When do personality disorders begin, and how do they develop? Current clinical thinking (DSM-IV) suggests that they are enduring patterns with an onset in adolescence or early adulthood. However, there are surprisingly few data that speak to these assumptions. Questions concerning the prevalence and longitudinal vicissitudes of personality disorders can be addressed in several ways. The most valid answers will likely come from assessing large epidemiologic nonclinical and clinical-epidemiologic samples followed repeatedly across developmental periods. Korenblum and colleagues (
1) assessed a nonclinical sample of adolescents at ages 13, 16, and 18. Forty-two percent of the sample displayed some degree of personality dysfunction, and roughly 33% showed evidence of dysfunction at all three assessment points. Cluster C personality disorders seemed to decrease in frequency with increasing age. Bernstein and colleagues (
2) followed a community sample of 733 subjects aged 9 to 19 over a 2-year period. The prevalence of personality disorders peaked during early adolescence, declined sharply during middle adolescence, and leveled off during late adolescence. To our knowledge, no study has been reported that has tracked personality disorders across the major developmental eras of adolescence into adulthood.
Clues toward understanding the onset and prevalence of personality disorders can also be obtained by comparing independent samples from different developmental eras assessed cross-sectionally. One important advantage to this type of design is that frequency estimates can be arrived at by using similar diagnostic criteria at one time point. This is important given that changing sociocultural factors can influence nosological usage and criteria over time. The present study examined the frequency of personality disorders during adolescence and early adulthood in a clinical study group of consecutively admitted inpatients, through the use of structured diagnostic interviews. We tested for differences in frequency during the two age periods to obtain a first approximation of the evolution of these disorders.
METHOD
Subjects were a consecutive series of 255 patients admitted to a private, not-for-profit, tertiary care psychiatric hospital. Patients were admitted on the basis of need for inpatient-level psychiatric treatment (Global Assessment of Functioning [DSM-IV] ratings at the time of admission averaged 36.4 [SD=9.2]); no other selection processes were used. One hundred thirty-seven (53.7%) of the subjects were male, 227 (89.0%) were Caucasian, most were middle-class (70% from families in Hollingshead-Redlich [3] social classes II–IV), and all had third-party insurance coverage.
Of the 255 patients admitted, 138 were adolescents aged 12 to less than 18 years (mean=15.5, SD=1.4), and 117 were young adults aged 18 to 37 years (mean=23.6, SD=5.6). The two study groups did not differ significantly in gender or in parental socioeconomic status. The adult group had a significantly higher proportion of Caucasian patients (96.6%, N=113) than the adolescent group (82.6%, N=114) (Yates's continuity-corrected χ2=12.65, df=1, p<0.001, two-tailed test).
Subjects were given the Personality Disorder Examination (
4) to assess for the presence of DSM-III-R personality disorders. Subjects were judged to meet specific criteria of the Personality Disorder Examination if personality dysfunction had been pervasive and persistent for at least 5 years for adults and 3 years for adolescents, as in previous work (
4). The duration specifications of the Personality Disorder Examination represent more stringent criteria than those of either DSM-III-R or DSM-IV; the latter specifies a 1-year duration criterion for persons under 18 years of age. Antisocial personality disorder was not diagnosed in the adolescent patients because of the DSM-III-R criterion requiring an age of at least 18 years. The structured interviews were performed soon after admission by a trained and monitored research evaluation team that functioned independently from the clinical teams. Interviewers were blind to the study's aims. All subjects (and the parents of adolescents) provided written informed consent.
Diagnoses were reliably assigned. Kappa coefficients for interrater reliability (based on tests of independent simultaneous ratings by pairs of raters) across all diagnoses ranged from 0.65 to 1.0 (average kappa=0.84). Final research diagnoses were established by the “best-estimate” method, based on the structured interviews and any additional relevant medical record data, in accordance with the Longitudinal Expert All Data standard (
5). The best-estimate research diagnosis was generated at an evaluation research conference led by one of us (W.S.E.) approximately 4 weeks after admission. This allowed for the consideration and integration of clinical data from all sources, including family reports and medical records. Moreover, these data were no longer confounded by reporting because of acute decompensation or distress typically experienced at admission. The Personality Disorder Examination and best-estimate research diagnoses concurred in more than 85% of cases.
