The impact of lithium prophylaxis on the course of bipolar disorder has become a remarkably controversial issue. On the one hand, all but one of the double-blind trials conducted with bipolar I patients have found a significantly lower recurrence rate in patients treated with lithium than in those receiving placebo (
1–
8). On the other hand, studies carried out under ordinary clinical conditions have reported a rise in the admission rate for mania between the 1970s and the 1980s, despite the increased use of lithium (
9), and have found no significant difference on outcome measures between lithium-treated and non-lithium-treated bipolar patients (
10–
12).
The evidence provided by these two series of studies is not unambiguous. Some of the double-blind studies were in fact discontinuation trials, in which the recurrence rate among patients receiving placebo was probably inflated by the fact that they had just discontinued lithium; some others were parallel-group prospective trials in which treating physicians knew which patients were taking lithium and were allowed to increase the dosage of the drug when prodromic manic symptoms appeared, which probably produced an underestimation of the recurrence rate in the lithium-treated group (
13). On the other hand, the epidemiological studies showing an increased admission rate for mania from the 1970s to the 1980s did not document that patients hospitalized during the observation period had actually received lithium before admission (
14), and some of the clinical studies reporting a comparable outcome for lithium-treated and non-lithium-treated bipolar patients actually included in the lithium group patients who had received the drug for only part of the observation period and who may well have relapsed after lithium discontinuation. Furthermore, several studies carried out in ordinary clinical conditions did not ensure regular monitoring of plasma lithium levels, in the absence of which lithium prophylaxis cannot be said to be properly implemented.
The discrepancy between the results of the above-mentioned two series of studies has led researchers to draw different conclusions. Some of them (e.g., reference 11) have emphasized that lithium prophylaxis is not as useful in clinical practice as double-blind trials had suggested and have advocated the use of alternative drugs or combination treatments; some others (e.g, reference 15) have argued that if lithium does not work well in ordinary clinical conditions, this means that these conditions are not good enough, and the solution is not to use lithium less but to use it better. However, proponents of both approaches (e.g., references 10 and 16) have underscored the usefulness of a closer look at the experience of lithium clinics, which represent an intermediate situation between the experimental—and in some respects artificial—setting of double-blind trials and a clinical routine in which lithium prophylaxis is often not properly implemented and, therefore, cannot be expected to be fully effective. As a matter of fact, in lithium clinics the inclusion and exclusion criteria for double-blind trials, which limit the representativeness of patient samples, are not adopted, but treatment surveillance is accurate, and an effort is made to optimize compliance by means of the therapeutic alliance.
Unfortunately, currently available studies based on the experience of lithium clinics do not contribute substantially to the debate we have described. In fact, most of them were retrospective, were focused on self-selected groups of patients (typically, those who completed a minimum number of years of treatment), and ignored dropouts. These drawbacks were avoided in the present prospective study, which provides information on all bipolar patients who started routine lithium prophylaxis at a lithium clinic through a period of more than 15 years. For as long as they received lithium, these patients were evaluated every second month with standardized instruments. Moreover, all of them were contacted for a follow-up interview 5 years after the start of prophylaxis, and for those who were available (approximately 90% of the total group), the current drug treatment was recorded and the clinical and psychosocial outcomes were evaluated.
METHOD
The study group included all patients meeting the Research Diagnostic Criteria (RDC) (
17) for bipolar I disorder who started routine lithium prophylaxis at the lithium clinic of the First Psychiatric Department of Naples University between Jan. 1, 1975, and Dec. 31, 1991. There were 402 of these patients (180 male and 222 female), ranging in age at intake from 20 to 65 years (mean=40.7 years, SD=9.5). On the occasion of the first visit, they received a clinical interview and, starting in 1978, the Schedule for Affective Disorders and Schizophrenia (SADS) (
18) and the Comprehensive Psychopathological Rating Scale (
19). All assessments were made by trained psychiatrists, whose agreement in the use of the RDC, the SADS, and the Comprehensive Psychopathological Rating Scale had been found to be satisfactory (
20). An ad hoc schedule was used to record, for each patient, the following demographic and historical data: age, sex, age at first psychiatric contact, number of prior affective episodes and hospitalizations, presence or absence of the rapid cycling pattern (defined as the occurrence of at least four affective episodes during the past year [21]), presence or absence of the pattern of course of illness marked by the sequence depression/mania/free intervals, presence or absence of delusions and/or hallucinations during the index episode (i.e., the episode during or after which lithium treatment was started), and presence or absence of a history of bipolar disorder in first-degree relatives, as explored with the Family History Research Diagnostic Criteria (
22). The affective morbidity and the hospitalizations during the 2 years preceding the index episode were reviewed month by month on the basis of the information provided by the patient, his or her relatives, and available clinical records.
