Many patients with schizophrenia fail to show satisfactory improvement early in the course of antipsychotic treatment, and clinicians have traditionally responded by increasing the medication dose. Growing evidence—derived from studies of plasma level/response relationships, receptor occupancy, and responses to dose reduction—suggests that this tradition may be counterproductive and that attention to plasma levels may enhance clinical management.
Haloperidol has no active metabolites, with the possible exception of reduced haloperidol, and has been the antipsychotic most often used in plasma level/response studies. Many efforts to find clear relationships between plasma levels and response have failed, but falsely negative studies are far more likely to occur than falsely positive ones for a number of reasons. Protocols that titrate dose to clinical change produce data that are confounded by artifactual associations between high plasma levels and response. Among fixed-dose studies, the inclusion of subjects who are unlikely to improve at any plasma level obscures potential plasma level/response relationships. Moreover, the distribution of steady-state blood levels must fall generously on either side of a true therapeutic threshold in order to define it. If the distribution of plasma levels is insufficient, no relationship will emerge.
Despite these potential difficulties, at least nine studies have succeeded in identifying a plasma level threshold above which clinical improvement is no more, or is even less, likely to occur (
1–
10). The proposed upper thresholds covered a wide range, and some were defined by only a few subjects. Notably, however, seven of the proposed upper thresholds lie between 11 ng/ml and 18 ng/ml, inclusive, and the median value for all nine studies is 17 ng/ml.
Positron emission tomography (PET) offers another approach to the question of therapeutic plasma level thresholds. Receptor occupancy appears to reach an asymptote of approximately 80% at haloperidol steady-state levels between 4 ng/ml and 10 ng/ml (
11,
12). Once this plateau has been reached, higher antipsychotic plasma levels are associated with higher extrapyramidal symptom scores (
13,
14). These findings fit well with those of McEvoy et al. (
15,
16), who found that neuroleptic thresholds, the plasma levels at which extrapyramidal signs first manifest, cluster between 3 and 5 ng/ml.
Evidence for upper therapeutic limits has prompted investigators to use dose manipulation studies to weigh the possible benefits of lower doses. In two of these, the lowering of doses among institutionalized (
17) or chronically treatment-refractory patients (
18) reduced side effects but did not worsen positive symptoms.
Volavka et al. (
8) tested the effects of lowering doses in a controlled fashion. Patients were assigned to doses that targeted either a low (2 ng/ml) or a moderate (10 ng/ml) steady-state plasma level. Half of those who had improved by less than 50% after 3 weeks were assigned to the alternate dose range. Dose increases were followed by increases in negative symptoms, while the converse occurred after doses were lowered. Neither manipulation had an appreciable effect on positive symptoms.
Such findings support the routine use of plasma level measures in clinical management, particularly for those patients who initially fail to improve. We report here a study that used the median upper therapeutic threshold of 18 ng/ml to directly assess the value of a specified therapeutic plasma level range in the clinical management of those schizophrenic patients whose initial improvement with haloperidol was inadequate.
METHOD
Subjects
Subjects were recruited from the adult psychiatric inpatient units of the University of Iowa Hospital within 1 week of admission. All subjects provided written informed consent after the procedures and risks involved had been fully explained to them. Inclusion criteria specified that all participants met DSM-III criteria for schizophrenia, were 17 years of age or older, and had an IQ of at least 70, a Brief Psychiatric Rating Scale (BPRS) score higher than 40, and no history of allergy to haloperidol. The patients had also been free of depot antipsychotics for at least 3 months. In all cases, the attending psychiatrist had determined that the patient should be treated with an antipsychotic and that no other psychotropic drug would be necessary beyond those needed to control extrapyramidal symptoms.
Procedures
Diagnoses were based on information from medical records and direct interviews. The patients were evaluated at baseline with the Scale for the Assessment of Negative Symptoms (SANS) (
19), the Scale for the Assessment of Positive Symptoms (SAPS) (
20), and the modified 23-item BPRS (items rated 1–7, with 7 being severe) (
21).
