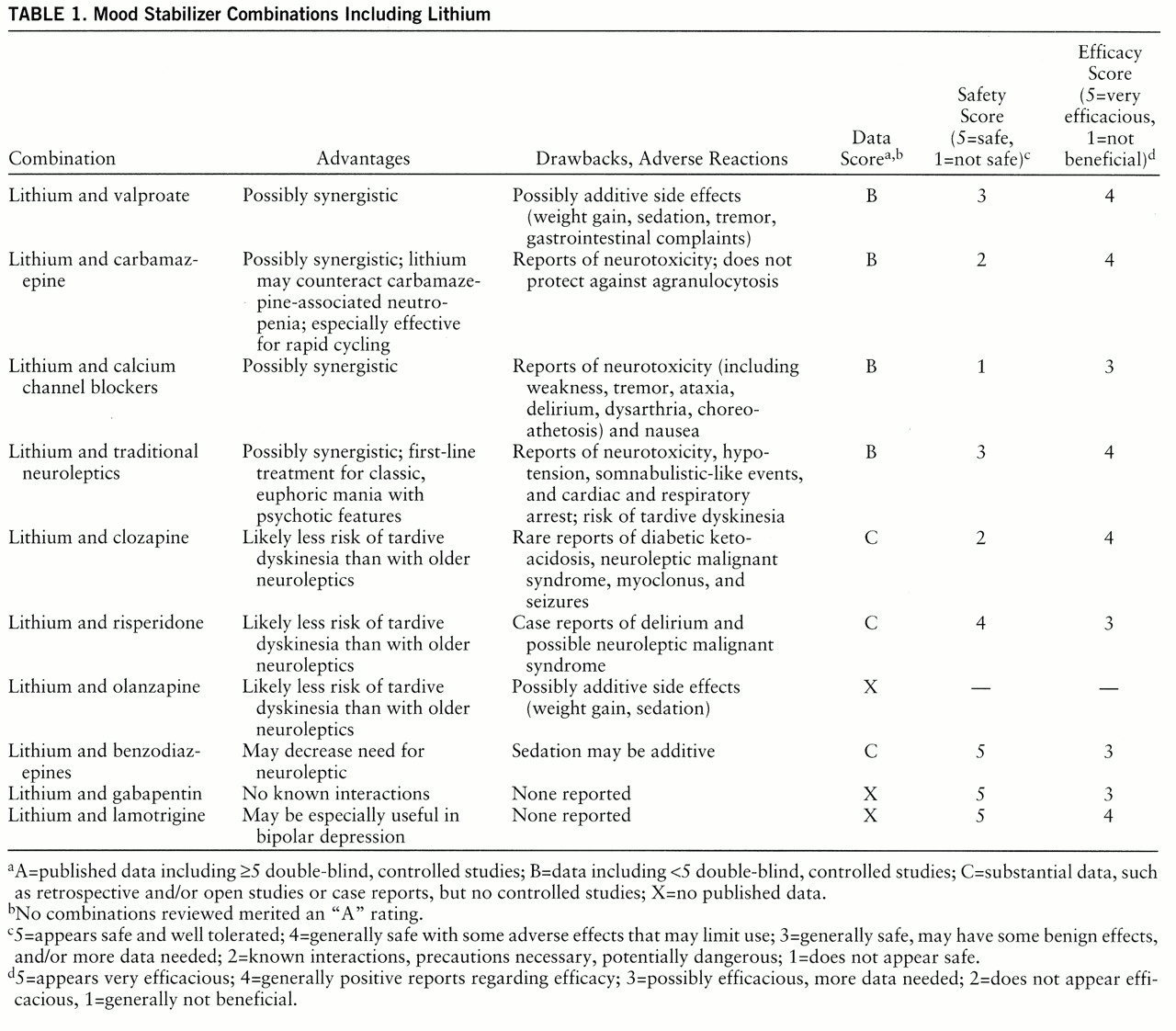
Combinations With Lithium (table 1)
Lithium and valproate. The use of the combination of lithium and valproate is gaining favor, and it appears to be a safe and effective regimen. Use of valproate, both as monotherapy and in combinations, has increased substantially over the past 5 years (
3). As reported in the consensus guideline for bipolar disorder (
2), the addition of valproate to lithium has been recognized as a first-line treatment for mania that is refractory to lithium monotherapy, and conversely, the treatment of choice for acute mania with partial but inadequate response to valproate is the addition of lithium. Generally, the addition of valproate is most effective for patients with rapid cycling or mixed episodes. In one recent placebo-controlled double-blind study (
4), patients receiving a combination of lithium and valproate were significantly less likely to suffer a relapse than were patients receiving lithium and placebo. The study involved 12 patients followed for a minimum of 14 weeks, and most patients were followed for 1 year. In open-label (
5) and retrospective (
6) studies, this combination was effective in both the manic and depressive phases of the illness. Single case reports (
7,
8) also support the efficacy of lithium and valproate together, especially for rapid cycling.