Lithium was prescribed by the psychiatrist in charge of each patient, and its dosage was adjusted in order to obtain 12-hour plasma levels in the range of 0.5–1.0 mmol/liter. Other treatments were decided by the same psychiatrist on the basis of clinical judgment. At the beginning of lithium prophylaxis, 64 patients were being treated with antipsychotics, 185 with benzodiazepines, and 17 with antidepressants; none was being treated with other mood stabilizers.
Before starting lithium prophylaxis, all patients and, when possible, their key relatives received detailed information on bipolar disorder, the aims of lithium treatment, and its most frequent side effects. Each patient was informed that data concerning the outcome of his or her treatment would be used for research purposes but that he or she would not be personally identifiable in any report. After complete description of the study to the subjects, written informed consent was obtained.
For as long as they received lithium, the patients were seen with variable frequency, depending on clinical need, but were evaluated systematically every second month. These evaluations included a clinical interview, and, starting in 1978, the administration of the Comprehensive Psychopathological Rating Scale and the version of the SADS for measuring change (SADS-C). New RDC-diagnosed major depressive and manic episodes, new hospitalizations, the Comprehensive Psychopathological Rating Scale global score, lithium dosage and 12-hour plasma levels, other prescribed drugs and their dosage, and major intercurrent life events (i.e., death of a close family member, major financial or work difficulties, major physical illness, divorce or marital separation, and hospitalization of a close family member for serious illness) were carefully recorded. On the occasion of each visit, patients had the opportunity to discuss with their psychiatrists all their doubts and problems concerning treatment, its efficacy, and its side effects.
Five years after the start of lithium prophylaxis, all patients, whether or not they still attended the clinic, were contacted for a brief interview to collect information on current drug treatment, to explore the reasons for interruption of prophylaxis among those who were not taking lithium, and to administer the Strauss-Carpenter outcome scale (
23). This scale was applied by trained psychiatrists whose agreement in the use of the instrument had been found to be satisfactory (for the individual items, Cohen's kappa coefficient=0.73–0.99).
This procedure allowed us to answer the following questions: 1) How many bipolar patients who have started lithium prophylaxis at a lithium clinic are still taking lithium after 5 years? 2) Of those who are not taking lithium, how many interrupted prophylaxis on their own initiative and for what reasons? 3) Among those who are taking lithium, what patterns of outcome of the prophylactic treatment can be identified? 4) Are there any demographic, historical, or clinical correlates of these patterns? 5) Is there any significant difference, with respect to recent course of illness and psychosocial adjustment, between bipolar patients who are still taking lithium after 5 years and those who are not?
Comparisons between the patients who were taking lithium at follow-up and those who were not, and between the subgroups of patients who were taking lithium, were performed with the use of Student's t test, analysis of variance with Tukey's honestly significant difference test for post hoc comparisons, or the chi-square test, as appropriate.
A hierarchical logistic regression analysis was computed for the patients who were still taking lithium at follow-up. This analysis explored the impact of the above-mentioned demographic, historical, and clinical variables, as well as that of adherence to treatment (i.e., whether plasma lithium levels had been below 0.5 mmol/liter on more than 10% of checks), on the probability that there would be a recurrence of illness during the treatment period.
RESULTS
Dropout Rate and Reasons for Interruption of Prophylaxis
Of the 402 patients who had started lithium prophylaxis, 359 (89.3%) could be interviewed after 5 years. Of the rest, 10 were dead and 33 could not be traced or refused the interview. No significant difference, with respect to baseline demographic and historical characteristics listed in the previous section, was detected between the patients who could be interviewed and those who could not.
Two hundred forty-seven patients (61.4% of the initial study group and 68.8% of those who could be interviewed) were still taking lithium at follow-up. Of the above-mentioned baseline demographic and historical characteristics, the only one that distinguished the patients who were still taking lithium at follow-up from those who were not was the percentage of cases in which there were delusions and/or hallucinations during the index episode, which was higher in the latter group (χ2=2.84, df=1, p<0.01).
