The DSM-IV criteria for posttraumatic stress disorder (PTSD) include two aspects of sleep disturbance: recurrent nightmares, listed in the reexperiencing cluster (criteria B), and sleep continuity disturbances, listed in the hyperarousal cluster (criteria D). However, a careful analysis as to whether sustained sleep disturbances in chronic PTSD are specifically related to the impact of exposure to traumatic stress or are a consequence of comorbid disorders has not occurred. This is because of insufficient measurement and control of comorbid conditions, the lack of careful measurement of traumatic exposure, and the use of treatment-seeking patients who may not reflect the general population with PTSD. This study addressed these problems by examining the role of exposure to trauma, nonsleep PTSD symptoms, and comorbid medical and psychiatric disorders in contributing to different domains of sleep disturbance in a nationally representative community sample of male Vietnam veterans and two comparison groups.
We analyzed the questionnaire items that address specific complaints about sleep from the National Vietnam Veterans Readjustment Study (
1). That study was a major population-based study conducted in the late 1980s whose theater sample was selected to represent the entire group of 3.1 million men and women who served in the Vietnam theater. That study estimated the prevalence of current PTSD and other psychiatric disorders in Vietnam theater veterans in comparison to Vietnam era veterans and civilians. It remains the most comprehensive survey to date that examines the relationships among war zone exposure, PTSD, and postwar adjustment in multiple domains of psychosocial functioning. The goal of our study was to compare the frequency of nightmares and sleep continuity disturbances in combat veterans to that in Vietnam era veteran and civilian comparison subjects. We also sought to examine the role of combat exposure, comorbid psychiatric and medical disorder, and substance abuse in accounting for different domains of sleep disturbance.
Our hypothesis was that exposure to war zone trauma would be strongly linked to nightmares and less associated with sleep continuity disturbance. This hypothesis was guided by a published survey of 4,042 mono~zygotic and dizygotic Vietnam era veteran twins which found that combat exposure was highly correlated with reports of dreams and nightmares but only weakly associated with sleep onset and sleep maintenance insomnia (
2). Further, we hypothesized that nightmares would be related predominantly to combat exposure and less related to comorbid psychiatric disorder, substance abuse, and chronic medical illness.
METHOD
Subjects
The National Vietnam Veterans Readjustment Study is a cross-sectional survey of three groups: theater veterans (who served in Vietnam and the airspace and waters surrounding Vietnam), era veterans (who served on active duty in the U.S. Armed Forces during the Vietnam era but not in the Vietnam theater), and age- and gender-matched civilian comparison subjects. The sample consisted of 1,200 male theater veterans, 412 male era veterans, and 450 male civilian comparison subjects (
3). Subjects, identified by a national probability sampling strategy that drew from rural and urban areas in all 50 states, were interviewed in their homes through use of the National Survey of the Vietnam Generation (
1). After complete description of the study to the subjects, written informed consent was obtained. The Vietnam era veteran and civilian comparison subjects were matched by age and ethnicity, and the two groups were weighted to the theater veteran population.
The demographic characteristics, prevalence of PTSD, and comorbid psychiatric diagnoses of the three study groups have been previously reported (
3–
5). Most subjects were middle-aged, were married, and had attended some college.
Measures
The data analyzed in this study come from responses to the National Survey of the Vietnam Generation, which included the military and civilian version of the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder (
6). The case definition for PTSD in this study of sleep was based on a cutoff score of 81 on the Mississippi scale minus the five items pertaining to sleep. This cutoff score yields a prevalence of PTSD of 15.0% in male theater veterans, which is closely comparable to the 15.2% adjusted prevalence reported in the National Vietnam Veterans Readjustment Study (
3). We found that a PTSD case definition that used this criterion has a sensitivity of 72.7% and specificity of 83.6% when compared to the Structured Clinical Interview for DSM-III-R—Non-Patient Version (SCID-NP) (
7). This case definition was chosen over the modified National Institute of Mental Health Diagnostic Interview Schedule (DIS) PTSD module (
1,
8), which produced poor sensitivity when compared to the SCID-NP (
9).
