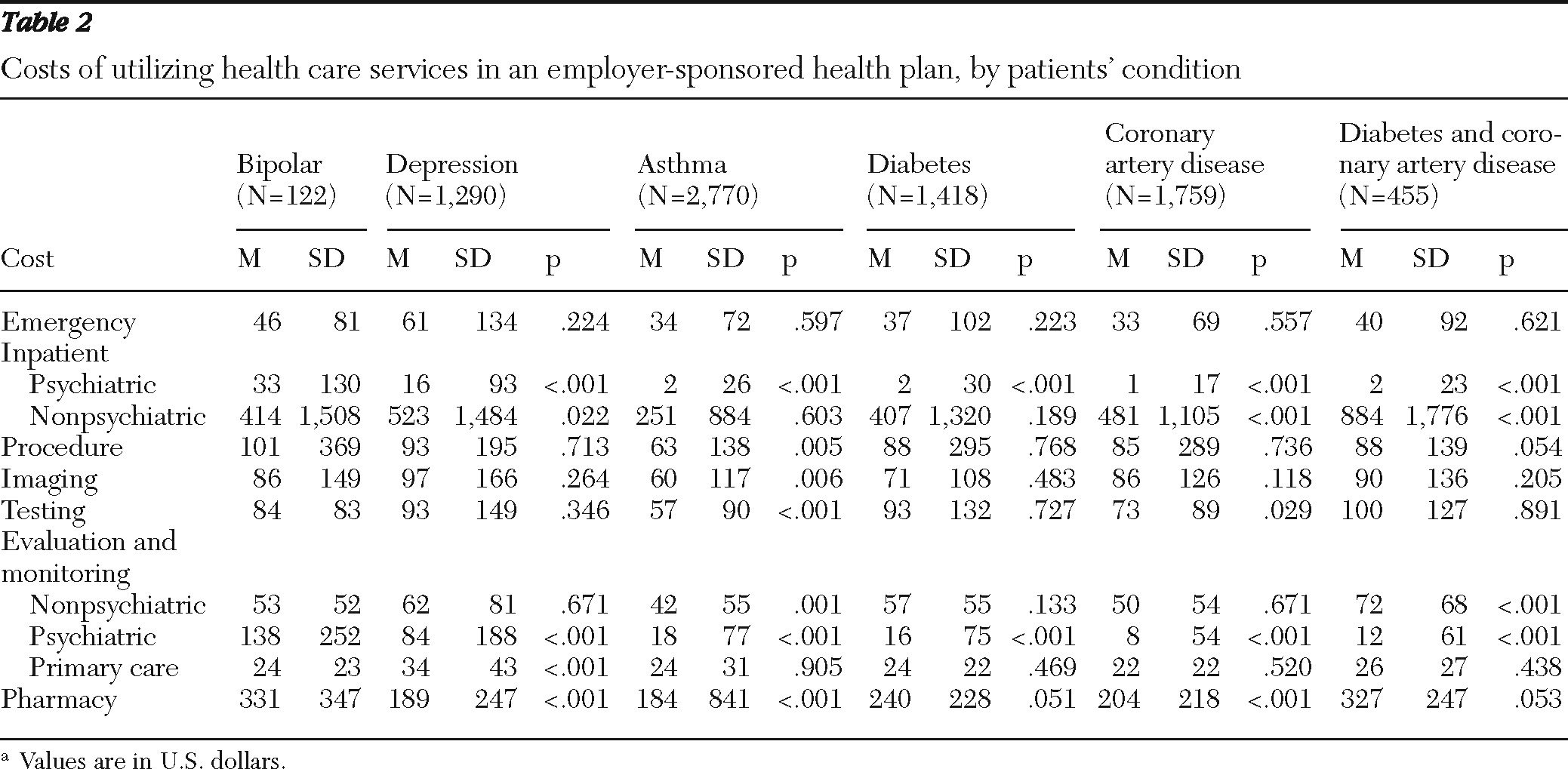
The study population is described in
Table 1. The bipolar group was, on average, older than the depression and the asthma groups but younger than the coronary artery disease and diabetes groups. Additionally, the bipolar group had a relatively low level of comorbidity.