Initial doses for the majority of patients were derived from a kinetics determination. Patients took an oral loading dose of haloperidol, 20 mg, at 9:00 p.m. and provided blood samples 12 and 24 hours later. A formula (
22) was applied to the resulting data to calculate the doses needed to produce steady-state haloperidol levels in a “low” (8–18 ng/ml) or “high” (25–35 ng/ml) range. The upper limit of this range was chosen to correspond to the median of the proposed upper limits from studies available when the protocol was developed. Because there was very little evidence on which to base a lower limit, this was chosen arbitrarily. The boundaries for the higher range were likewise arbitrary. We wished to minimize overlap between the two groups but also wished to produce levels that would be common in clinical settings. A random numbers table was used to assign patients to one or the other of these ranges in a 1:1 ratio. Regardless of assignment, all patients received benztropine, 1 mg b.i.d., and propranolol, 20 mg t.i.d., to prevent extrapyramidal symptoms and akathisia.
Some patients entered the protocol on a Thursday or Friday, and a kinetic determination of dose would have delayed the initiation of treatment. In these cases, doses were assigned according to a formula that reflected both weight and smoking status (
23). In either case, dose assignments for weeks 1–3 were made within the first week and remained fixed for the remainder of the initial 3-week period.
A rater blind to plasma levels and dose assignments administered the BPRS and rated side effects at the end of each week with the Simpson-Angus Rating Scale (
24) and the Hillside Akathisia Scale (
25). SANS and SAPS scales were completed at the end of weeks 3 and 6. After 3 weeks, patients whose total BPRS score had improved 30% or more from baseline were kept at the same dose for an additional 3 weeks. The remaining patients were eligible for dose reassignment. Half of these patients were randomly assigned to continue at the same dose, and the other half were assigned a dose that was intended to achieve a steady-state haloperidol plasma level in the alternate range. Doses were then fixed for the remaining 3 weeks.
The protocol did not require continued inpatient status. The patient's physician determined the discharge date according to routine clinical criteria and, in all cases, discharge occurred before protocol completion. Blood samples and ratings were then obtained on an outpatient basis for the remainder of the protocol.
Haloperidol plasma concentrations were determined by high performance liquid chromatography with ultraviolet detection as described by Jatlow et al. (
26). The assay is linear between concentrations of 2 and 75 ng/ml and has a lower limit of sensitivity of 2 ng/ml. Within- and between-day coefficients of variation range from 5% to 8% for each at concentrations of 5, 10, 20, and 30 ng/ml.
Analyses
The two target plasma level ranges, less than 18 ng/ml and greater than 25 ng/ml, were designated “low” and “high,” respectively. Patients who, despite projections, had levels between these two ranges were placed in the “intermediate” group. Changes in BPRS scores for these three groups were compared at each of the first 3 weeks. Time to 30% improvement in BPRS scores for the groups were then compared by using life-table methods (
27).
Analyses also considered continuous relationships between plasma level and symptom changes over the first 3 weeks of fixed dosing. Scatter plots of weekly haloperidol plasma levels against percent changes in the full-scale BPRS scores and in the negative and positive symptom subscale scores were inspected for visually obvious relationships.
Patients whose BPRS scores failed to improve by at least 30% by the end of the third week and who then underwent a dose change were considered separately. These subjects were grouped by the resulting haloperidol steady-state levels, and symptom changes for these groups were compared over the final 3 weeks. The patients were also grouped simply by whether their doses were increased or decreased, and symptom changes for these two groups were likewise compared over the subsequent weeks. Since substantially fewer symptom changes occurred in the last 3 weeks than in the first 3 weeks, life-table comparisons employed 20% change as an endpoint. We used the Wilcoxon statistic for all life-table comparisons.
