ECT is a safe and effective treatment for patients with all subtypes of major depression (
1). A substantial body of research indicates that ECT is at least as effective as antidepressant medications for the treatment of major depression (
2); nonetheless, ECT is only rarely used as a first-line treatment (
3). The use of ECT in clinical practice has been limited by public concern regarding its safety (
4), regulations governing its use (
5,
6), and the perception that it is not a cost-effective alternative.
It is often assumed that ECT increases the length and costs of inpatient care (
7–
9). This assumption is based on studies that compare the length of stay of patients who have and have not received ECT. Depressed inpatients treated with ECT have significantly longer stays (mean=36.7 days) than patients treated with antidepressants (mean=19.5 days) (
7). Conversely, patients with long stays are more likely than patients with shorter stays to receive ECT (
8). Even inpatients who are treated with ECT promptly after hospital admission have longer stays than patients initially treated with antidepressant medications (
9). In the past decade, the only report to conclude that ECT shortens rather than lengthens hospital stays was from an inpatient unit with an exceptionally long mean length of stay (54.6 days) for depressed patients treated without ECT (
10).
An important limitation of previous studies is that they were conducted at urban, tertiary care teaching hospitals, and so their findings may not generalize to broader practice patterns. Furthermore, there has not been a consistent effort to control or adjust for pretreatment differences in the demographic and diagnostic characteristics of the patients who receive ECT. It is possible that underlying differences in the characteristics of patients selected for ECT help contribute to the observed correlation between ECT and longer inpatient stays.
ECT is often reserved for patients who have had an incomplete or partial response to antidepressant medications (
3). In evaluating the effect of ECT on the costs and length of hospitalization, it is important to distinguish this application of ECT from its use as an initial treatment. In this context, it remains unknown whether prompt initiation of ECT is associated with increased or decreased costs of the inpatient treatment of major depression. Given the generally comparable efficacy of ECT and antidepressant medications for major depression, the issue of cost-effectiveness assumes increased relevance. These issues are especially important in the light of present-day financial realities and the increasing trend toward prospective payment and capitation.
In this report, we analyze data from a large, nationally representative sample survey of general hospital inpatients to study the use of ECT for recurrent major depression. Before conducting the analyses, we hypothesized that patients selected for ECT would be older, have high rates of psychiatric and general medical comorbidity, and tend to receive inpatient care within large, urban medical centers. We further hypothesized that adjusting for these and related patient and hospital characteristics would account for much of the greater length of stay and greater inpatient costs associated with ECT.
METHOD
Patient data were drawn from the 1993 nationwide inpatient sample of the Healthcare Cost and Utilization Project (
11), which is sponsored by the Agency for Health Care Policy and Research. It consists of 6.5 million computerized case records from a geographically dispersed sample of 913 community hospitals in 17 states. It approximates a 20% sample of U.S. community hospitals. No state mental hospitals are included in the sample.
Some data on hospital variables in this report are derived from the 1994 American Hospital Association (AHA) Annual Survey of Hospitals (
12). The AHA survey includes detailed information on the services and operation of hospitals in the United States and associated territories that can be linked to the specific hospitals sampled in the Healthcare Cost and Utilization Project.
Sample selection was based on a stratified probability sample of short-stay nonfederal hospitals. To help ensure that the surveyed hospitals were representative, sampling strata were defined for five hospital characteristics: geographic region, ownership (nonfederal government, private nonprofit, or private for-profit), location (urban or rural), teaching status, and size (number of beds). A systematic random sample was drawn from each stratum. This selection occurred after we sorted hospitals by state within each stratum and by the first three digits of the hospital's zip code within each state and then by a random number within each three-digit zip code. Sampling probabilities were proportional to the number of U.S. community hospitals in each stratum. The Agency for Health Care Policy and Research constructed weights based on the reciprocal probability of sampling to approximate national estimates. All percentages in this report are weighted to adjust for the sampling probability.
Patient variables selected from the Healthcare Cost and Utilization Project discharge abstracts included length of inpatient stay, age, sex, race/ethnicity, primary payer, principal discharge diagnosis, discharge status, secondary diagnoses (up to 14), principal procedure, secondary procedures (up to 14), median income in the patient's residential zip code area, and total inpatient charges. Hospital variables drawn from the AHA survey included size, ownership, location, teaching status, number of psychiatric beds, and geographic region.