Of the 112 interviewed patients who were not taking lithium at follow-up, 95 (84.8%) had interrupted prophylaxis on their own initiative. The alleged main reason for interruption of medication was its perceived inefficacy in 35 cases, trouble related to side effects in 27, the conviction that the patient was cured and needed no more drugs in 17, the annoyance of taking medicines in 11, and loss of energy or productivity in five.
Of the patients not taking lithium, 26 (23.2%) were not taking any psychotropic drug on a regular basis (or were taking only benzodiazepines) at the time of the follow-up interview, whereas 19 (17.0%) were taking only one or more mood stabilizers other than lithium (carbamazepine, valproic acid, and/or dipropylacetamide), 28 (25.0%) were taking one or more mood stabilizers other than lithium plus antipsychotics and/or antidepressants, and 39 (34.8%) were taking only antipsychotics and/or antidepressants.
Patterns of Outcome of Prophylaxis and Their Correlates
Of the 247 patients who were still taking lithium at the time of the follow-up interview, 94 (38.1%) had had no RDC-diagnosed major depressive or manic episode during the treatment period (group A); 115 (46.6%) had had at least one RDC-diagnosed major depressive or manic episode, but with a reduction of at least 50% in the mean annual time spent in the hospital during the treatment period compared to the 2-year period preceding the index episode (group B); and 38 (15.4%) had had at least one RDC-diagnosed major depressive or manic episode without the above-mentioned reduction of at least 50% in the mean annual time spent in the hospital (group C). Within group A, 37 patients (15.0% of those taking lithium at follow-up) had shown a subsyndromal affective morbidity during the treatment period (defined as the presence at least two of the symptoms listed in the RDC for either major depression or mania, on the occasion of at least two evaluations). Within group B, 16 patients (6.5% of those taking lithium at the time of the follow-up interview) had had affective episodes only during the first year of prophylaxis.
Thus, considering the whole group of bipolar patients who had started lithium prophylaxis, 10.7% were not available at follow-up; 27.9% were not taking lithium at follow-up; 9.5% were taking lithium and had had at least one affective episode during the treatment period, without a reduction of at least 50% in the mean annual time spent in the hospital; 28.6% were taking lithium and had had at least one recurrence during the treatment period, with a reduction of at least 50% of the mean annual time spent in the hospital; and 23.4% were taking lithium and had had no affective episode during the treatment period (including a subgroup of 14.2% of the patients who had had no affective morbidity, even subsyndromal).