Lenox et al. (
9) suggested that the combination of lithium and valproate may be synergistic. They found that the combination produced additive suppression of the protein myristoylated alanine-rich C kinase substrate.
Safety was examined in a controlled crossover trial (
10) in which lithium was administered to 16 patients receiving either divalproex sodium or placebo. Lithium's pharmacokinetics were found to be unchanged by valproate, and there was no significant difference in adverse events reported by the valproate and placebo groups.
Potential drawbacks to concurrent treatment with lithium and valproate include additive adverse reactions, such as weight gain, sedation, gastrointestinal complaints, and tremor. Overall, on the basis of the available data, the combination of lithium and valproate appears to be well tolerated and effective in treating bipolar illness.
Lithium and carbamazepine. The use of carbamazepine for bipolar disorder is declining because of the difficulties generated by carbamazepine's pharmacokinetic interactions with other medications, its side effects, and the rising popularity of valproate (
3). However, the concurrent use of lithium and carbamazepine is still common. As reported in the consensus guideline for bipolar disorder (
2), almost one-half of the recognized experts consider the addition of carbamazepine to lithium a first-line treatment for mania refractory to lithium monotherapy.
The available data suggest that the combination of lithium and carbamazepine is safe and effective, especially for rapid-cycling patients. Di Costanzo and Schifano (
11) reported a retrospective examination of 16 rapid-cycling patients given lithium either alone or in combination with carbamazepine. Improvement was noted earlier in the group receiving both lithium and carbamazepine than in the patients receiving lithium monotherapy. Lithium and carbamazepine may work synergistically. Kramlinger and Post (
12) observed improvement in seven manic patients receiving carbamazepine (who previously had not responded to lithium monotherapy) with the double-blind addition of lithium. Small et al. (
13) reported giving neuroleptic or carbamazepine under blind conditions to 33 patients taking lithium; after 8 weeks both groups improved clinically, but the carbamazepine-lithium combination was tolerated better.
Furthermore, in a retrospective study of 18 patients conducted in 1992 (
14), those receiving both lithium and carbamazepine experienced better prophylaxis against bipolar episodes than patients treated with either medication alone, and the addition of carbamazepine allowed patients to function better while maintaining lower lithium levels. Also, in a prospective study (
15) of 14 patients with lithium-resistant bipolar disorder, treatment with the combination of lithium and carbamazepine for 1 year was superior to treatment with lithium and neuroleptics in the nine patients completing the study. Several other anecdotal reports (
16–
19) suggest that the combination of lithium and carbamazepine is effective and perhaps synergistic. Besides efficacy, another advantage noted in the literature is that lithium may counteract carbamazepine-induced leukopenia, although the clinical significance of this phenomenon is unclear (
19–
21).
Cases of neurotoxicity and asterixis have been reported with the concomitant use of lithium and carbamazepine (
22,
23). Patients with preexisting CNS disease may be especially vulnerable to negative outcomes with this combination (
24). Generally, most of the available data suggest that the combination of lithium and carbamazepine is safe and effective, but use of this combination for patients with comorbid CNS disease should be avoided.
Lithium and calcium channel blockers. It is advisable to use caution when combining lithium and calcium channel blockers. Multiple cases of toxicity, particularly neurotoxicity, have been reported (
25–
27). Also, Dubovsky et al. (
28) reported two cases of severe bradycardia in elderly manic patients taking lithium and verapamil concomitantly.