RESULTS
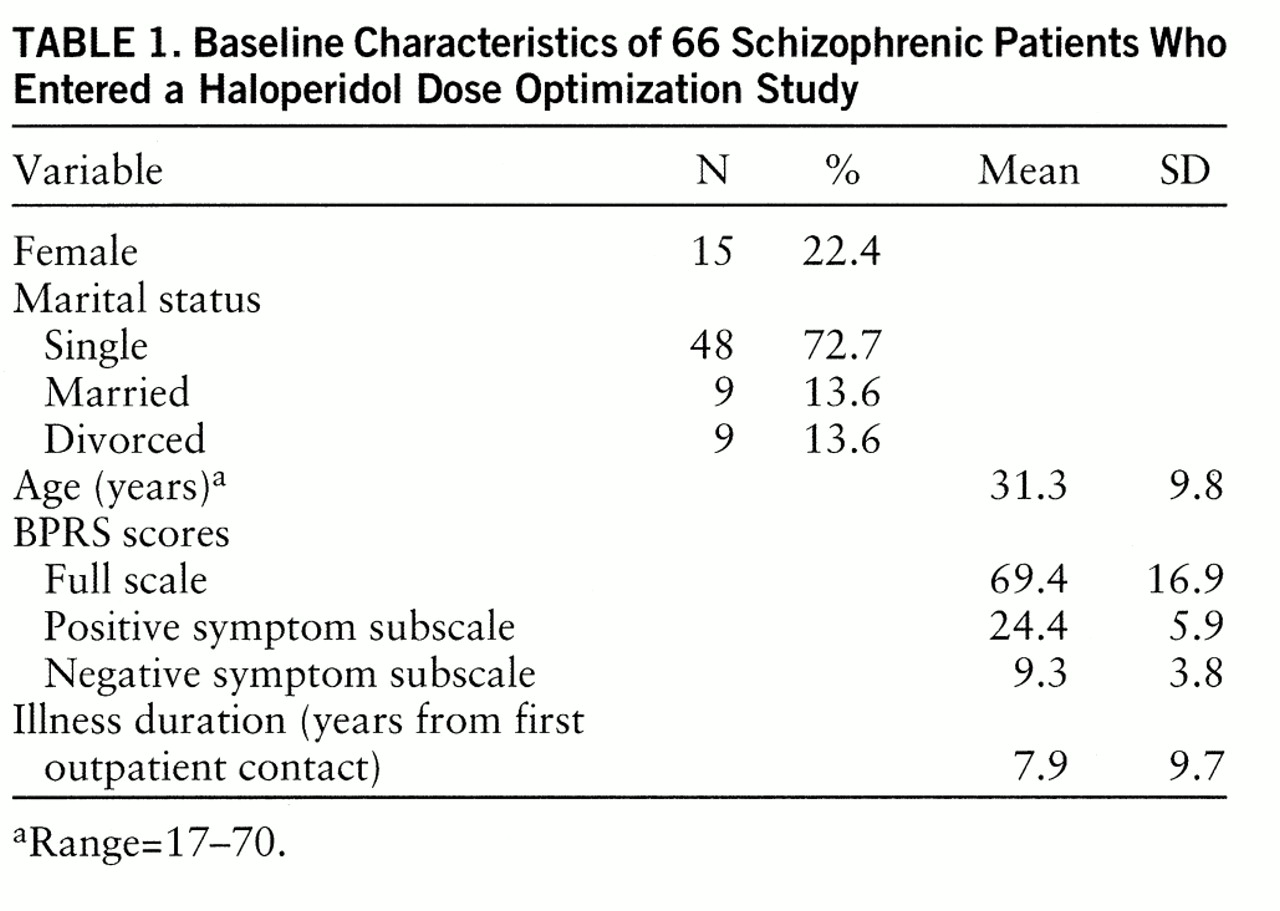
Sixty-six subjects entered the protocol, and their demographic and clinical characteristics at baseline are presented in
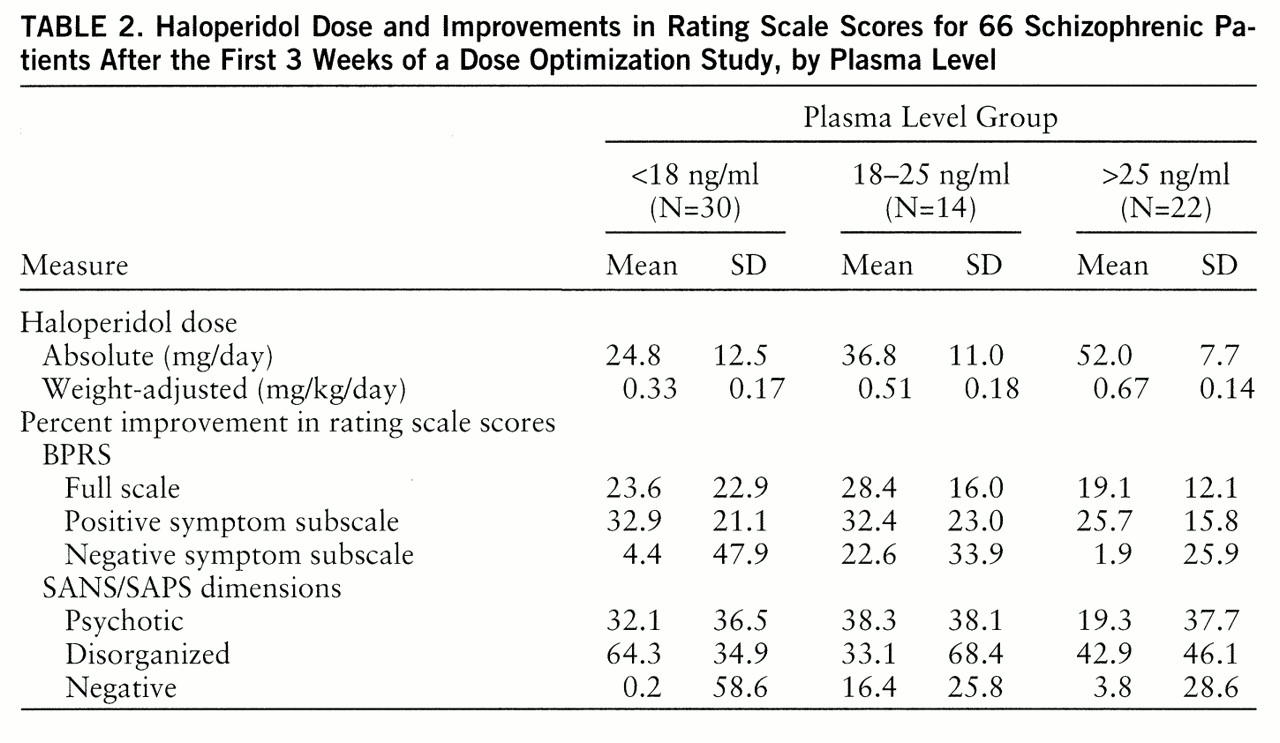
table 1. After 3 weeks, 30 patients had mean haloperidol plasma levels in the low (less than 18 ng/ml) range; 14 and 22 subjects had mean plasma levels in the intermediate (18–25 ng/ml) and high (greater than 25 ng/ml) ranges, respectively.
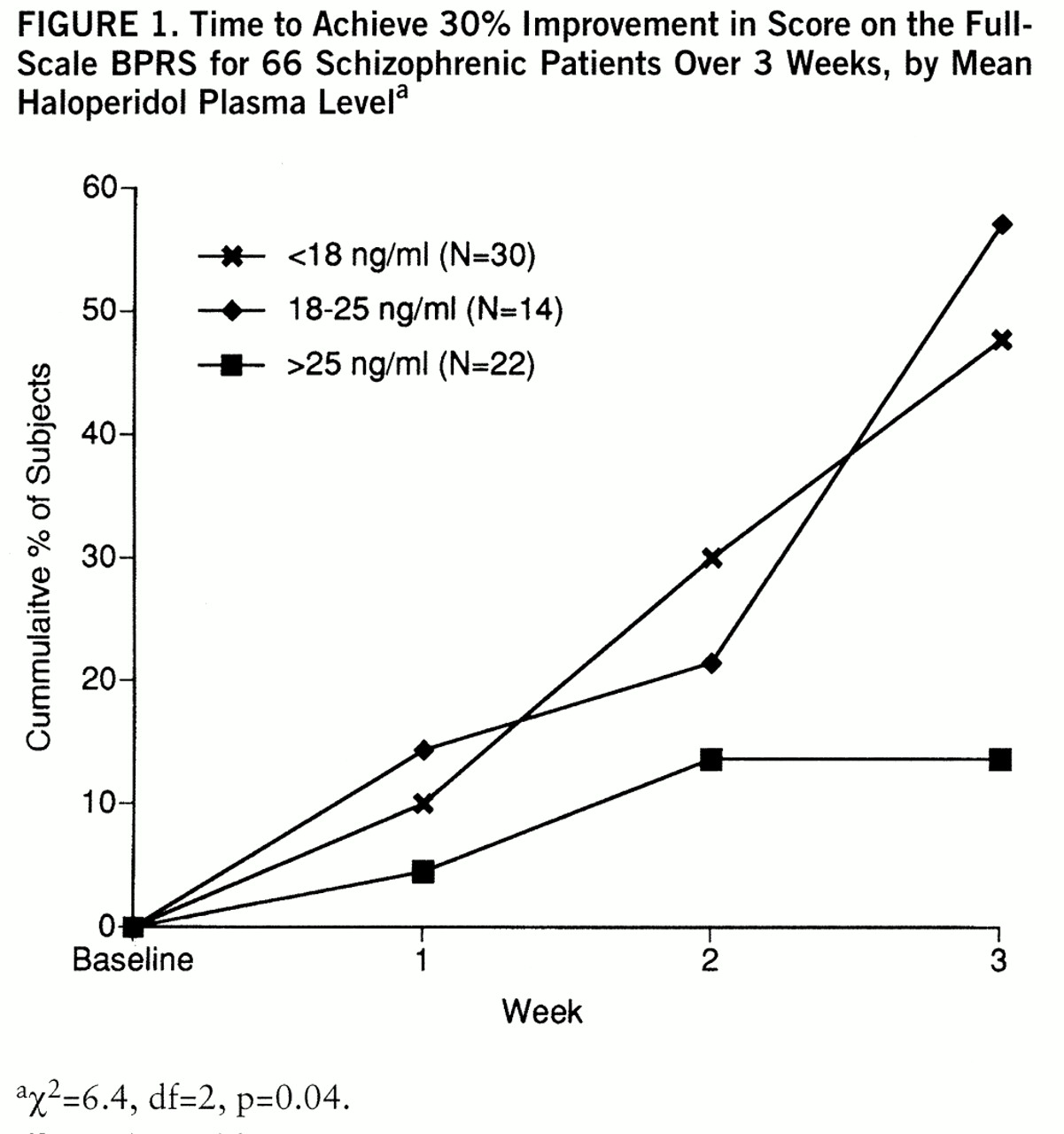
For the three plasma level groups, changes from baseline in rating scale scores did not differ significantly (
table 2). Nor did analyses of variance reveal any statistically significant associations between haloperidol plasma level, treated as a continuous variable, and any of the improvement scores listed in
