The experience of homelessness is distressingly common among people with severe mental disorders and is of critical concern for mentally ill individuals, their families, and the professionals who treat them. Nonetheless, several fundamental questions about homelessness in this population remain unanswered.
Still unknown, for example, is the risk of homelessness in a representative sample of mentally ill persons. Although several studies have reported on the prevalence of homelessness among persons with severe mental disorders, they have employed atypical samples such as state hospital patients from inner city areas (
1,
2) and clinic outpatients (
3). Moreover, these studies were generally not conducted in the suburban and semirural areas where most Americans now live.
The present study addresses these questions by assessing the risk of homelessness in a quasi-representative sample of persons with psychotic disorders hospitalized for the first time in a large suburban and semirural county in Long Island, N.Y. We report the rates of homelessness both before initial hospitalization and during a 2-year period immediately after this episode. We compared the rates of homelessness among diagnostic groups and then, within a subgroup of patients with schizophrenia and related disorders, among differing symptom profiles.
METHOD
Subjects
The methods of the ongoing Suffolk County Mental Health Project have been described in detail elsewhere (
6). Briefly, liaisons in the county's 12 inpatient facilities attempted to refer to us all Suffolk County patients 15–60 years of age who had possible symptoms of psychosis and no history of psychiatric admission to any inpatient facility in the previous 6 months. Information about prior admissions was obtained from medical records, interviews with family members, and from individual subjects. Roughly 15 subjects (2.1%) who were referred for initial assessment were excluded after previously unknown hospitalizations were discovered.
After the procurement of subjects' written informed consent, those who were eligible were administered diagnostic and other assessments at initial evaluation and at 6- and 24-month follow-up. As detailed elsewhere (
6,
7), subjects could be lost at each step of this process, but the great majority of eligible patients were retained. This report is based on data from 237 patients who were hospitalized at 10 of the 12 facilities after a definite episode of psychosis (other than substance abuse, N=11) and for whom initial and 24-month follow-up assessments were completed.
Diagnosis
The instrument used to elicit symptoms for the diagnoses in this study was the Structured Clinical Interview for DSM-III-R (SCID) (
8), which was administered both at initial evaluation and at 6-month follow-up. Interviewers were clinically experienced master's-level health professionals trained to good reliability on the SCID over a period of 3–6 months (
6). After the second administration of the SCID at 6-month follow-up, two project psychiatrists reviewed all completed assessments and formulated a diagnosis together. Their diagnosis and the rationale for it were presented and debated in a diagnostic meeting of all investigators and coordinators. The consensus decision reached at this diagnostic meeting is the diagnosis employed in the present study.
The dimensions of positive and negative symptoms have been found to be useful descriptors of symptoms in schizophrenia and have been widely employed in both clinical and research settings (
9), including a study of homelessness among chronically mentally ill adults (
10). Positive symptoms include hallucinations and delusions, bizarre behavior, and thought disorder; negative symptoms include avolition, apathy, affective blunting, and social withdrawal. We explored whether higher levels of either positive or negative symptoms were associated with a greater risk of homelessness, since such symptoms might interfere with the maintenance of family and social ties felt to be crucial to avoiding homelessness. Positive and negative symptom profiles at baseline were rated with the Scale for the Assessment of Positive Symptoms (SAPS) and the Scale for the Assessment of Negative Symptoms (SANS) (
9), both of which have been widely employed in previous research. In our study, internal consistency reliabilities for the SAPS and SANS were adequate (alphas of 0.52 and 0.64, respectively).
Definition of Homelessness
We assessed homelessness both before entry into the study and during the follow-up period. Subjects were classified as having experienced antecedent homelessness if, at any time before their baseline interview, they considered themselves to have been homeless and they had, for at least one night, slept in a shelter, park, or abandoned building, in the street, or in a bus or train station because they had nowhere else to stay. Subjects were classified as having experienced follow-up homelessness if they met these criteria during the 24-month follow-up period after enrollment into the study. Subjects were classified as having experienced any early-course homelessness if they were found to have been homeless either before baseline or during the follow-up period. We also assessed lifetime duration of homelessness.