Data were collected from seven of the 10 AHA geographic regions of the United States and associated territories (
11). In some analyses, mountain and Pacific states were collapsed into “western states” New England, middle Atlantic, and south Atlantic states were collapsed into “eastern states” and east and west north central states were collapsed into “midwestern states.”
We restricted the main analysis to data on adults 18 years of age and older who had a principal discharge diagnosis of major depression, recurrent (ICD diagnosis 296.3), had a stay of more than 1 day, and were admitted to a general medical and surgical hospital with at least one psychiatric bed. Preliminary analysis revealed that ECT was far more commonly used in the treatment of recurrent depression than of single-episode major depression. In addition, ECT was very rarely used (0.17% of cases) for patients under 18 years of age who had recurrent major depression. Very brief stays (1 day or less) were excluded as administrative or “paper admissions.” Because of important differences in the presentation and treatment of depression in patients assigned to psychiatric beds and those assigned to general medical beds (
13), we excluded from the analysis patients who were admitted to hospitals without dedicated psychiatric beds. The vast majority (98.5%) of adult general hospital inpatients with a principal diagnosis of recurrent major depression who received ECT were treated in hospitals with at least one psychiatric bed. We have no means of determining the proportion of selected cases in which the patients were treated in dedicated psychiatric beds within these facilities.
Our first goal was to provide a descriptive overview of the use of ECT (ICD-9 procedure 94.27) for the treatment of depressive disorders, focusing on major depression, recurrent. We determined rates of ECT use stratified by patients' sociodemographic and diagnostic characteristics and hospitals' characteristics. A logistic regression was conducted to estimate associations of these variables with ECT.
Our second goal was to examine the effect of prompt use of ECT on the length and cost of inpatient care for recurrent depression. We evaluated the effect of ECT on these variables stratified by the date of the first ECT (during the first 1–5 hospital days versus more than 5 days after admission). General linear multiple regression analysis was used to estimate the association of prompt ECT administration with length of stay and total hospital charges, with control for sociodemographic, diagnostic, and hospital organizational variables.
Information on the timing of the first ECT session was only available when ECT was listed as the principal procedure. ECT was the principal procedure in 77.6% (N=1,754) of the cases of adult recurrent major depression for which it was provided. The remaining 22.4% of cases (N=437) were removed from the multivariate analyses of cost and length of stay.
We used the SUDAAN software package (
14) to accommodate the Healthcare Cost and Utilization Project sampling design and weights. SUDAAN was used to calculate adjusted means and corresponding standard errors with the logistic and linear regressions and to calculate 99% confidence intervals for the rate estimates.
RESULTS
In 1993 an estimated 249,600 patients were discharged from general hospitals with a principal diagnosis of a depressive disorder. These diagnoses were unevenly distributed between major depression, recurrent (47.7%), major depression, single episode (39.6%), depression not otherwise specified (6.4%), and dysthymia (6.3%). Major depression, recurrent, with psychotic features was the principal diagnosis in 10.0% of the depressive disorder cases, and major depression, single episode, with psychotic features was the principal diagnosis in 5.9% of the cases.
The rate of ECT use per 100 patients was higher for inpatients with a principal diagnosis of major depression, recurrent (9.4%), than for those with major depression, single episode (3.2%), dysthymia (0.5%), and depression not otherwise specified (0.8%). Patients with major depression, recurrent, with psychotic features and those with major depression, single episode, with psychotic features had relatively high rates of ECT (11.8% and 5.5%, respectively).