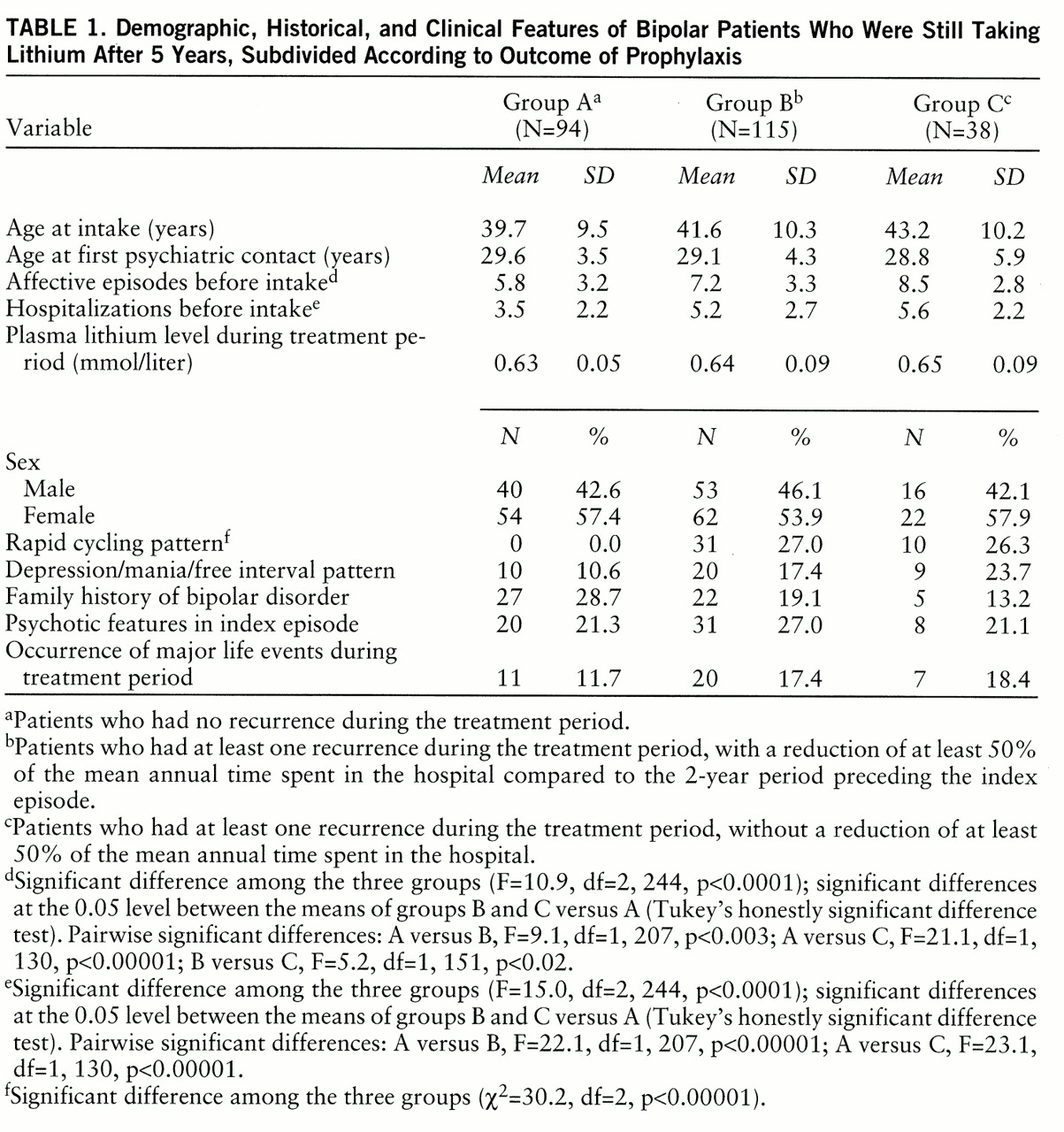
When groups A, B, and C of the patients still taking lithium at follow-up were compared with respect to demographic, historical, and clinical features (
table 1), significant differences were found in the mean number of prior affective episodes and hospitalizations and the frequency of the rapid cycling pattern. The percentage of patients who were taking other psychotropic drugs in addition to lithium at the follow-up interview was 17.0% for group A (N=16) (no patient was taking other mood stabilizers), 36.5% for group B (N=42) (14.8% were taking other mood stabilizers), and 86.8% for group C (N=33) (52.6% were taking other mood stabilizers). In the hierarchical logistic regression analysis, the variables that were found to have an impact on the patients' probability of having no recurrence were adherence to treatment (β value=0.54, df=1, p<0.01) and the number of pretreatment hospitalizations (β value=–0.14, df=1, p<0.04).
Among the patients who were still taking lithium at follow-up, 200 (81.0%) had had plasma lithium levels below 0.5 mmol/liter on no more than 10% of checks. Of these patients, 86 (43.0%) belonged to group A, 90 (45.0%) to group B, and 24 (12.0%) to group C. When the comparison between groups A, B, and C reported in
table 1 was repeated for these subgroups, the differences concerning the mean numbers of pretreatment affective episodes and hospitalizations and the frequency of the rapid cycling pattern remained significant (F=7.2, df=2,197, p<0.001; F=11.0, df=2,197, p<0.00001; and χ
2=24.8, df=2, p<0.00001, respectively).
Follow-Up Assessments
The patients who were not taking lithium at follow-up, compared with those who were, had significantly lower total scores on the Strauss-Carpenter outcome scale (i.e., worse outcomes) (mean score=11.6, SD=3.3, versus mean=12.6, SD=3.0; t=4.54, df=358, p<0.001) and significantly lower scores on the hospitalization item (t=3.81, df=358, p<0.001) and the employment item (t=3.76, df=358, p<0.001). The subgroup of patients who were not taking any psychotropic drugs (except benzodiazepines) did not differ significantly on any outcome measure from the group of patients taking lithium.
DISCUSSION
This is, to our knowledge, the first prospective study that has collected information on all bipolar I patients who started lithium prophylaxis at a lithium clinic through a period of more than 15 years. Unlike most previous reports of the experience of lithium clinics, this study did not focus on a self-selected group of patients (i.e., those who had completed a minimum number of years of treatment) and did not ignore dropouts.