Verapamil administration may decrease the serum lithium level by increasing excretion, potentially increasing the risk of relapse (
29). The risk of neurotoxicity may be greater with verapamil and diltiazem and less with nifedipine, possibly owing to differences in interactions with calcium channels, metabolism, and/or ability to cross the blood-brain barrier (
26,
27). Although possibly effective (
30), lithium and calcium channel blockers in combination may be hazardous.
Lithium and traditional neuroleptics. Lithium is frequently used with neuroleptics. For patients with classic, euphoric acute mania with psychotic features, most experts consider the combination of a high- or medium-potency neuroleptic with lithium to be a first-line treatment (
2). Substantial controversy exists in the literature regarding the safety of such combinations.
There have been only two controlled studies of the use of lithium with neuroleptics. Small et al. (
13) reported giving neuroleptic or carbamazepine under blind conditions to 33 patients taking lithium; after 8 weeks both groups improved clinically, but poorer tolerance of the neuroleptic-lithium combination was noted. In another study, Esparon et al. (
31) reported a double-blind comparison of depot flupenthixol and placebo for 11 bipolar patients taking lithium. Over the course of 2 years, it was concluded that the neuroleptic provided no prophylactic effect.
A number of prospective and retrospective studies (
32–
40) support the safety of lithium in conjunction with traditional neuroleptics. There are also case reports suggesting the clinical benefits of combining a neuroleptic and lithium, and synergism between lithium and neuroleptics has been suggested anecdotally (
41,
42).
In contrast, there is also substantial evidence of adverse reactions to such combinations. These mainly consist of neurotoxicity. In one study (
43), delirium, extrapyramidal signs, and cerebellar dysfunction were reported in three of five elderly bipolar patients receiving lithium and neuroleptics. In another study (
35), two of 30 patients receiving lithium and a neuroleptic developed severe tremor. Cases in which use of lithium combined with a neuroleptic resulted in severe neurotoxicity, such as delirium, seizures, tardive dyskinesia, encephalopathy, or EEG abnormalities, have been reported, as have hypotension and cardiac arrhythmias (
44–
52). However, Krishna et al. (
34) reported that neurologic symptoms are usually mild and resolve with discontinuation of medication. Given the possibility of long-term treatment, use of lithium in combination with neuroleptics may increase the risk of tardive dyskinesia (
53,
54).
Goodwin and Jamison (
55) emphasized that 1) the risk of neurotoxicity appears to be higher in patients with preexisting encephalopathy, 2) neuroleptics should be used in lower doses when combined with lithium, and 3) lithium levels should be maintained below 1.0 meq/liter when lithium is used with neuroleptics. Thus, as concomitant lithium and neuroleptic administration is widespread and generally effective, care should be used to minimize the risk of neurotoxicity.
Lithium and clozapine. Clozapine has been gaining acceptance as a highly effective mood stabilizer for refractory illness, both as monotherapy (
56–
61) and with other medication. Clozapine and lithium in combination have been reported anecdotally to be effective for refractory bipolar disorder (
62–
64).
However, the combination of lithium and clozapine has been reported to cause neurologic symptoms (
65–
67). Also, one case each of diabetic ketoacidosis (
68) and neuroleptic malignant syndrome (
69) associated with this combination has been reported. Although lithium may be helpful in counteracting clozapine-induced leukopenia (
70), it will not prevent agranulocytosis (
71).
The few available data include reports of both clinical improvement and adverse events. More study of this combination is needed before assertions of safety or efficacy can be made.
Lithium and risperidone. Tohen et al. (
72) studied risperidone in combination with mood stabilizers in the treatment of mania. They found that for eight of 12 patients the combination of risperidone and lithium was well tolerated and efficacious. Also, safety and efficacy were noted in a retrospective study (
73), in which nine patients were treated with this combination. The authors of this study did not differentiate between adverse reactions occurring with risperidone monotherapy and those associated with polypharmacy, and so the drawbacks of these specific treatments cannot be inferred.