table 2. The three groups did, however, differ in time to achieve the preselected threshold of 30% improvement in full-scale BPRS score (
figure 1). Those in the low- and intermediate-level groups were four to five times as likely to achieve this level of improvement. Those with high levels (greater than 25 ng/ml) differed significantly both from the intermediate-level group (χ
2=6.0, df=1, p=0.01) and the low-level group (χ
2=5.1, df=1, p=0.02). Improvement in negative symptom scores (χ
2=6.4, df=2, p=0.04), rather than changes in positive symptom scores (χ
2=0.9, df=2, p=0.60), accounted for most of this difference.
Despite these differences in symptom levels, the three groups had very similar, and generally quite low, levels of side effects. None of the subscale scores of the Simpson-Angus Rating Scale or the Hillside Akathisia Scale significantly differed across groups. The mean overall severity ratings of akathisia at the end of week 3, for instance, were 2.1 (SD=1.1), 2.2 (SD=1.6), and 2.1 (SD=1.4) for the low, intermediate, and high plasma level ranges, respectively (a score of 2 corresponds to a rating of “borderline” akathisia).
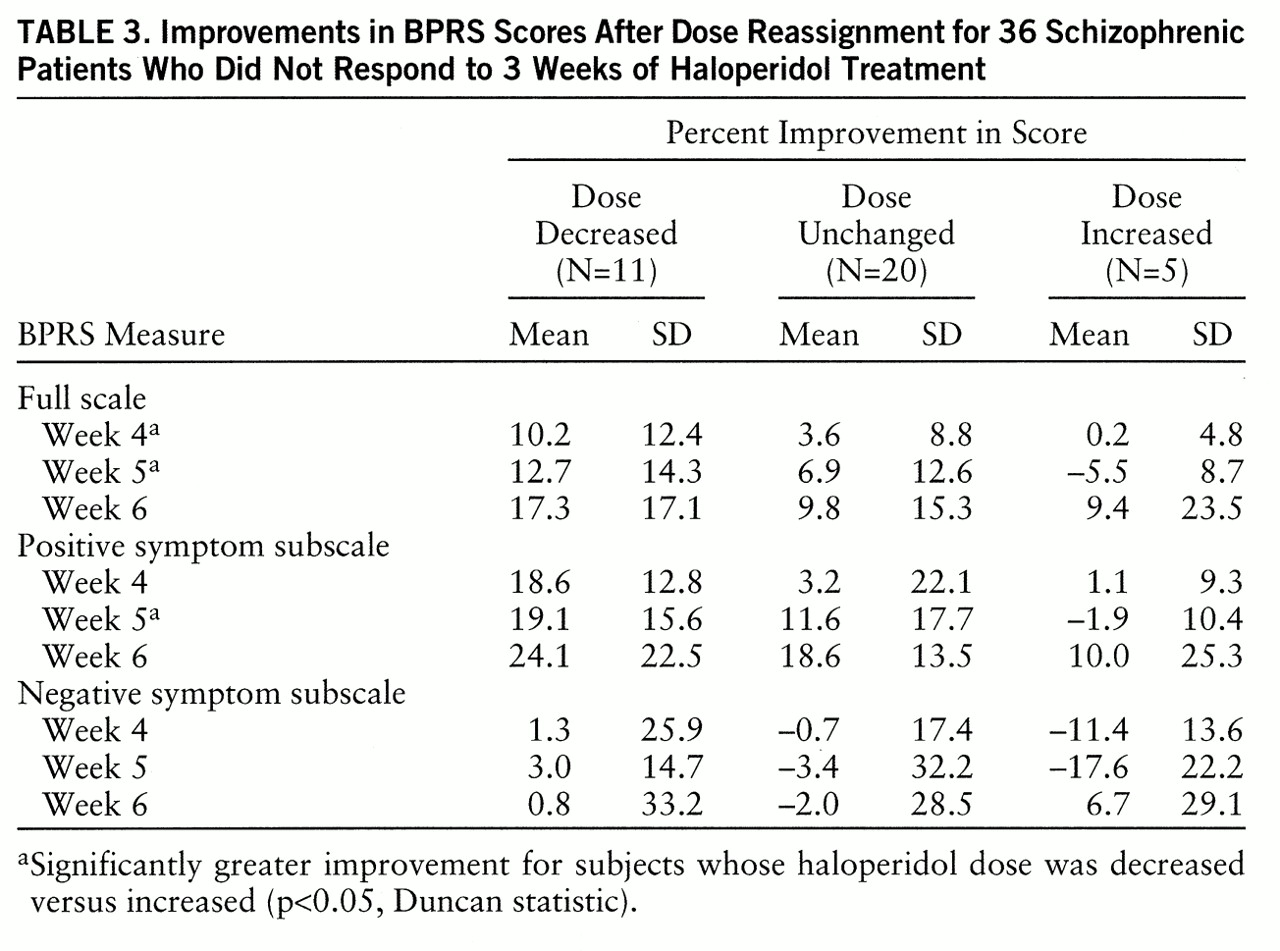
Of the 66 patients assessed at the end of week 3, 39 (59.1%) had scores on the full-scale BPRS that failed to improve by at least 30%. Of the 36 patients who subsequently remained in the study, five were randomly assigned to a higher dose, and 11 were assigned to a lower dose; the haloperidol dose of 20 subjects remained unchanged. More patients were assigned to a lower dose than to a higher one because all subjects who did not meet the response criterion were subject to reassignment, regardless of plasma level. Since patients in the moderate plasma level range (less than 18 ng/ml) were more likely to have improved, they were underrepresented in the pool of nonresponding subjects, and, consequently, relatively few were eligible to have their dose increased.
Among patients whose BPRS score had failed to improve by the requisite 30% after 3 weeks of haloperidol treatment, those assigned to a decrease in dose experienced significantly more improvement in the next 2 weeks than did those assigned to a dose increase (
table 3). This advantage persisted but was no longer statistically significant at week 6. Those assigned to receive the same dose had intermediate levels of improvement. Similar patterns emerged for both positive and negative symptom subscale scores.