The group of patients followed up in this study included patients with other concomitant psychiatric disorders, alcohol or drug abuse, and rapid cycling, as well as patients with concomitant physical diseases (except those in which lithium treatment is contraindicated) and those who were receiving treatment with other psychotropic drugs. All patients and, when possible, their key relatives received adequate information on bipolar disorder, the aims of lithium prophylaxis, and the possible side effects of treatment. Throughout the treatment period, an effort was made to optimize compliance by seeing patients frequently and giving them the opportunity to discuss regularly with their psychiatrists all treatment-related doubts and problems. Plasma lithium levels were estimated every second month, and lithium dosage was adjusted accordingly.
In this series, whose representativeness was not biased by the inclusion and exclusion criteria commonly adopted in double-blind trials, and in which treatment surveillance was in keeping with internationally accepted guidelines, one-fourth of the patients interrupted lithium prophylaxis on their own initiative before the term of 5 years. This demonstrates that “information, support and supervision” (
15) are not sufficient to counteract the tendency of bipolar patients receiving long-term lithium treatment to drop out. Adjunctive psychoeducational and psychotherapeutic interventions may improve patients' acceptance of lithium prophylaxis, but their ability to reduce the impact of factors such as perceived inefficacy of treatment or trouble related to side effects (which accounted for about two-thirds of the interruptions in our study group) remains to be documented. The interruption of lithium treatment is likely to contribute substantially to the persistently high admission rates for mania reported by epidemiological studies (
9), since it is followed by a high risk of early recurrence of mania (
24) and may cause the development of a secondary refractoriness to treatment with the drug (
25,
26).
When we concentrated our attention on patients who were still taking lithium at the time of the follow-up interview, we found that about 85% of them had had a reduction of at least 50% in mean annual time spent in the hospital during the treatment period compared to the 2-year period preceding the index episode, and that about 38% of them had had no recurrence during lithium prophylaxis. These percentages increased to 88% and 43%, respectively, when we considered only patients who had had plasma lithium levels below 0.5 mmol/liter on no more than 10% of checks. These findings apparently support the predominant clinical perception that lithium, if taken regularly for several years, has a substantial impact on the course of illness in most bipolar patients. However, the bias of self-selection should not be overlooked; the figures just cited refer to subgroups (61% and 50% of the enrolled patients, respectively) whose permanence on the prophylactic regimen may have been a consequence as well as a determinant of the favorable response, and who may be not representative of the initial study group. As a matter of fact, patients with psychotic features in the index episode, which have been reported to be associated with poor prognosis in bipolar disorder (
27), were overrepresented among those who stopped lithium before the 5-year term.
= The results of the follow-up assessments should be interpreted in the same light: the better outcome of the patients still taking lithium may have been a consequence of self-selection, whereas the lack of differences between the patients who were taking no psychotropic drugs except benzodiazepines and those who were taking lithium may simply mean that patients who stop lithium prophylaxis include a subgroup with a very benign course of illness who do not need long-term drug treatment.
= Our effort to replicate the previous reports of an association between a family history of bipolar disorder and a favorable outcome of lithium prophylaxis, and between the depression/mania/free interval pattern of course of illness and a poor outcome (see reference 28 for a review), was not successful. Although the expected trend was observed, the associations were not significant. On the other hand, we confirmed the previous findings (
29,
30) that a high frequency of pretreatment affective episodes and hospitalizations and the rapid cycling pattern are associated with a poor outcome of prophylaxis. These three variables, however, can hardly be regarded as true predictors of response to lithium; they actually predict a poor outcome of bipolar disorder independent of treatment (
21,
31) and may not be useful in the choice of medication. The claim that anticonvulsants are more effective than lithium in rapid cyclers has not been supported so far by comparative investigations, whereas a retrospective study by Okuma (
32), one of the earliest advocates of the use of carbamazepine in bipolar disorder, found that rapid cycling is a predictor of a poor response to that drug as well as to lithium.
= In conclusion, this study, the first carried out prospectively on all bipolar patients who started lithium prophylaxis at a lithium clinic over a period of more than 15 years, confirms that the impact of lithium prophylaxis on the course of bipolar disorder is severely limited by the very high dropout rate. For patients who keep on taking lithium for several years, a drastic reduction of the mean annual time spent in the hospital is almost the rule. However, bipolar patients who remain on a lithium regimen for several years represent a self-selected population in which some groups at high risk of poor outcome may be underrepresented.