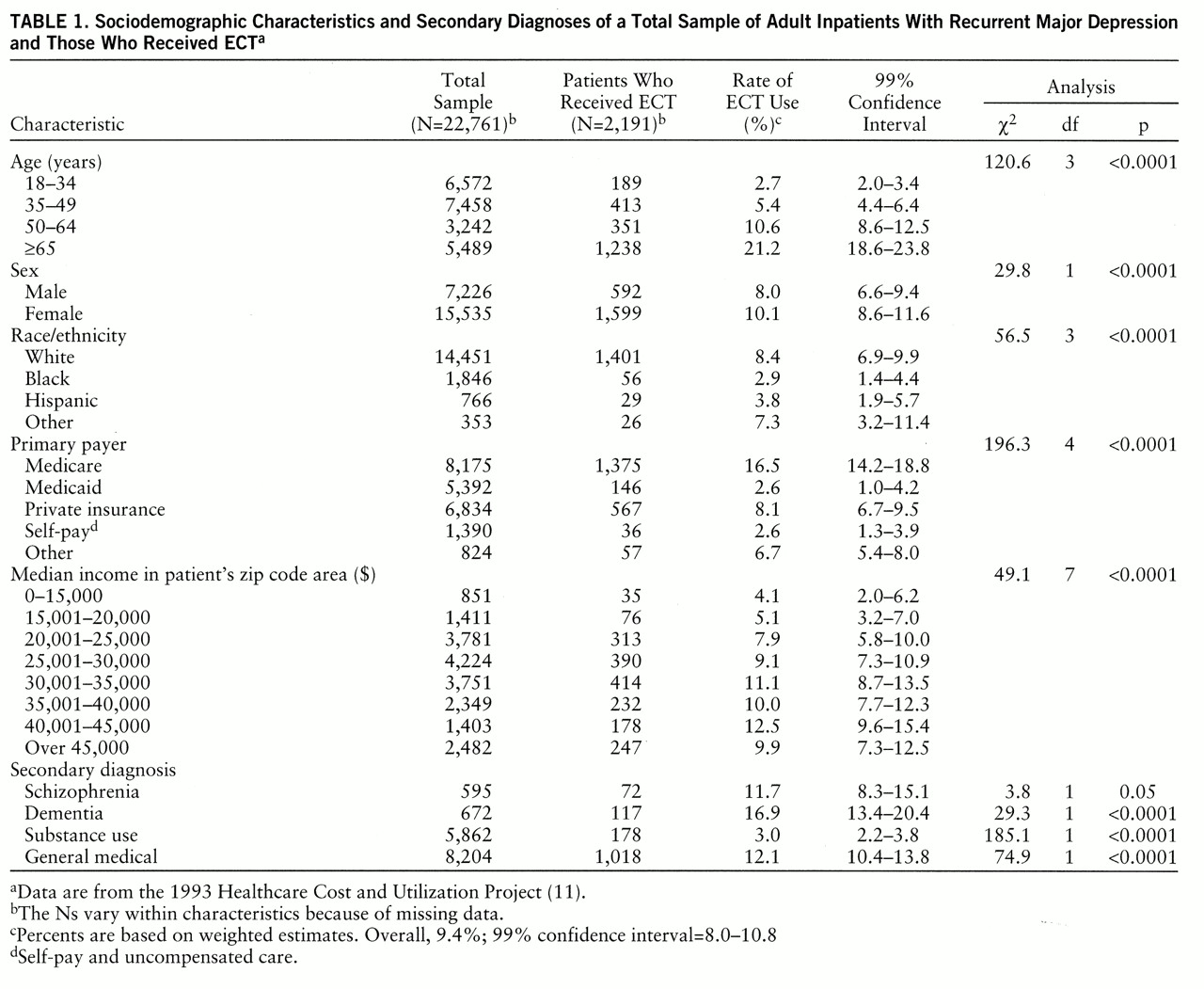
Among adults with a principal diagnosis of recurrent major depression, ECT use varied widely across demographic strata (
table 1). Comparatively high rates of ECT use were evident for older patients (especially those aged 65 years and older), whites, Medicare beneficiaries, and patients living in more affluent residential areas. By contrast, lower rates of ECT were observed for younger adults, blacks, Hispanics, Medicaid beneficiaries, self-paying patients, and those who lived in the poorest residential regions. Depressed inpatients with a secondary diagnosis of schizophrenia, a general medical disorder, or dementia were considerably more likely to receive ECT than those with a secondary diagnosis of a substance use disorder.