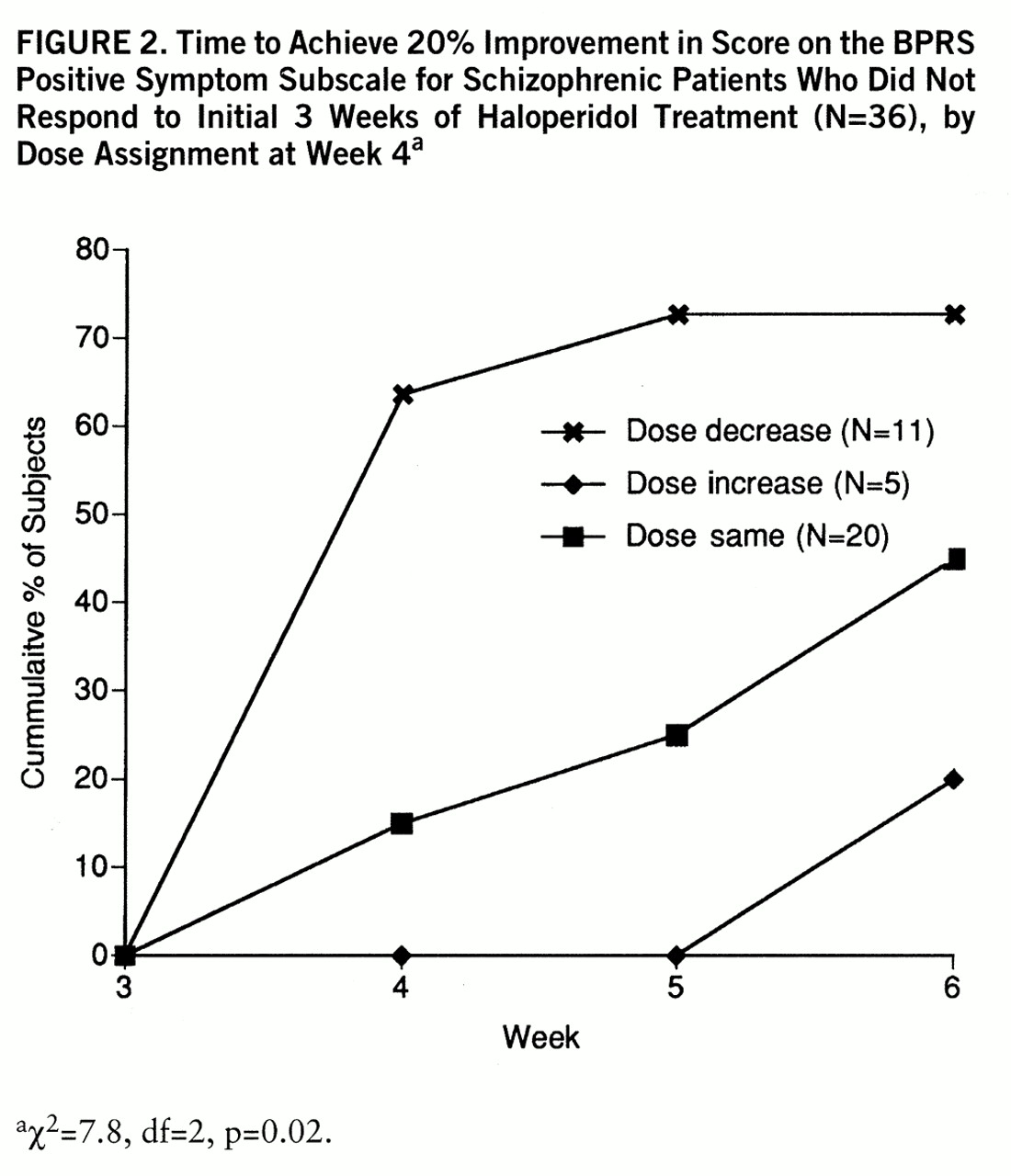
Survival analyses of time to achieve 20% improvement also favored those who had been assigned to a dose decrease. Patients who underwent decreases in their assigned haloperidol dose were significantly more likely to meet this threshold of improvement than were those whose assigned dose was increased (χ
2=4.9, df=1, p=0.03) or was not changed (χ
2=5.1, df=1, p=0.02). Changes in full-scale BPRS scores for the subjects whose doses were decreased did not differ significantly from those of subjects whose dose remained unchanged. Group differences in positive symptom subscale score changes, however, were more marked and were statistically significant (
figure 2).
Haloperidol plasma level groupings in the final 3 weeks were not significantly related to changes in BPRS score over that period. Among the 34 subjects who did not respond after the first 3 weeks and who then completed the protocol, the seven with mean haloperidol levels between 18 and 25 ng/ml had a mean improvement in full-scale BPRS score from weeks 3 to 6 of 8.1% (SD=7.1%). The 11 subjects with mean values above 25 ng/ml and the 16 with values below 18 ng/ml improved by 10.3% (SD=19.4%) and 16.4% (SD=15.4%), respectively.
Those who had improved by at least 30% at the end of week 3, and who therefore continued at the same dose, showed somewhat less overall improvement in BPRS scores in the final 3 weeks. Again, no significant relationship emerged between mean plasma levels achieved and symptom changes. The four with intermediate levels improved a mean of 7.1% (SD=0.9%), while those with high (N=5) and low (N=10) mean levels improved by 4.0% (SD=13.6%) and 9.4% (SD=24.8%), respectively.