The dependent variables in this study were derived from the responses to the five sleep items in the military and civilian versions of the Mississippi scale. All responses were made on a 1–5-point Likert scale ranging from low to high severity of sleep disturbance. The difficulty in sleep onset variable was derived from the mean of the two items that inquire about difficulties with sleep onset: “I fall asleep easily at night” (reflected so that a score of 5 meant that the subject “never” fell asleep easily) and “I am afraid to go to sleep at night.” The Pearson correlation coefficient for these two items is 0.41 (p<0.0001, N=1,167). The measure for nightmares was derived from the two items that refer to frightening dreams: “I have nightmares of experiences in the military [civilian scale uses “in my past"] that really happened” and “My dreams at night are so real that I waken in a cold sweat and force myself to stay awake” (r=0.60, p<0.0001, N=1,167). The measure for sleep maintenance difficulty uses the single item, “I fall asleep, stay asleep and awaken only when the alarm goes off.”
The independent variables used to predict disturbances in the three sleep domains include combat exposure, lifetime history of major depression, alcohol abuse, substance abuse, panic disorder, mania, current major depression, and current medical comorbidity. The combat exposure factor was derived from items that comprise four dimensions of war zone trauma: exposure to combat, exposure to abusive violence, deprivation, and loss of meaning and control. A second-order principal components analysis showed that the four dimensions of exposure could be combined into a single index, ranging from –1.0 to 1.0 (
1,
10). Veterans' self-reports of war zone exposure have been validated against studies of military records (
1). Lifetime and current comorbid psychiatric disorders were diagnosed by the DIS (
8). The factor for current medical comorbidity was based on responses to questions that asked if subjects had been bothered by any one of 32 chronic medical conditions (e.g., asthma, arthritis, diabetes, hypertension, kidney disease, seizures) within the past 12 months. These items were summed and recoded on a 5-point ordinal scale ranging from 0 to 4 (
1,
11).
Statistical Analysis
The National Vietnam Veterans Readjustment Study data were obtained by a stratified, weighted sampling strategy that violates the simple random sampling assumptions of the common statistical packages. In this situation, common statistical procedures produce accurate point estimates (when properly weighted), but inaccurate (typically underestimated) variances, with the consequence of type I errors in statistical tests (
12). Therefore, we performed all statistical tests by using SUDAAN (