In contrast to the relative safety observed by Tohen et al. (
72), cases of fever, high creatine phosphokinase levels and WBC counts, and delirium have been reported by others (
74,
75). Therefore, caution should be exercised when using lithium and risperidone in combination.
Lithium and olanzapine. To our knowledge there are no published data at this time regarding this combination. Side effects (e.g., weight gain, sedation) may be additive.
Lithium and benzodiazepines. Although probably not effective as monotherapy for the long-term treatment of bipolar disorder (
76), benzodiazepines are frequently used in combination with lithium. Combinations of lithium and benzodiazepines are generally well tolerated and effective. This is especially important in the consideration of the potential dangers of combining lithium and neuroleptics, as discussed earlier. For example, Sachs et al. (
77,
78) reported that for some patients previously receiving both lithium and a neuroleptic, clonazepam successfully replaced the neuroleptic. Also, Adler (
79) reported successful use of lithium and clonazepam to treat mania in a patient with neuroleptic malignant syndrome, which resolved after clonazepam treatment was started in place of the neuroleptic. Lorazepam has also been studied in combination with lithium. In an open study (N=4), Modell et al. (
80) found the combination of lithium and lorazepam to be rapidly effective and safe for acute mania.
In contrast, Koczerginski et al. (
81) described five cases in which the combination appeared to cause neurotoxicity, specifically ataxia and dysarthria. Also, long-term benzodiazepine use may be problematic for some patients with comorbid substance abuse.
Overall, the concomitant use of lithium with benzodiazepines appears effective and safe, may decrease the need for neuroleptics, and may treat comorbid anxiety.
Lithium and gabapentin. Gabapentin is currently being studied as a treatment for bipolar disorder, and there have been favorable reports regarding its potential as a mood stabilizer (
82,
83). The advantages of gabapentin include the lack of interactions with other drugs in the cytochrome P450 system and the lack of protein binding (
84). Since there is little risk of drug interactions, use with lithium is likely to be safe. The combination of lithium and gabapentin seems to be a reasonable treatment for patients with refractory illness.
Lithium and lamotrigine. The combination of lithium and lamotrigine appears promising for the treatment of bipolar disorder. Anecdotal reports (