As was the case at the end of week 3, haloperidol plasma levels were not significantly related to side effect ratings. Of the 10 Simpson-Angus scale scores rated, only “head dropping” significantly distinguished the groups (χ2=6.5, df=2, p=0.04). Hillside Akathisia Scale scores did not significantly differ across groups.
DISCUSSION
The analyses considered relationships between haloperidol plasma levels and clinical change in a variety of ways. Those relationships that did emerge consistently favored plasma levels less than 18 ng/ml over plasma levels that exceeded 25 ng/ml. The results suggest two clinical tools, one applicable when treatment is initiated and the other after some weeks have passed.
First, clinicians may use plasma levels after a loading dose to project doses that are likely to yield plasma levels less than 18 ng/ml. Alternatively, plasma levels at 1 week can be used to provide this feedback. The results of this and our earlier, nonoverlapping study (
5) suggest that patients who achieve levels in this range will reach target improvement levels sooner than those whose plasma levels are substantially higher. Second, in the face of inadequate improvement, the ascertainment of a steady-state plasma level may guide a clinician to lower doses when this level substantially exceeds 18 ng/ml.
The advantage of lowering doses when plasma levels exceed 18 ng/ml was statistically apparent even though power was limited by small cell sizes. While a lower limit to the haloperidol therapeutic plasma level range must exist, its quantity is a matter of debate (
28,
29), and the plasma level range indicative of inadequate dosing is more ambiguous. The receptor occupancy studies mentioned earlier, however, provide a theoretical lower limit of approximately 4 ng/ml.
We chose the upper limit of the therapeutic plasma level range on the basis of our earlier study and the median value of the various upper limits proposed in the literature. Because no clear correlation emerged between plasma levels and clinical change in the current study, we did not attempt to identify a more optimal range in the analysis. We suspect that plasma level/response relationships were less robust in this series than in our previous one because evolving referral patterns supplied smaller proportions of patients to our facility who had true responses to medication. Patients in the earlier series had a mean improvement in BPRS scores of 31.6% at week 3; the mean improvement at week 3 in the current series was 23.0% (t=1.5, df=56, p=0.13). The likelihood of discernible plasma level relationships decreases in direct proportion to the number of drug-resistant patients included in a cohort. Thus, the predicted effects of dose manipulation seen here may have been more robust in a cohort of patients recruited through private practitioners.
Also, the use of depot neuroleptics may have become more prevalent in this geographical area over the past decade. Although our exclusion criteria specified a minimum of 3 months from the last depot injection, this may have been insufficient. Residual effects of previously administered depot agents may have further obscured plasma level/response relationships.
The results of receptor occupancy studies are consistent with a lack of incremental clinical improvement as haloperidol plasma levels increase well beyond 10 ng/ml. They do not explain the finding that responses among patients with high plasma levels were inferior to those of patients with lower plasma levels, an inferiority manifest on both positive and negative subscale scores of the BPRS. Although the Simpson-Angus scale is designed to quantify adverse effects, it did not significantly discriminate among the plasma level groups. However, these measures may not be sufficiently sensitive to the adverse effects that are consequent to excessive plasma levels. Certain of these effects, such as akathisia or akinesia may, instead, mimic positive or negative symptoms, respectively. On the other hand, excessive levels may perturb neurotransmitter systems in ways that directly counter what might otherwise be beneficial effects. Whether or not one or the other, or both, of these possibilities occur, however, the literature now contains compelling evidence that haloperidol plasma levels well beyond 18 ng/ml offer no advantage over lower ones and are, in many cases, actually countertherapeutic.
These findings have relevance not only to optimal haloperidol dosing but also for initial selection of an antipsychotic. Newer antipsychotics such as olanzapine and risperidone are coming into wide use in the initial treatment of schizophrenia, despite costs that are many-fold higher than those for conventional antipsychotics such as haloperidol. These newer agents result in fewer extrapyramidal symptoms, and the results of at least one study suggest that they have superior efficacy (
30), but in that study, haloperidol doses were fixed at 20 mg/day. Evidence that the efficacy and tolerability of haloperidol can be substantially enhanced through the use of plasma level feedback is now substantial. Comparisons of the newer antipsychotics to haloperidol, given under these circumstances, are now clearly warranted.