During the 24-month follow-up assessment, subjects who reported any previous homelessness were asked to estimate the total amount of time that they had been homeless during their lifetime. Response options were less than a week, more than a week but less than a month, more than 1 month but less than 6 months, more than 6 months but less than a year, and more than a year.
Data Analysis
We assessed separately the risk of antecedent homelessness, the risk of follow-up homelessness, and the risk of any early-course homelessness. We then compared the risk of antecedent, follow-up, and any early-course homelessness by demographic and diagnostic groups. Since the results were similar for all three homelessness measures, we present only the results for any early-course homelessness.
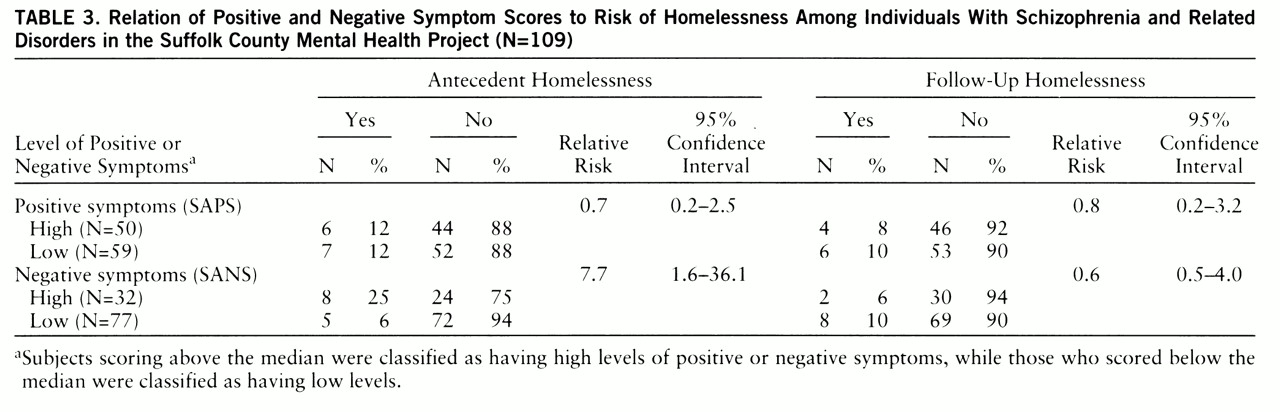
In analyses confined to the 109 subjects who were diagnosed with schizophrenia and related disorders (schizoaffective and schizophreniform disorder), we compared the risk of antecedent and follow-up homelessness among subjects with high versus low levels of positive and negative symptoms. Since the results differed, we present them separately. Scores on the SAPS ranged from 0.0 to 4.0 (mean=1.8, median=1.8, SD=0.9). Scores on the SANS ranged from 0.2 to 3.6 (mean=1.8, median=1.8, SD=0.8). Positive symptom scores above the median on the SAPS were classified as high, while scores below the median were classified as low. Similarly, negative symptom scores above the median score on the SANS were classified as high, and scores below the median were classified as low. Relative risks (odds ratios) were computed in separate logistic regression models in which the effect of high positive symptom scores was estimated while we adjusted for the effect of high negative symptom scores. In a similar fashion, the effect of high negative symptom scores was estimated while we adjusted for the effect of high positive symptom scores. We also tested for the presence of significant interactions between high positive and high negative symptom scores in predicting both homelessness outcomes.