DISCUSSION
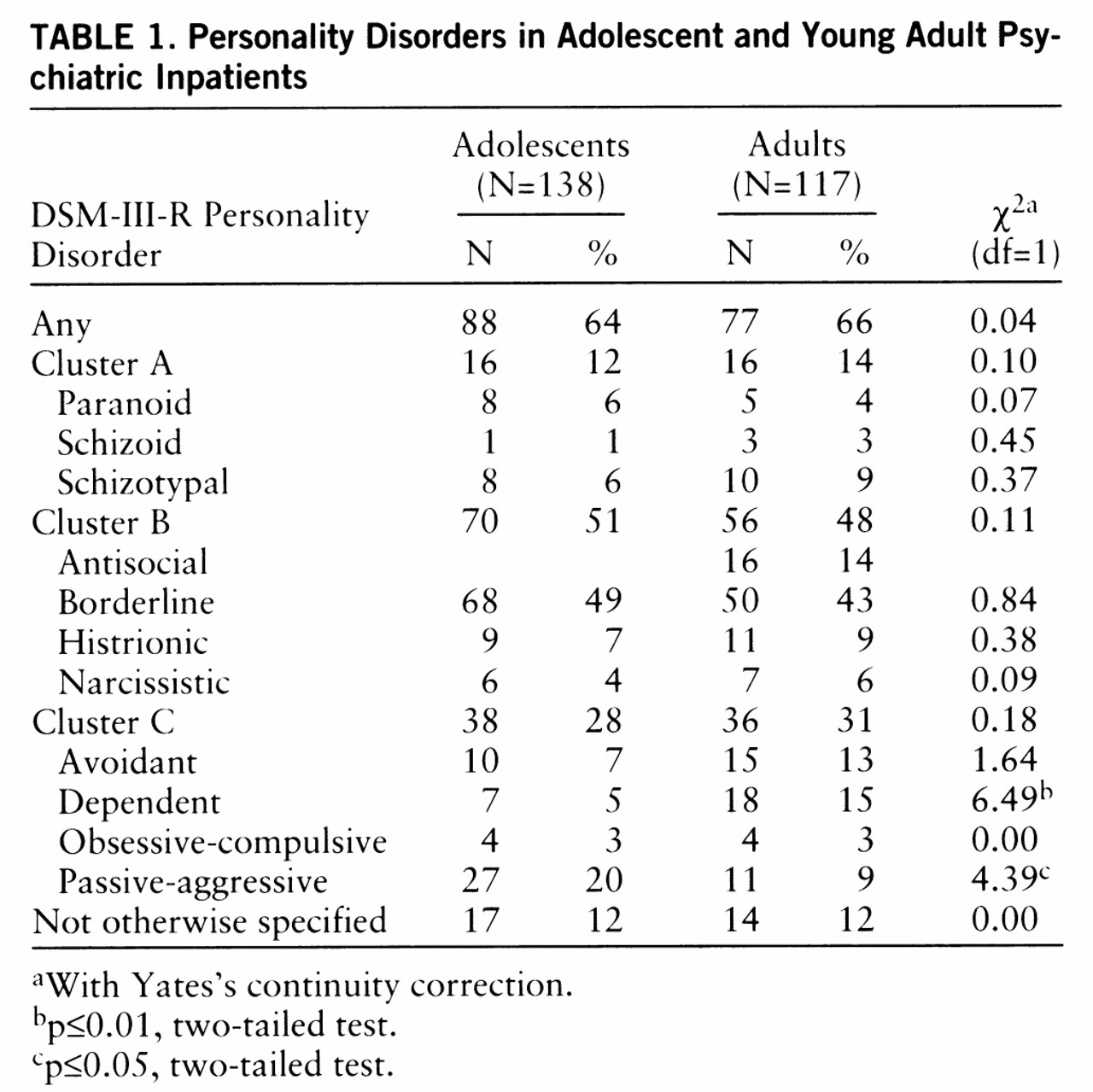
This study reliably assessed a consecutive series of adolescent and young adult inpatients by using structured diagnostic interviews for DSM-III-R personality disorders. All but two personality disorders had similar frequencies in the two age groups. Cluster A and B personality disorders were diagnosed at strikingly similar frequencies across age groups. Cluster C disorders proved to be the most sensitive to the developmental era but in different directions: passive-aggressive personality disorder had a lower frequency, whereas dependent personality disorder had a higher frequency, in the adult inpatient group.