Total costs were adjusted for age and comorbidities (
Figure 1). These overall costs were highest in those patients with both diabetes and coronary artery disease. Total costs for patients with bipolar disorder were significantly (p<.05) higher than those for patients with depression, asthma, and coronary artery disease and numerically but not statistically (p=.06) higher than those for patients with diabetes.
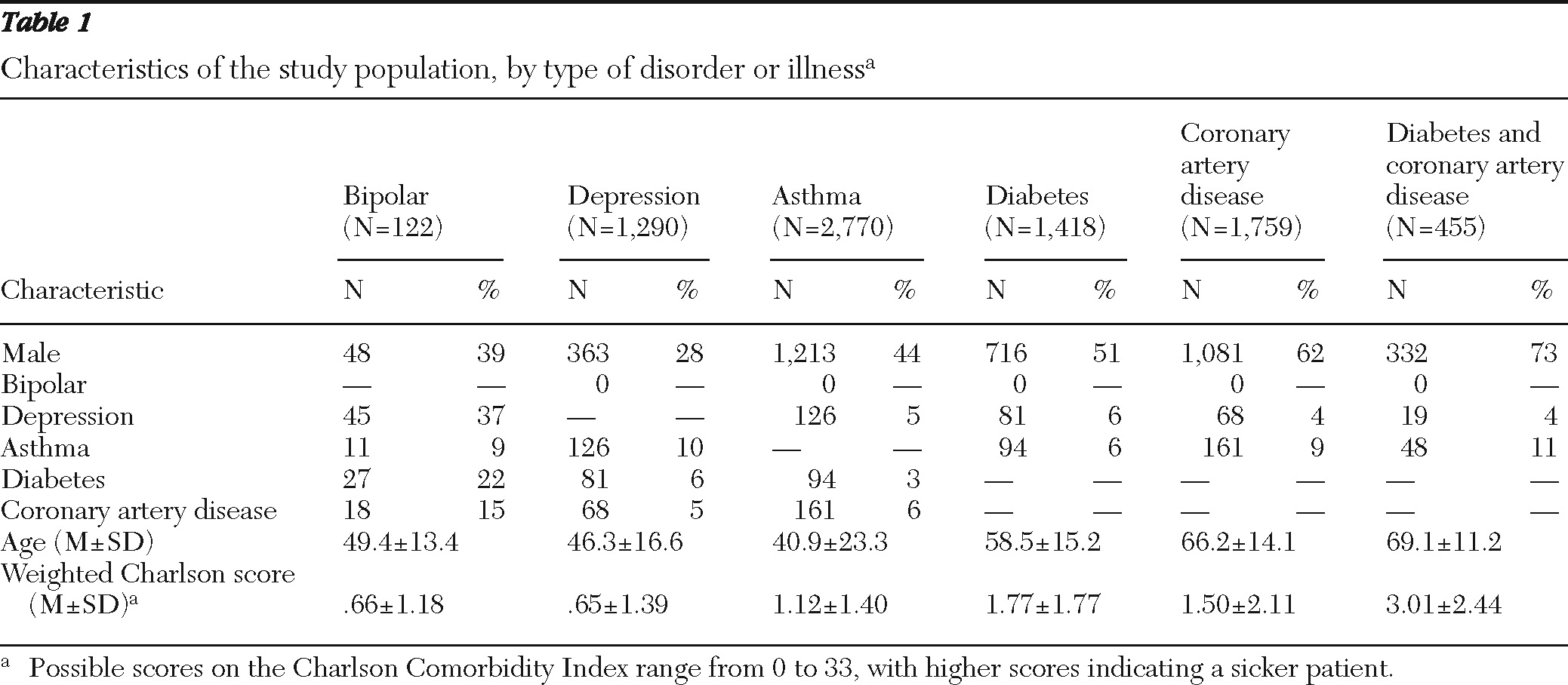
Inpatient and outpatient psychiatric costs were higher for patients with bipolar disorder than for any of the other groups (
Table 2). Compared with patients with bipolar disorder, those with depression had statistically significantly higher primary care utilization (p<.001) and higher nonpsychiatric inpatient admissions (p=.022). Patients with bipolar disorder had higher pharmacy costs than patients with depression, asthma, and coronary artery disease (p<.001).