85) suggest that it may be especially helpful in cases of bipolar depression. In an open trial conducted by Calabrese et al. (
86), after 12 months lamotrigine appeared to be both well tolerated and effective as monotherapy (N=17) and in combination with other mood stabilizers (N=50). Hence, lithium and lamotrigine in combination may be a rational regimen, but more data are needed.
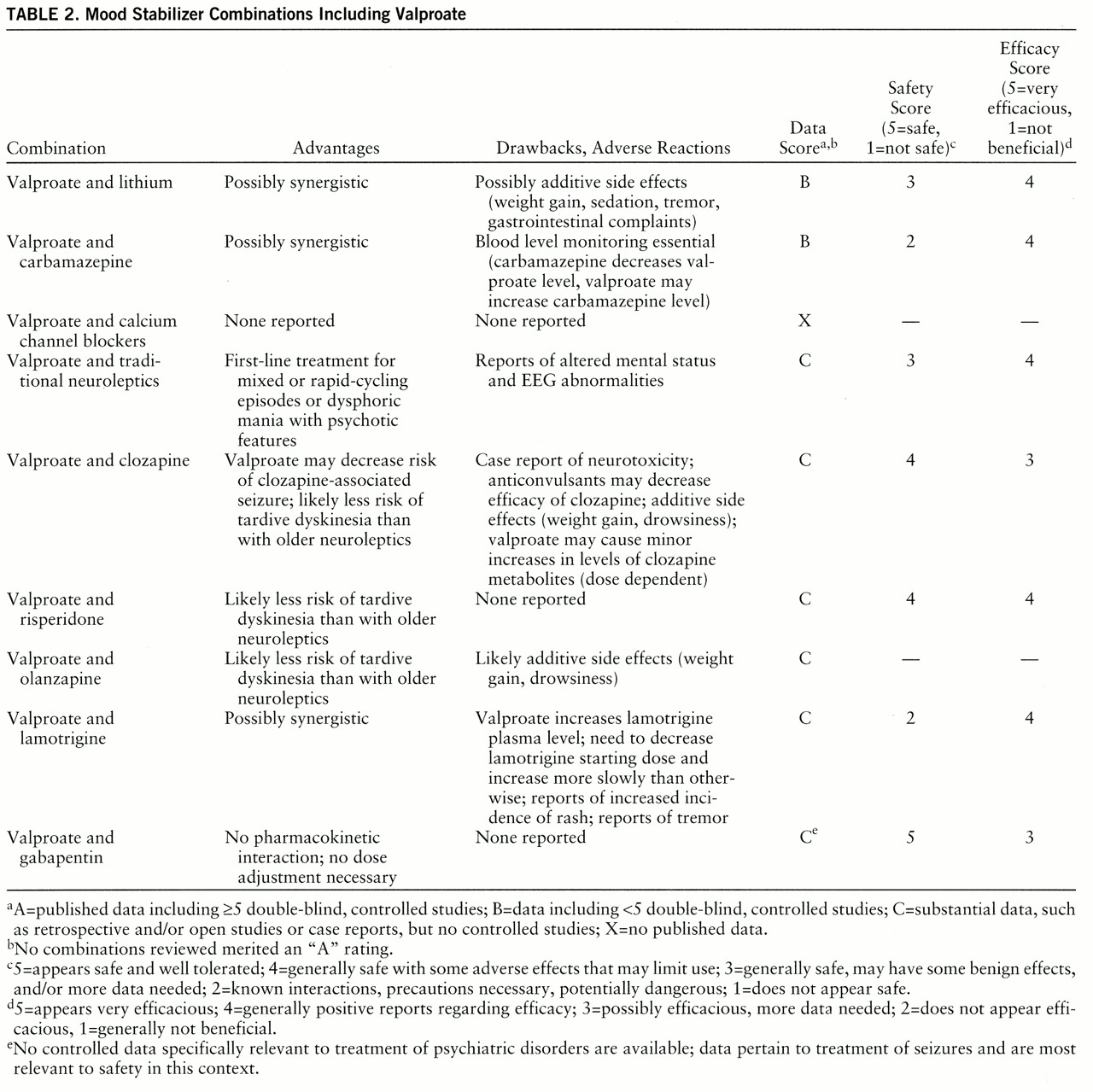
Combinations With Valproate (table 2)
Valproate and lithium. See the previous discussion of the combination of lithium and valproate in the Combinations With Lithium section.
Valproate and carbamazepine. While the combination of valproate and carbamazepine has been generally found to be effective, its safety has been questioned. When Schaff et al. (
6) gave divalproex sodium to patients taking carbamazepine, improvement was observed in 69% of patients who had failed to respond to carbamazepine alone (N=29). Tohen et al. (
87) studied pharmacy records of patients treated with both medications simultaneously and found that all 12 of the bipolar disorder patients studied had moderate to marked responses, while only two patients had minor side effects.
A synergistic effect was suggested by Ketter et al. (
88), who described a case of rapid-cycling bipolar disorder that had been refractory to both valproate and carbamazepine monotherapy but under double-blind conditions responded dramatically to the combination.
However, blood levels of these anticonvulsants must be monitored closely. Carbamazepine induces metabolism of both itself and valproate via the cytochrome P450 3A3/4 system, which may decrease the serum concentrations of both drugs and increase the risk of relapse (
89,
90). Therefore, large doses of valproate are often necessary when used with carbamazepine. In addition, valproate may moderately inhibit the metabolism of carbamazepine and displace protein-bound carbamazepine and in some cases increase levels of free carbamazepine. This drug-drug interaction may result in neurotoxicity, even when valproate levels are relatively low (
91).
Therefore, hazards exist with concomitant valproate and carbamazepine use. This treatment may be highly efficacious, but diligent monitoring of blood levels is required to reduce risk.
Valproate and calcium channel blockers. We found no published data regarding valproate and calcium channel blockers in combination, although one of us (A.L.S.) has used this combination on several occasions with moderate success and without adverse effects.