RESULTS
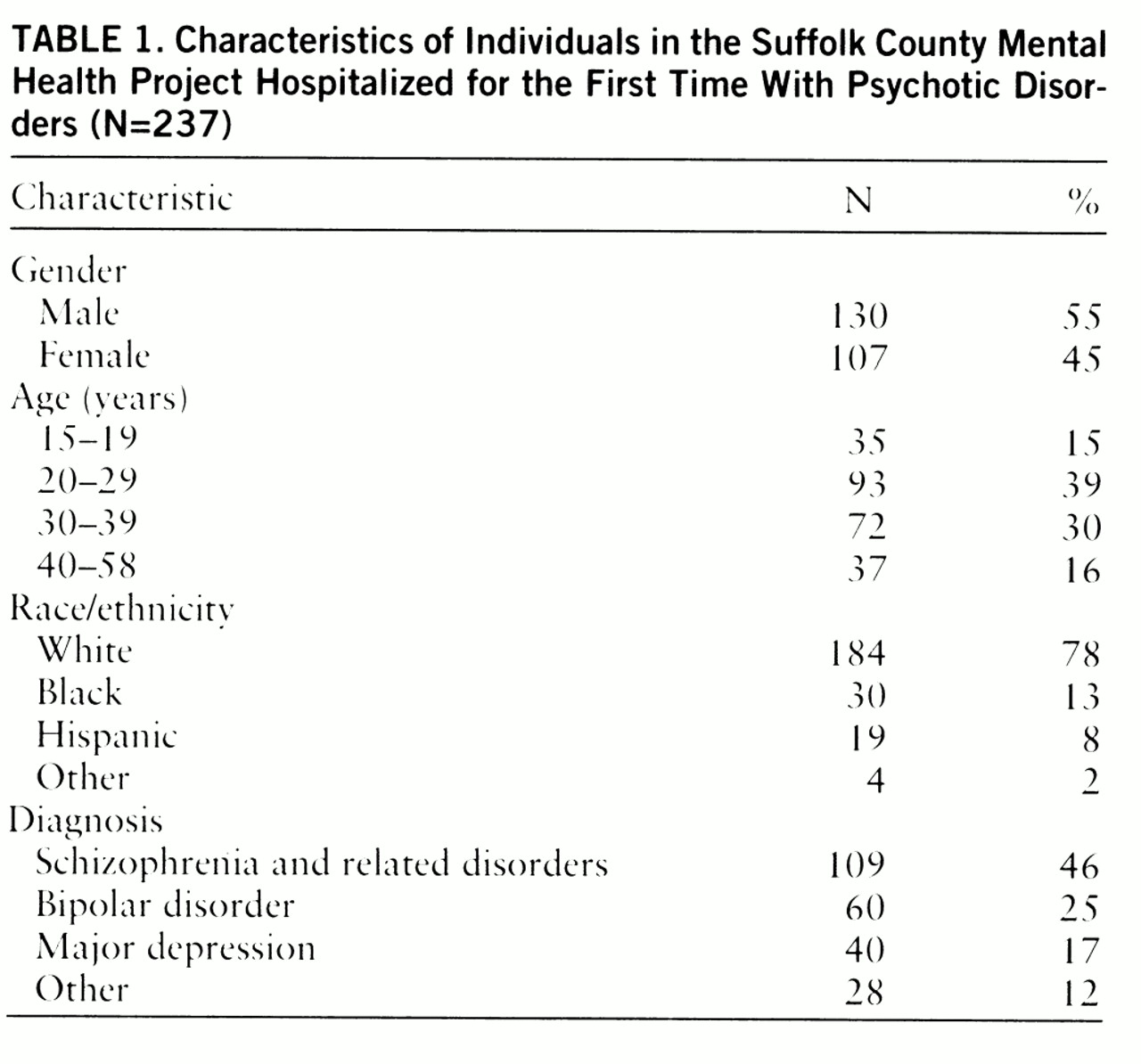
Table 1 provides the demographic and diagnostic characteristics of the participants in the Suffolk County Mental Health Project. The cohort was primarily male, white, and young (median age=28). Schizophrenia and related disorders (which included schizoaffective and schizophreniform disorders) were the most frequent diagnoses.