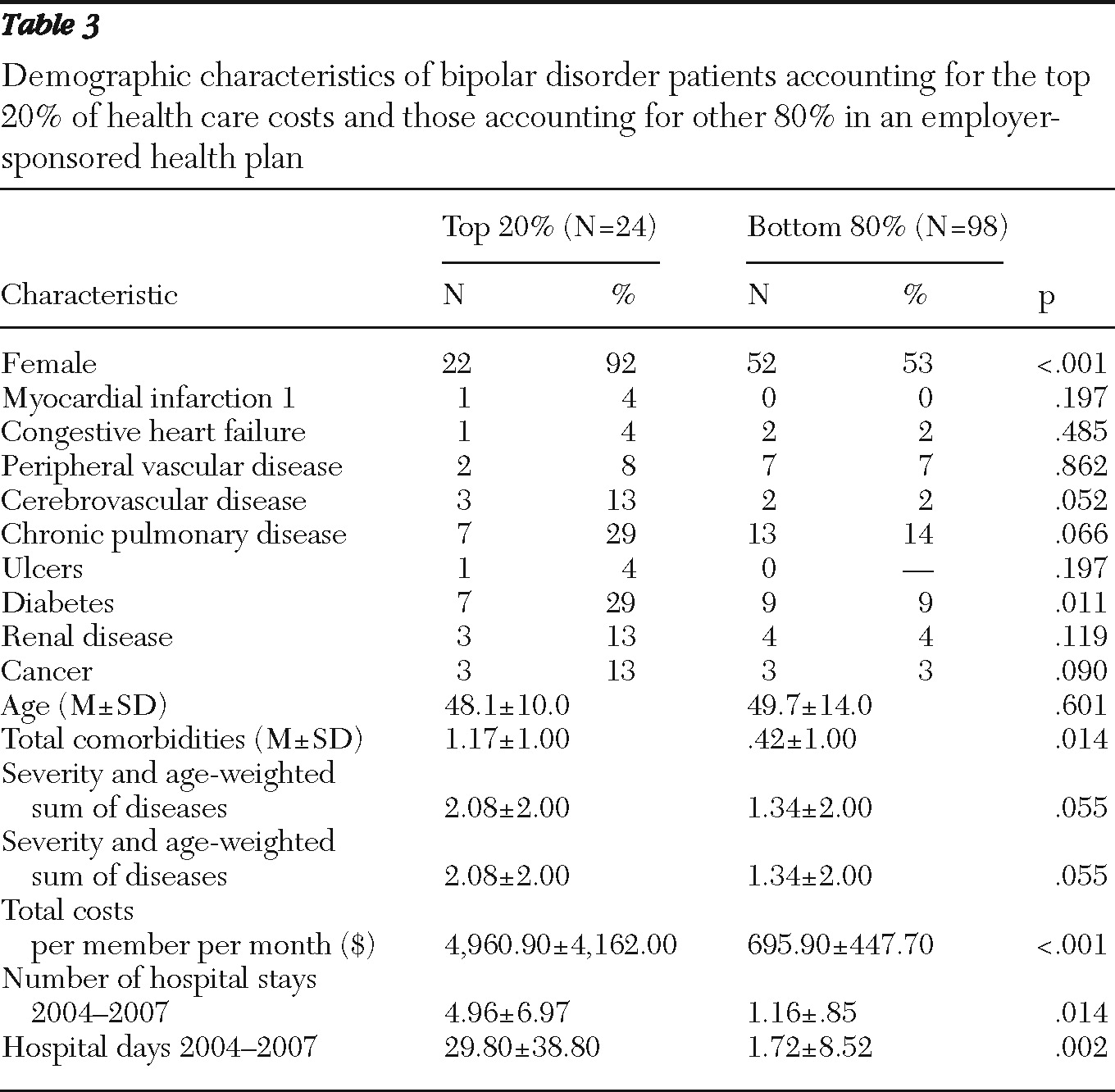
The distributions of specialty care costs revealed that the top 20% of patients with bipolar disorder accounted for 64% of total costs (
Table 3). This top 20% (by cost) of the bipolar group of patients (compared with the remaining 80%) were more likely to be women (92% versus 53%, p<.001), with more comorbidities (2.08 versus 1.34; p<.05), with diabetes being a predominant comorbidity. This group also had significantly more hospital admissions and hospital days (p<.05). Further conclusions are limited by a small sample size.
Discussion
Patients with bipolar disorder in this employee-sponsored, self-funded health care plan had significantly higher total health care utilization costs than patients with diabetes, depression, asthma, and coronary artery disease, and costs comparable to patients with diabetes. All of these conditions have been identified as areas of attention in practice redesign for the management of chronic health conditions. The only patient group who demonstrated a higher total cost was patients with both diabetes and coronary artery disease. This is in contrast to the results in the literature (
4) showing that medical disorders were more costly than bipolar disorder. We did not subdivide patients into the same categories, except for diabetes. It is interesting that in our analysis of the subgroup of patients with bipolar disorder with the highest costs, diabetes was one of the most common comorbidities. The numbers of patients became very small to expand this analysis.
The higher cost for bipolar disorder was primarily driven by psychiatric inpatient-outpatient utilization and pharmacy costs. Given the complexity of pharmacotherapy of bipolar disorder (
10), we would speculate that these pharmacy costs are likely also driven by psychiatry specialty practitioners. There is evidence that specialty care practitioners do not necessarily follow practice guidelines in the treatment of bipolar disorder (