Valproate and traditional neuroleptics. For patients with mixed or rapid-cycling episodes or dysphoric mania with psychotic features, most experts consider the combination of a high- or medium-potency neuroleptic and valproate a first-line treatment (
2). Wassef et al. (
92) reported efficacy in treating psychosis in two schizophrenic patients and one schizoaffective patient, who responded dramatically to the combination of valproate and neuroleptics. Van Sweden and Van Moffaert (
93) reported four cases of encephalopathy resulting from the concurrent administration of valproate and neuroleptics. Although combined use of valproate and traditional neuroleptics is widespread and may be a sensible treatment approach, more definitive studies are needed.
Valproate and clozapine. Presently, the data concerning the combination of valproate and clozapine are variable. In one open-label study of 55 patients (
94), this combination was effective for 87% of the patients. The most common adverse reactions were sedation, enuresis, nausea, excessive salivation, and benign increase in liver function tests. One patient developed subsequent hepatic dysfunction. Conflicting reports suggest that valproate may slightly increase the serum concentrations of clozapine metabolites (
95) or decrease concentrations of clozapine and metabolites (
96). Furthermore, a case of neurotoxicity after several months of treatment with this combination has been described (
97). In an uncontrolled study, Wilson (
98) retrospectively examined records of sequential patients who received clozapine for refractory psychosis and concluded that concomitant anticonvulsant administration may decrease the efficacy of clozapine. The 20 patients receiving concurrent anticonvulsant treatment were judged to have poorer clinical outcomes than the 68 patients who did not receive anticonvulsants.
At this time, the efficacy and safety of this combination are not established. Clozapine lowers the seizure threshold, so adding valproate can prevent associated seizures. Both drugs exhibit antikindling properties, raising intriguing questions about epileptogenesis and mood stabilization (
99). Hence, more data regarding combination treatment with valproate and clozapine are needed.
Valproate and risperidone. Data regarding the combined use of valproate and risperidone are scarce. In two studies that examined this issue, the investigators did not differentiate efficacy and adverse reactions occurring with risperidone monotherapy from those associated with several different combinations of mood stabilizers and risperidone. Advantages and drawbacks of specific combinations are difficult to infer, but Ghaemi et al. (
73) rated three of four patients treated with a combination of risperidone, lithium, and valproate as “much improved.” Tohen et al. (
72) reported that in their study two patients treated with a combination of risperidone, valproate, and lithium were able to complete the 6-week study, and they stated that no patients who completed the study worsened clinically. The data regarding the combination of valproate with traditional neuroleptics, described earlier, may also be applicable to the combination of risperidone and valproate.
Valproate and olanzapine. To our knowledge there are no published data at this time regarding this combination. Side effects (e.g., weight gain, sedation) may be additive.
Valproate and lamotrigine. Most of the known information about the combination of valproate and lamotrigine is based on use with seizure patients. Most important, concomitant valproate treatment substantially increases the blood level of lamotrigine (
100,
101) because of the inhibition of glucuronidation. Adverse reactions, particularly skin rash, may occur with greater frequency or severity. Other side effects that may occur are ataxia, tremor, sedation, and fatigue (
100–
105). However, such symptoms should improve as the dose of lamotrigine is decreased (
102,
103). Also important, when lamotrigine is added to valproate therapy, valproate concentrations may be possibly decreased (
106).
Specifically concerning bipolar disorder, in the previously mentioned open study by Calabrese et al. (
86), valproate plus lamotrigine was used (N=18), and preliminary results indicate efficacy. Six of the eight patients who dropped out because of adverse events experienced rash, a finding that emphasizes the need to monitor patients receiving this combination closely for dermatologic side effects.
In summary, the combination of valproate and lamotrigine may be highly effective, but extreme caution is warranted. The most troubling factor is the increased risk of serious dermatologic reactions. Hence, the combination of valproate and lamotrigine may be a rational treatment if patients are adequately informed about the risks of adverse reactions, low doses of lamotrigine are used, and lamotrigine is discontinued at the onset of severe rash or rash with systemic symptoms.