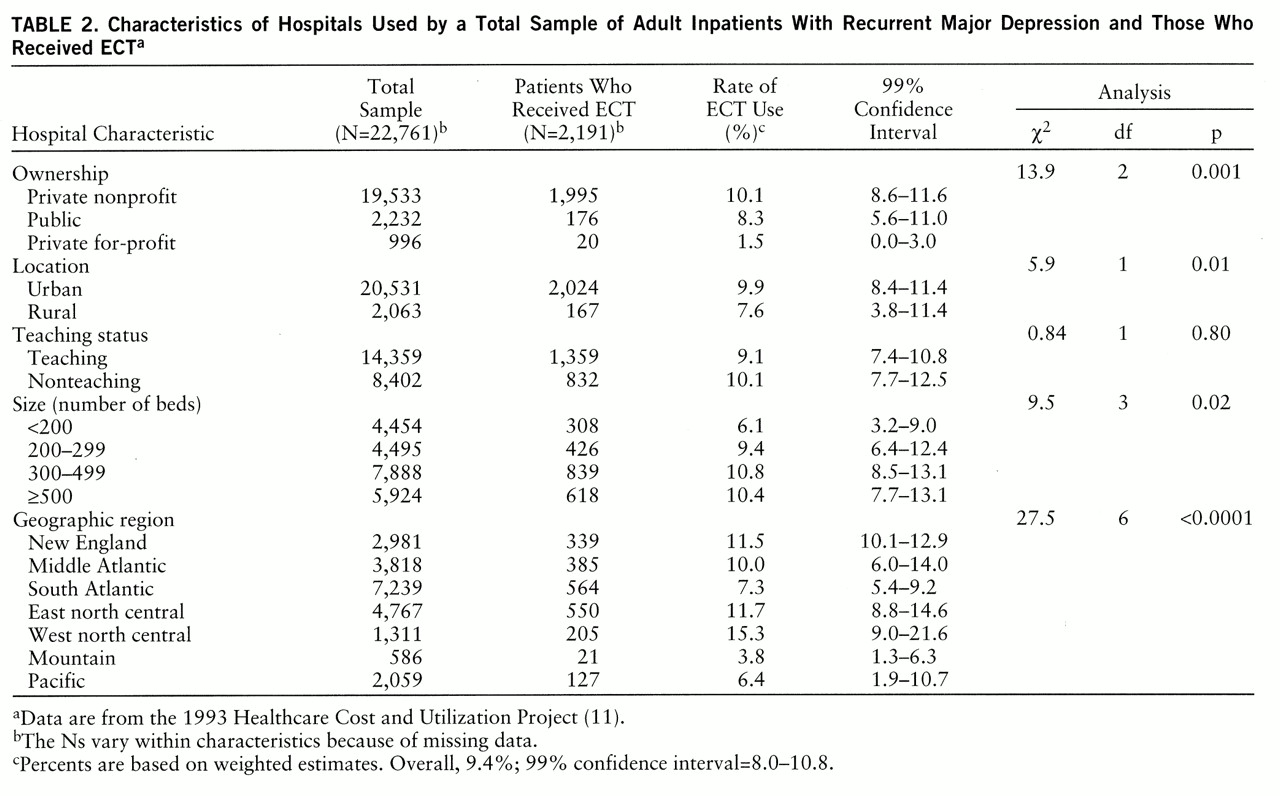
Use of ECT varied widely by geographic region. Depressed patients treated in the west north central states (Minnesota, Iowa, Missouri, North Dakota, South Dakota, Nebraska, Kansas) were approximately four times as likely as their counterparts in the mountain states (Montana, Idaho, Wyoming, Colorado, New Mexico, Arizona, Utah, Nevada) to receive ECT (
table 2). Depressed patients in private nonprofit and public general hospitals were significantly more likely to receive ECT than their counterparts in private for-profit general hospitals.
Data on discharge status were available for 2,176 patients with recurrent major depression who received ECT. Most (83.5%) were routinely discharged. Much smaller percentages were discharged to a skilled nursing facility (4.2%), home health care (3.8%), another short-term hospital (2.2%), an intensive care facility (1.9%), or some other health care facility (3.4%). Only 1.0% of the recurrently depressed patients who received ECT were discharged against medical advice.