11). Psychiatrists are also the only providers with inpatient psychiatric admission privileges in this care system. Closer examination of the medication history was not a part of this study, but no standardized practice or use of algorithm-based care of bipolar disorder was part of the delivery system.
In comparison, the cost of care for patients with depression in our data was characterized by higher primary care and nonpsychiatric hospitalization costs. Chronic care models for depression are often targeted at primary care practices, where the majority of depressed patients present. These data might suggest, in contrast, that models for bipolar disorder should be designed to include attention to specialty practices. In recent discussions about the patient-centered medical home, there are debates regarding the degree to which patients can meet the majority of their care needs in primary care. The cost of chronic illness care (including depression) delivered by a specialist that might be transferred into primary care has been examined, and it was found to be substantial (
12). The high inpatient and outpatient specialty costs for bipolar disorder noted in these data (
Table 2) suggest that bipolar disorder care may be even more challenging to move into a patient-centered medical home than depression and may require a more nuanced model that crosses primary care and specialty care boundaries.
Chronic care collaborative models have been shown to reduce utilization costs for depression (
13), and collaborative care models for bipolar disorder have also shown improvements in several outcomes while being cost neutral (
14). No such collaborative models were practiced for this patient population during the time of this review. A major barrier to the implementation of a collaborative model for bipolar disorder may arguably be found in our payment systems.