Valproate and gabapentin. Valproate and gabapentin in combination require further study, as few data are currently available. These agents appear to be safe together and to have no major interactions, and no adverse reactions have been reported (
107). Hence, no dose adjustment or additional serum blood level monitoring is indicated. Efficacy for bipolar disorder patients is not yet established for gabapentin monotherapy, but the combination of valproate and gabapentin may be a reasonable treatment approach for patients with refractory illness.
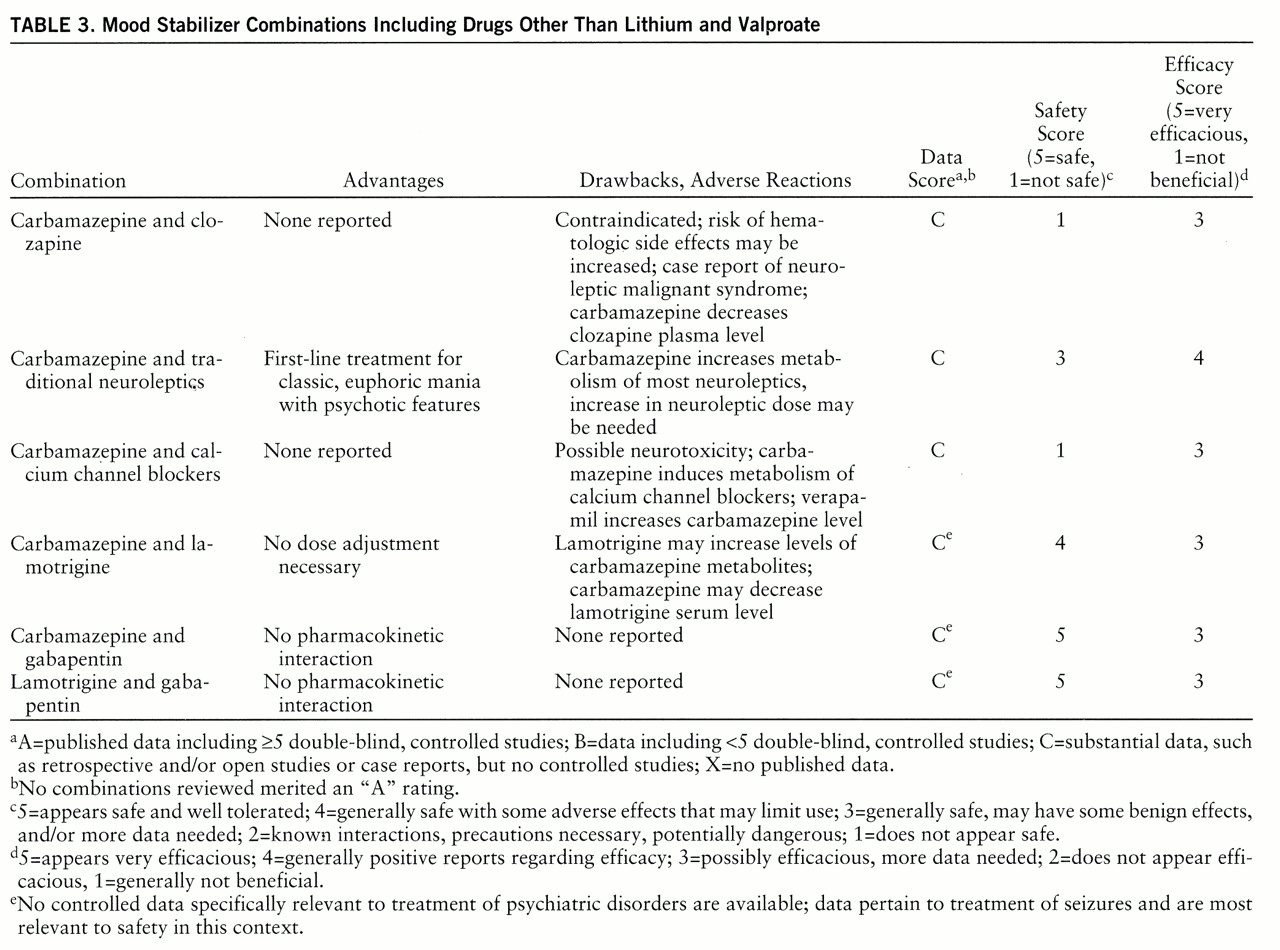
Other Combinations (table 3)
Carbamazepine and clozapine. The combination of carbamazepine and clozapine is generally contraindicated. First, carbamazepine and clozapine each produce hematologic side effects at higher frequencies than do most other available drugs (
108). Another consideration is that carbamazepine lowers the level of clozapine, possibly more than it lowers levels of traditional neuroleptics (
109,
110).