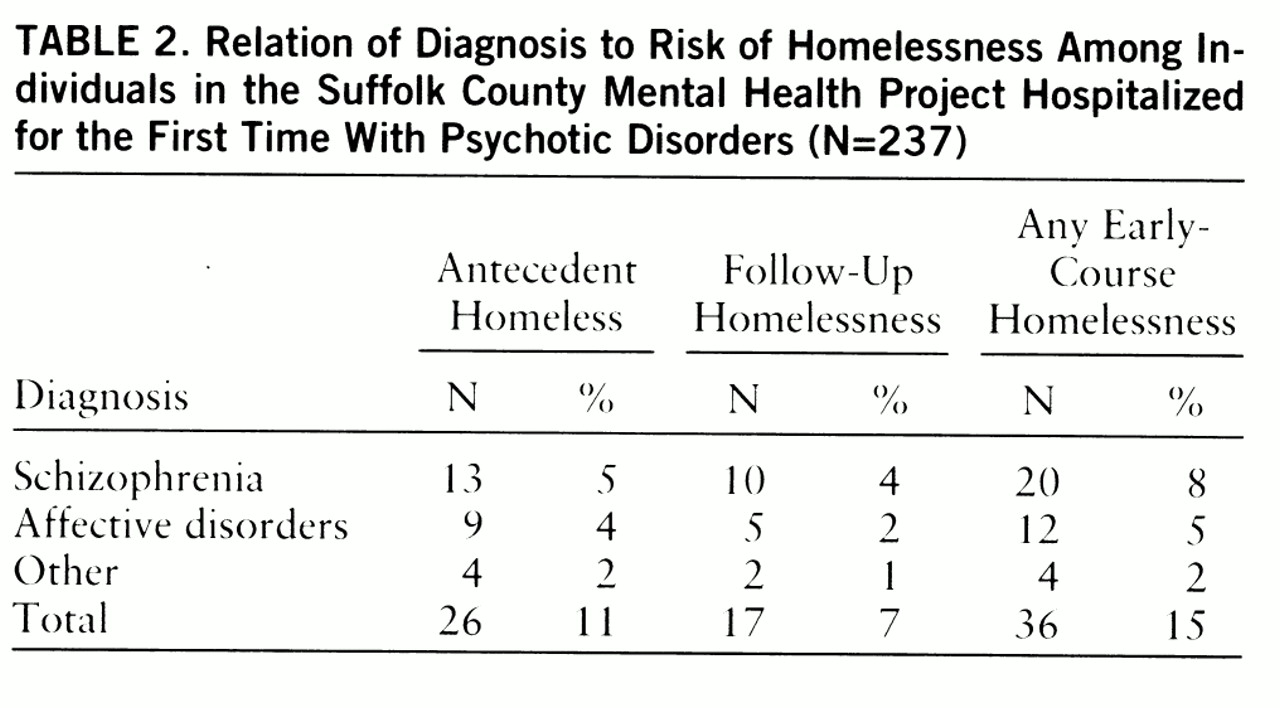
Table 2 presents the risk of antecedent homelessness, follow-up homelessness, and any early-course homelessness and gives these risks by diagnosis. Twenty-six subjects (11%) had been homeless before enrolling in the study, and 17 (7%) experienced homelessness during the 2-year period after enrollment. Thirty-six subjects (15%) reported any early-course homelessness. For most of these subjects, the duration of their homeless experience was substantial: 24 subjects had been homeless for more than 1 month during their lifetime, and eight had been homeless for more than 6 months.
The risk of early-course homelessness did not differ significantly among diagnostic groups (χ
2=1.7, df=3, p=0.65). Early-course homelessness also did not differ significantly between men and women (18% versus 12%, respectively; χ
2=1.4, df=1, p=0.24) or by age group (16% for those 30 or under versus 14% for those over 30; χ
2=0.2, df=1, p=0.70). Consistent with the findings of numerous other studies (
11–
14), black subjects were significantly more likely to experience early-course homelessness than were nonblack subjects (33% versus 13%, respectively; χ
2=8.8, df=1, p=0.003).
Table 3 compares the risk of antecedent and follow-up homelessness associated with positive and negative symptom profiles among subjects with schizophrenia and related disorders. The risk of antecedent homelessness was significantly greater among persons with high negative symptom scores than among those who did not score high on this scale. There was no significant association between positive symptoms and antecedent homelessness. Positive or negative symptoms were not significantly associated with follow-up homelessness. No significant interactions were found.
DISCUSSION
This is the first study of homelessness in a quasi-representative sample of persons with severe mental illness in a geographic area that is characteristic of where most Americans live. These data have documented among persons with psychiatric disorders an exceptionally high risk of homelessness early in the course of their illness. Moreover, in many cases the onset of homelessness preceded the first hospitalization and possibly influenced the course of illness from the earliest stages.