The major advantage of this study resides in the use of a conservative, standardized, and reliable procedure for diagnosis. Both groups were evaluated by the same research evaluation team, which used the same diagnostic instruments and applied the same criteria sets and decision rules. The study employed Loranger et al.'s 3- and 5-year duration specification criteria (
4) for diagnosing personality disorders in adolescents and adults, respectively. This criterion, while more stringent than either DSM-III-R or DSM-IV specifications, suggests that the findings regarding personality dysfunction may reflect a relatively stable phenomenon rather than a situational response to axis I pathology. Adolescents may have a poor sense of time, thus making the duration criterion potentially ambiguous. However, the use of the stringent Personality Disorder Examination criteria was complemented by the best-estimate method, in accordance with the Longitudinal Expert All Data standard (
5), at a consensus research meeting 4 weeks after admission, thus allowing integration of clinical data.
A possible disadvantage is that the comparison groups were concurrent and independent rather than the same subjects followed into adulthood. Perhaps a more ideal study would begin with patients in adolescence and follow them over time. Of course, that study might be confounded by the influence of changing sociocultural factors, nosological schemes, and diagnostic practices. Further, our study group consisted of acutely ill adolescents and young adults requiring psychiatric hospitalization. Thus, our findings may not be generalizable to outpatient or community populations (
2) in which base rates of disorders are likely to differ. With these strengths and weaknesses in mind, we offer the following comments and recommendations for future investigation.
DSM-defined cluster A and B personality disorders appear to occur at similar frequencies in adolescent and young adult psychiatric inpatients. Cluster A disorders, insofar as they are part of the schizophrenia spectrum, are generally thought to represent the most biologically “wired-in” of the personality disorders. As such, it might be expected to find them in limited but consistent numbers despite differences in sample age or severity or both.
We found that passive-aggressive personality disorder was diagnosed with lower frequency and dependent personality disorder with higher frequency in the young adult than in the adolescent inpatient group. Some of this may be artifactual owing to the diagnostic criteria for the disorders. DSM-III-R criterion 2 for dependent personality disorder, for example, reads “Allows others to make most of his or her important decisions, e.g., where to live” Raters may not regard this as abnormal in adolescents, as opposed to young adults. The observed differences between the two age cohorts, therefore, might reflect differential interpretation of the pathology of behavior depending on developmental period. If so, the personality disorder criteria may need reformulation to be more sensitive and specific to developmental age. The criteria for passive-aggressive personality disorder are similar to those for the oppositional defiant disorder diagnosis of adolescence. Indeed, in DSM-IV, passive-aggressive personality disorder (which is included in appendix B as a research category) is considered only in adults. The presence of oppositional defiant disorder in adolescents tends to result in treatment seeking by their parents. The decrease in passive-aggressive personality disorder in adults may reflect less treatment seeking by these patients.
To summarize, our findings provide clues for understanding the longitudinal vicissitudes of personality dysfunction. Cluster A and B personality disorders were diagnosed at similar frequencies in adolescent and young adult inpatients. This isomorphism of relative prevalence might suggest that what we see in adolescents are valid forms of most of the adult personality disorders that do not go through some intermediate form before adulthood. Variations in passive-aggressive personality disorder and oppositional defiant disorder might reflect developmental flux in symptoms or differential interpretation of the behavioral patterns in different age groups. Both replication of our findings through use of similar methodologies and extension through use of complementary longitudinal designs are needed with DSM-IV-defined disorders.