None of the depressed patients who received ECT died during the hospitalization. In contrast, 30 (0.14%) of the depressed patients who did not receive ECT died in the hospital (χ2=41.6, df=1, p<0.0001).
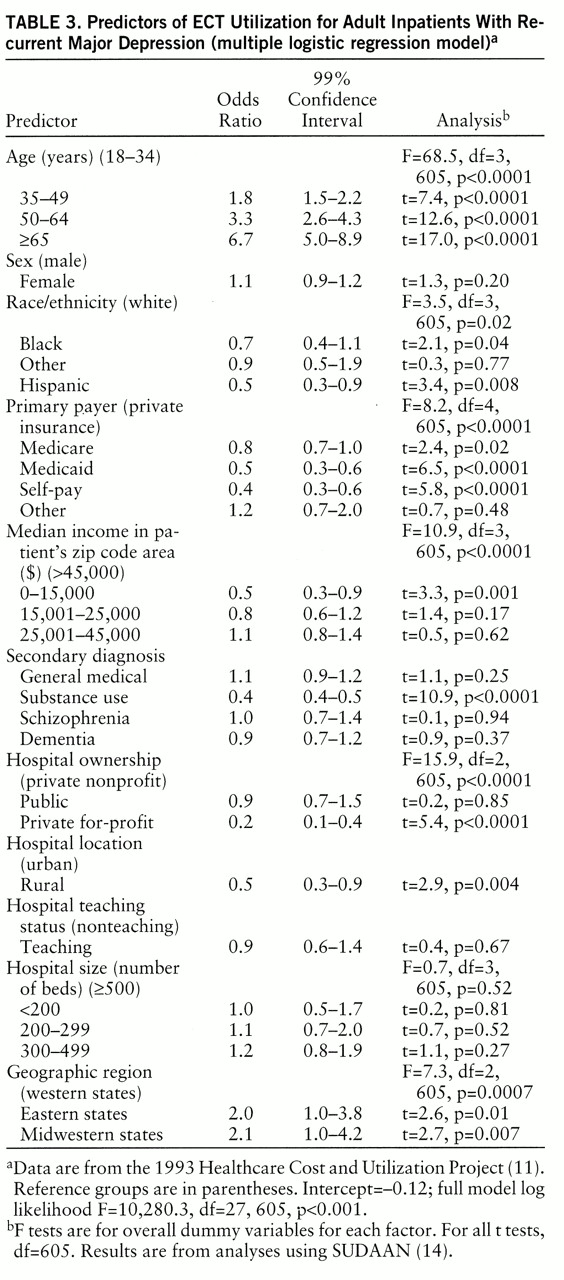
We used logistic regression to estimate associations of the demographic, payment, diagnostic, and hospital organizational variables with use of ECT for recurrent major depression. Age emerged as the most powerful predictor of the use of ECT, followed by geographic region (
table 3). In this model, patients aged 65 years and older had an estimated 6.7 times greater likelihood of receiving ECT than younger adults (18–34 years). Patients in eastern states and midwestern states were approximately twice as likely to receive ECT as their counterparts in western states.
Hispanic ethnicity, Medicaid payment, self-payment, low median residential area income, and a secondary substance use disorder diagnosis each independently and significantly decreased the likelihood of receiving ECT. Compared with whites, blacks tended to be less likely to receive ECT. The likelihood of receiving ECT was significantly reduced when treatment was in a rural hospital as compared with an urban hospital and within a private for-profit hospital as compared with a private nonprofit hospital (
table 3).