There were three main findings. First, 15% of this cohort of persons newly diagnosed with psychotic disorders had experienced at least one episode of early-course homelessness. This rate is surprisingly high given that subjects were young, were early in their course of illness, and were recruited primarily from nonurban areas. The observed risk of lifetime homelessness is roughly five times the age-adjusted estimated risk of lifetime homelessness in the U.S. population (
15).
Second was the unexpected finding that over two-thirds of those who reported early-course homelessness experienced their initial homeless episode before their first psychiatric hospitalization. This suggests that, for many persons with psychotic disorders, homelessness cannot be simply attributed to poor hospital discharge planning, since initial homelessness in most cases preceded contact with the inpatient system. This observation is consistent with the results of previous research (
16), which interpreted such evidence as supporting the hypothesis that homelessness could itself be a cause of mental illness. On the other hand, a review of selected case narratives and family reports for subjects in our study revealed that prehospitalization homelessness often appeared to first occur during the prodromal phase of disease onset, when social and occupational functioning were already substantially impaired.
For example, a black, 30-year-old man who worked in an office setting became romantically fixated on a co-worker, which resulted in police involvement. Eventually an order of protection was issued against him, which led to loss of employment, eviction for nonpayment of rent, and homelessness. He was ultimately referred to initial inpatient treatment by staff of the homeless shelter in which he was staying. Another subject was a white, 23-year-old man who had been hospitalized for the first time because of command hallucinations. At age 17, he had suddenly become withdrawn and had begun to exhibit violent behavior and dropped out of high school. He moved out of his family's home and soon became homeless for several months. He eventually enlisted in the armed forces from which he was discharged after a violent incident. A white, 34-year-old woman was referred for hospitalization from a shelter for homeless mothers after neglecting her infant and assaulting staff. According to her mother, this woman first began hearing voices 5 or 6 years earlier but had never received treatment. These examples suggest that, at least in some individuals, their developing illness may have contributed to their becoming homeless (
17). They also demonstrate that the mental health treatment system frequently fails to detect cases of psychosis until a considerable degree of social dysfunction has already occurred.
The third finding concerns the possible relationship between type and symptoms of illness and homelessness risk. There were no significant differences in the risk of homelessness among diagnostic groups. This result, which agrees with data previously reported (
2), implies that one or more general factors associated with severe mental disorder, rather than disorder-specific manifestations, play a key role in imparting risk of homelessness. Such general factors might include limited income related to unstable work history, reduced levels of family support, and impaired social networks.
Within the subgroup of subjects diagnosed with schizophrenia and related disorders, we found that those assessed as having high negative symptom scores at baseline were at significantly higher risk for antecedent (but not follow-up) homelessness than were those with lower negative symptom ratings. There are several plausible explanations for this finding. High levels of negative symptoms disrupt family relationships and other sources of social support that are thought to be important in preventing mentally ill individuals from becoming homeless. On the other hand, the direction of causality is ambiguous, since the experience of homelessness itself could, in part, account for the observed symptom ratings. Finally, patients with high levels of negative symptoms may have had longer periods of disturbance before hospitalization, thereby placing them at risk for longer periods of time.
There were several important limitations to this study. First, since our measure of homelessness was based upon subject self-reports, the estimated rates of homelessness are likely to be biased downward. Because of problems of recall, respondents may have failed to report episodes of homelessness, particularly those that preceded entry into the study or those that were of relatively brief duration.
Second, the study included only hospitalized persons. A homeless person who exhibits the same symptoms of mental disorder as a domiciled person may be more likely to be hospitalized, since by virtue of being homeless, he or she would be more likely to come to the attention of the police and other public authorities. The rates of homelessness we observed may be biased upward by this factor.
Third, while we called this study group a quasi-representative sample, it did not include patients hospitalized at two of the 12 facilities in the county. These two private, for-profit hospitals did not agree to participate at the time the study began.
A final caution concerns the generalizability of these findings. We studied patients with psychoses only. Persons with other significant mental disorders, such as nonpsychotic affective disorders and posttraumatic stress disorder, were excluded from the study.