Raising further questions regarding safety, Müller et al. (
111) reported a case of neuroleptic malignant syndrome in a patient taking clozapine and carbamazepine. Asterixis has also been reported (
23).
The combination of carbamazepine and clozapine should not be considered safe. Therefore, careful consideration of risks and benefits is mandatory before a regimen of this combination is begun. Should carbamazepine and clozapine be used together, vigilant monitoring of the WBC count and drug levels is crucial.
Carbamazepine and traditional neuroleptics. For patients with classic, euphoric acute mania with psychotic features, the combination of a high- or medium-potency neuroleptic and carbamazepine is considered by most experts to be a first-line treatment (
2).
As stated earlier, carbamazepine increases the metabolism of most neuroleptics. The levels of traditional neuroleptics are decreased by the induction of their metabolism by carbamazepine. This can lead to a recurrence of psychiatric symptoms, as seen in case reports (
112,
113).
Therefore, the simultaneous use of carbamazepine and traditional neuroleptics can be considered useful for bipolar disorder. Increasing the neuroleptic dose may be necessary to achieve therapeutic gains. More studies would be helpful in establishing safety and efficacy.
Carbamazepine and calcium channel blockers. Carbamazepine and calcium channel blockers should be used together with extreme caution. Both diltiazem and verapamil have been shown to increase levels of carbamazepine (
114,
115). Toxicity has been reported, most often in the form of neurologic symptoms. In one study (
116), six patients with epilepsy were given concurrent verapamil and carbamazepine, and within a few days all experienced neurotoxicity. In another study of seizure patients (
117), toxicity was seen with carbamazepine in combination with diltiazem and verapamil, but not with nifedipine.
Hence, carbamazepine and calcium channel blockers should be used together with caution. Different calcium channel blockers may pose distinct risks of neurotoxicity with carbamazepine, but combined use of carbamazepine and any calcium channel blocker should be considered potentially hazardous.
Carbamazepine and lamotrigine. Carbamazepine likely speeds the metabolism of lamotrigine, but the clinical significance is unclear. In children with seizure disorders, adjustments of carbamazepine dose were not necessary when lamotrigine was added (
101). Although one study of the pharmacokinetics (
118) has shown that lamotrigine has no effect on the metabolism of carbamazepine, another study (
119) showed that lamotrigine increased carbamazepine metabolite concentrations by 45% and resulted in neurotoxicity.
In a study of bipolar patients mentioned earlier (
86), both lamotrigine monotherapy and combination therapy have appeared effective and well tolerated, and one group received concomitant lamotrigine and carbamazepine (N=6).
As the data are contradictory, more study is required to assess the safety and efficacy of concurrent treatment with lamotrigine and carbamazepine, but these two agents have less significant pharmacologic interactions than do lamotrigine and valproate.
Carbamazepine and gabapentin. As with valproate, the coadministration of carbamazepine with gabapentin appears safe, with no significant interactions (
107). Hence, dose adjustments and additional blood level monitoring are not necessary. The combination of carbamazepine and gabapentin has not been established as efficacious in bipolar disorder, but to our knowledge no adverse reactions have been reported to date. At this time, concurrent carbamazepine and gabapentin treatment appears benign and may be reasonable in treating refractory bipolar disorder.
Lamotrigine and gabapentin. Our search revealed no published data regarding the coadministration of lamotrigine and gabapentin in bipolar disorder. To our knowledge no adverse reactions have been reported with concurrent use for epilepsy patients. One of us (A.L.S.) has eight patients with refractory bipolar disorder who are taking the combination of lamotrigine and gabapentin with satisfactory results.