Payment models to date have often paid only for face-to-face visits, attempted to control costs by limiting access, and have sometimes carved out mental health costs from other medical costs. For collaboration to be evidenced around chronic illnesses like depression and bipolar disorder, new ways of reimbursing providers that encourage collaboration may be necessary. An example of an alternative pattern of reimbursement is described in the Depression Improvement Across Minnesota—Offering a New Direction (DIAMOND) project (
15). In this model, a bundled payment that targets services rendered in primary care by care managers includes the cost of supervision of these care managers by a consulting psychiatrist. In this way, the payment pulls the specialist and primary care provider together to manage the patient's chronic illness.
Finally, the skew in cost distribution for patients with bipolar disorder underlines the importance of paying attention to the small number of patients (in this study, mostly middle-aged women with comorbid medical conditions) who use a large percentage of services. An intervention aimed to manage bipolar patients may require special attention to mood issues in women and medical comorbidities. As mentioned previously, the most common comorbidity in this top (by cost) 20% of patients with bipolar disorder was diabetes. Many medications used in stabilizing mood have side effects associated with lipids, glucose, and body weight. With the pharmacy costs for bipolar disorder being higher than for any of the other chronic conditions reviewed here, attention to the metabolic implications of the pharmacotherapy of bipolar disorder—particularly for women—is recommended by these data. This observation supports literature recommending point-of-care screening for metabolic risk among patients receiving antipsychotics (
16). Guideline-based pharmacotherapy for bipolar disorder has been shown to be lacking in general practice (
10,
11).
Our study included only direct costs from health care utilization. The secondary cost to society of lost productivity for bipolar disorder is also impressive (
4). Coordinated and standardized care of patients with bipolar disorder that includes attention to primary and to specialty practices with adjustments made to address the utilization patterns of the highest cost outliers may demonstrate significant cost savings in primary and secondary costs. Finally, this type of review of costs is possible only when all costs for patients are under one roof. The process of “carving out” mental health costs from medical costs makes it impossible to appreciate the total costs of a group of patients with bipolar disorder or depression while providing perverse incentives in the delivery of care by financially discouraging health providers from collaborating around the best needs of those patients.
The findings from this study should be interpreted with caution because of the small sample size of patients with bipolar disorder and a single-payer population that may limit generalizability. There is also the concern that diagnoses were from administrative claims data and not established with the use of a structured interview. On the other hand, few studies follow the same cohort for several years, so this study may have advantages over cross-sectional studies in the stability of the diagnosis. Data from patients who did not remain continuously enrolled in the health plan for four years were excluded from the analytic sample. For this reason, some of the more seriously ill patients in any category might be missed. Finally, there is a potential of overlap in that patients other than those with bipolar disorder could be counted in more than one category. To minimize this concern, we focused on comparing only those other groups with the bipolar group (a group with relatively few comorbidities) and did not attempt to compare the groups with each other.
Finally, our study involved insured patients with a relatively high education background. It would be interesting to compare results with a broader sample of patients, including those on government plans or without insurance, to see how much these cost differences between chronic illnesses persist or vary.
Conclusions
The findings of this study highlight the high health care utilization costs of bipolar disorder. Compared with patients with depression, asthma, and coronary artery disease in this study, patients with bipolar disorder had higher total health care utilization costs, and their total costs were comparable with those of patients with diabetes. Health care utilization costs associated with bipolar disorder in this sample were driven mainly by psychiatric inpatient and outpatient care along with pharmacy costs. In contrast, the costs for patients with depression were concentrated in primary care and nonpsychiatric hospitalizations. In the design of models of health care homes where health care systems must manage the needs of a population of patients, there may be significant savings to health plans in attending to the needs of patients with bipolar disorder and in developing models of care that encourage collaboration between primary and specialty mental health providers with a shared set of cost and utilization information.
Acknowledgments and disclosures
Dr. Frye has received grant support from Pfizer, and he has been a consultant to Dainippon Sumittomo Pharma, Merck, and Sepracor. His continuing medical education has been supported by Astra-Zeneca, Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, Merck, Otsuka Pharmaceuticals, Pfizer, Sanofi-Aventis. The other authors report no competing interests.