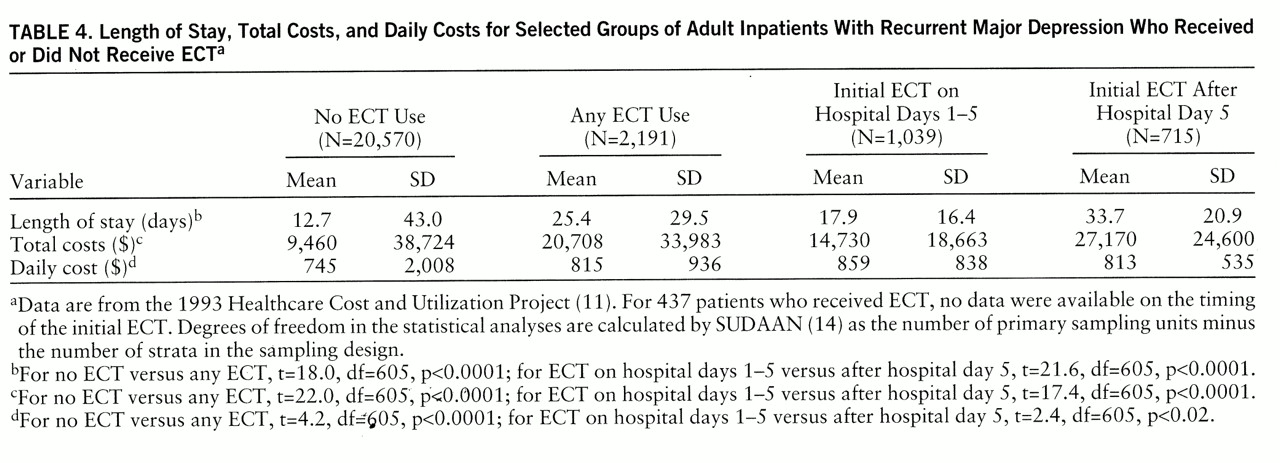
In univariate analyses, patients with recurrent depression who received ECT had significantly longer hospital stays, higher inpatient treatment costs, and higher daily treatment costs than patients who did not receive ECT (
table 4). Most (59.2%) of the patients who were treated with ECT as the principal procedure (N=1,754) received their initial ECT during the first 5 hospital days. The length of stay and total charges of patients who received ECT during the first 5 hospital days were significantly less than those of patients who received their initial ECT later in the hospitalization. However, the mean total inpatient cost for depressed patients who received ECT during the first 5 hospital days was more than $5,000 greater than the cost for depressed patients who did not receive ECT.
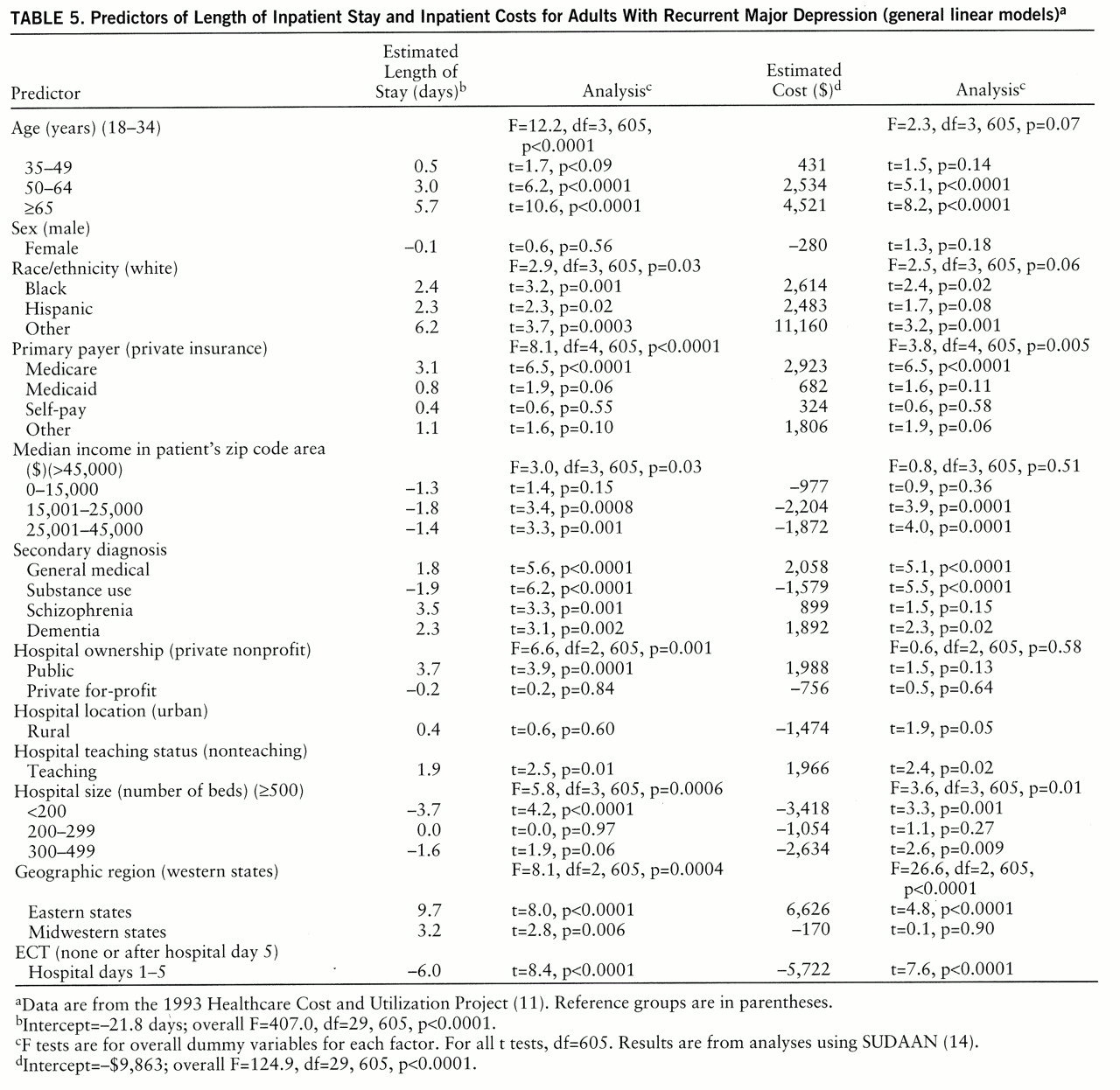
After controlling for the effects of the demographic, diagnostic, and hospital administrative variables, we found that prompt provision of ECT was associated with significantly shorter and less expensive inpatient stays (
table 5). In these multiple linear regression models, administration of ECT during the first 5 hospital days was associated with a 6.0-day reduction in length of stay and a decrease of $5,722 in hospital charges. Similar analyses of the subgroup of patients with recurrent major depression with psychotic features revealed an even stronger effect of prompt ECT administration on length of stay (9.0-day reduction) and hospital charges ($8,619 reduction).
Other factors associated with lower hospital charges included smaller hospital size, lower residential area median income, and a secondary diagnosis of a substance use disorder (
table 5). Factors significantly associated with greater hospital charges included older patient age, nonwhite race, Medicare insurance, and a secondary diagnosis of a general medical disorder or dementia. Higher inpatient costs were also associated with treatment in a teaching hospital and treatment in eastern rather than western states (
table 5).
DISCUSSION
In accord with several earlier studies, we found that depressed inpatients who receive ECT tend to have longer and more expensive hospital stays than similarly diagnosed patients treated without ECT (
7–
9). Even when ECT is initiated promptly during the hospitalization, it continues to be associated with longer and more costly inpatient treatment. However, depressed patients who receive ECT differ in several important respects from those who do not. Patients who receive ECT tend to be older (
15,
16) and are more likely to have secondary diagnoses of schizophrenia, dementia, and general medical (nonpsychiatric) disorders. They also tend to be treated in large urban hospitals that are operated on a private nonprofit basis and are located in eastern or midwestern states. When these and other differences are taken into account, prompt initiation of ECT is associated with shorter and less costly inpatient treatment as compared with no ECT or delayed ECT (
table 5). In other words, the long stays common among patients who receive ECT may be a consequence of underlying pretreatment patient and hospital characteristics rather than the ECT per se. Particularly impressive savings are associated with prompt use of ECT for patients with recurrent depression with psychotic features.
Aside from disposition of patients at hospital discharge, this study provides no information on clinical outcomes. For this reason, we are unable to assess the cost-effectiveness of ECT in this sample. However, we have no reason to believe that the clinical criteria for hospital discharge are different for depressed patients who receive ECT than for depressed patients who receive other treatments. We also note that a vast majority of the patients in our sample who were treated with ECT for recurrent depression were routinely discharged, and none of the patients who received ECT died during the hospitalization.
The finding of lower hospital charges associated with prompt use of ECT suggests that hospital costs would have been higher if ECT were not available for the patients who received it. However, we have no means of determining whether extending ECT to other patient groups or hospital settings would result in similar cost savings. It is possible that practicing physicians consider cost issues when selecting patients for ECT.
In line with earlier research (
15,
16), we observed that blacks tended to be less likely than whites to receive ECT. Beyond this racial disparity, Hispanic ethnicity, residence in a poorer area, Medicaid payment, and a lack of health insurance were each associated with a decreased probability of receiving ECT.
The basis of these disparities remains obscure. Low rates of ECT utilization among socioeconomically disadvantaged groups might reflect attitudinal or cultural barriers, knowledge deficits, or racial or economic biases in clinical selection and referral processes. Previous research indicates that ECT is rarely available in state and county mental hospitals (
15,
16). A dearth of funding to support personnel training may contribute to the scarcity of ECT in these facilities and in the general hospitals in the current study that serve poorer patient populations. There are no empirical data that provide a clinical rationale for the selective use of ECT in more affluent, socioeconomically advantaged patient groups. It is disconcerting that socioeconomically disadvantaged depressed patients do not have equal access to ECT. Detailed epidemiologic surveys of treatment seeking for major depression are needed for a better understanding of how clinical, attitudinal, cultural, financial, and service-related factors shape patient selection for ECT.
In keeping with previous research (
15,
17), we found a strong correlation between patients' age and the use of ECT. In years past, it was assumed that the selective use of ECT in older patients was related to the greater sensitivity of older patients to the side effects of tricyclic antidepressants. With the availability of newer antidepressants with fewer side effects and fewer drug-drug interactions, it might be expected that the rates of ECT would vary less across the age spectrum. However, a strong age effect persists. As with the socioeconomic disparities, it is not clear whether the selective use of ECT in the elderly represents differences in patients' attitudes, knowledge, and acceptance or entrenched practice patterns. There are data, however, which suggest that older depressed adults may preferentially respond to ECT (
18).
ECT was relatively rarely provided to depressed patients with a secondary diagnosis of a substance use disorder. Even after control for age and other factors, patients with a secondary substance use disorder were only about half as likely as those without such a disorder to receive ECT. Active substance use may complicate the clinical assessment and treatment of depressive symptoms. In many of these patients, depressive symptoms may resolve independent of specific antidepressant treatment (
19). Clinicians who perceive that affective symptoms are secondary to substance use may focus on maintaining abstinence and adopt a “watchful waiting” approach to the depressive symptoms.
We also found evidence of considerable geographic variation in ECT utilization, with higher use in eastern and midwestern states than in western states. Southern states, which have historically had low rates of ECT (
20), were not included in the survey. Differences in state regulation of the use of ECT are thought to help account for geographic variations in its use (
5,
17,
21). California, for example, regulates the use of ECT more stringently than several eastern and midwestern states (
5). Regional variation in psychiatric education concerning the clinical role of ECT (
22,
23) may be another source of geographic variation in the use of ECT. In many areas, ECT remains unavailable.
This study was constrained by several limitations in the survey data. Perhaps most important, the survey did not provide information on the clinical effectiveness of ECT. Beyond diagnosis, information was also not available concerning severity of illness and resistance to treatment. In addition, no data were provided on the specialty of the treating physician or on the quality of ECT administration (e.g., electrical stimulus intensity, electrode placement, number of ECTs) during the hospitalization. Furthermore, the analysis was limited to nonfederal general hospitals and so did not include information on the large number of patients who receive ECT in private psychiatric hospitals, state and county mental hospitals, and federal facilities.
In recent years, managed mental health care has spread at a breathtaking pace. The promise of cost savings has fueled the development of a complex array of cost-containment policies that effectively control patients' access to specialized mental health services. In this environment, procedures such as ECT that historically have been associated with long and more costly inpatient treatment are particularly vulnerable to rationing through utilization management.
We provide evidence suggesting that inpatient ECT for recurrent major depression is used in a highly selective manner. When ECT is initiated during the first few days of hospitalization, its added daily costs are more than offset by reductions in the length of the hospital stay. Before blunt administrative restrictions are placed on the use of ECT, it is critically important that careful analyses be conducted of the cost-effectiveness of this powerful treatment for depressive disorders.