13), a software package for the analysis of complex survey data. SUDAAN uses a first-order Taylor series approximation to estimate variance for data sampled under complex survey designs. Both the raw and weighted sample sizes for each group are presented in this report.
Our sample varies slightly from the complete data set for the National Vietnam Veterans Readjustment Study (
1) in that we have excluded 33 of the 1,200 theater veterans, one of the 412 era veterans, and 65 of the 450 civilian veterans because of missing data. The cases selected for the current study did not differ on demographic variables from the full National Vietnam Veterans Readjustment Study data set.
We constructed hierarchical regression models to determine the association between the outcome variable for nightmares and the following set of predictors: combat exposure, nonsleep PTSD symptoms, current and lifetime depression, alcohol and substance abuse, lifetime panic disorder, mania, and chronic medical illness.
RESULTS
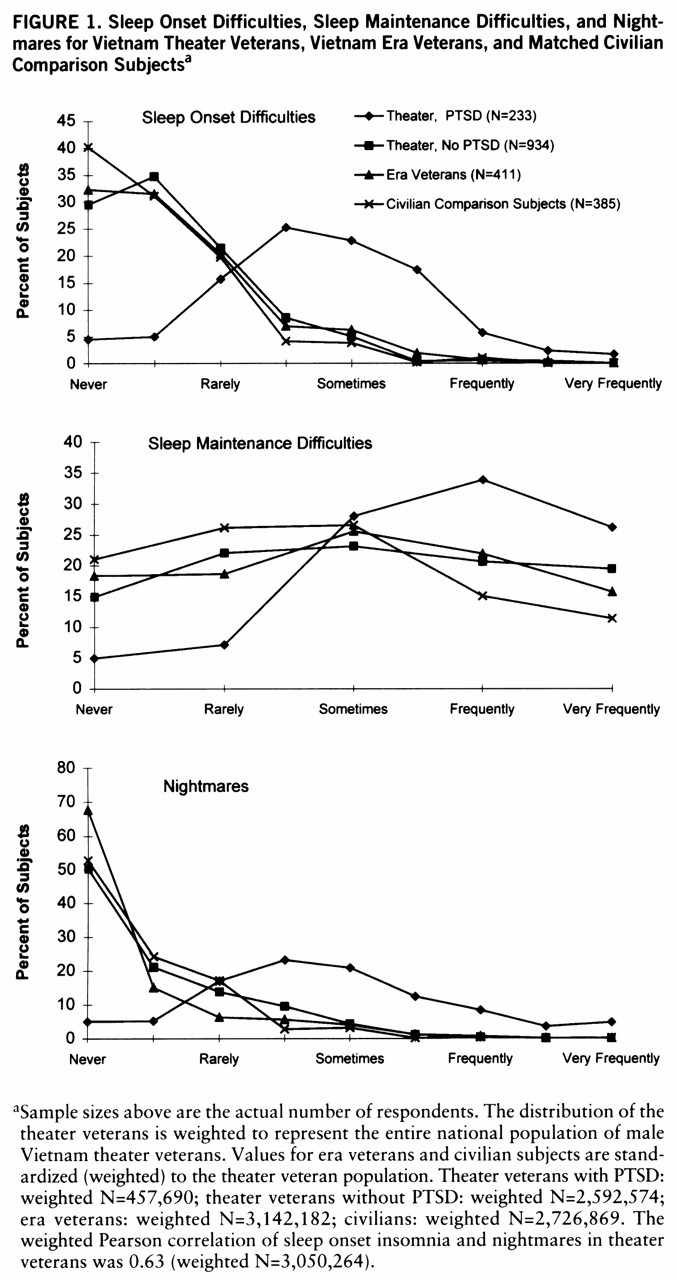
Male theater veterans with current PTSD at the time when the National Vietnam Veterans Readjustment Study was conducted reported more disturbances in all three domains of sleep. Difficulties with falling asleep occurred with a frequency varying from “sometimes” to “very frequently” in 44.0% of combat veterans with PTSD, 5.5% of combat veterans without PTSD, 9.4% of era veterans, and 5.0% of civilian comparison subjects (χ
2=126.0, df=24, p<0.0001) (
figure 1). Difficulties staying asleep occurred sometimes or more frequently in 90.7% of combat veterans with PTSD, 62.5% of combat veterans without PTSD, 63.1% of era veterans, and 52.9% of civilian subjects (χ
2=52.2, df=12, p<0.0001). Nightmares occurred sometimes or more frequently in 52.4% of combat veterans with PTSD, 4.8% of combat veterans without PTSD, 5.7% of era veterans, and 3.4% of civilian subjects (χ
2=185.4, df=24, p<0.0001). Frequent or very frequent nightmares and difficulties with falling asleep were found exclusively in subjects with PTSD.
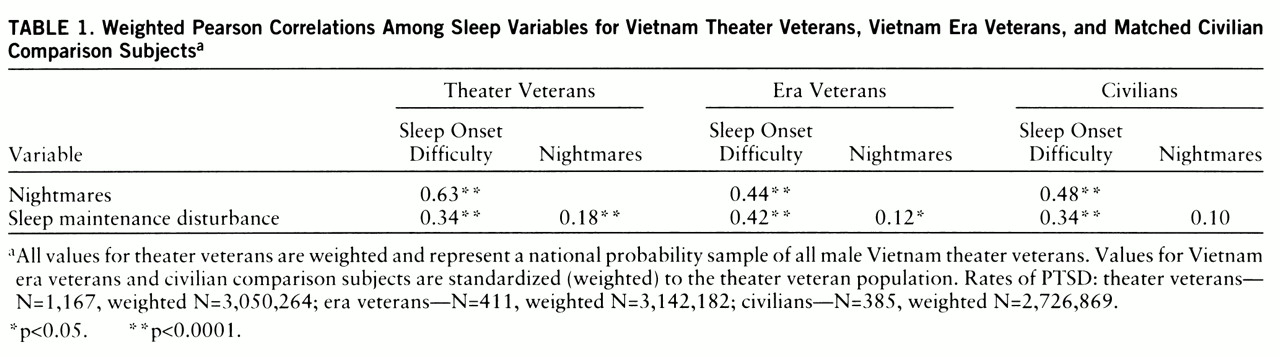
The correlations among the three domains of sleep in the three groups are shown in
table 1. Not surprisingly, the sleep onset and nightmare variables were highly correlated in the Vietnam theater group given that one of the sleep onset items asks subjects if they are “afraid to fall asleep.” The Pearson correlation coefficient between the item “afraid to fall asleep” and nightmares was 0.63 (p<0.0001, N=1,167), compared to 0.48 between “fall asleep easily” and nightmares. We retained sleep onset and nightmares as separate variables because they are different facets of sleep disturbance that are distinguished by those with PTSD.
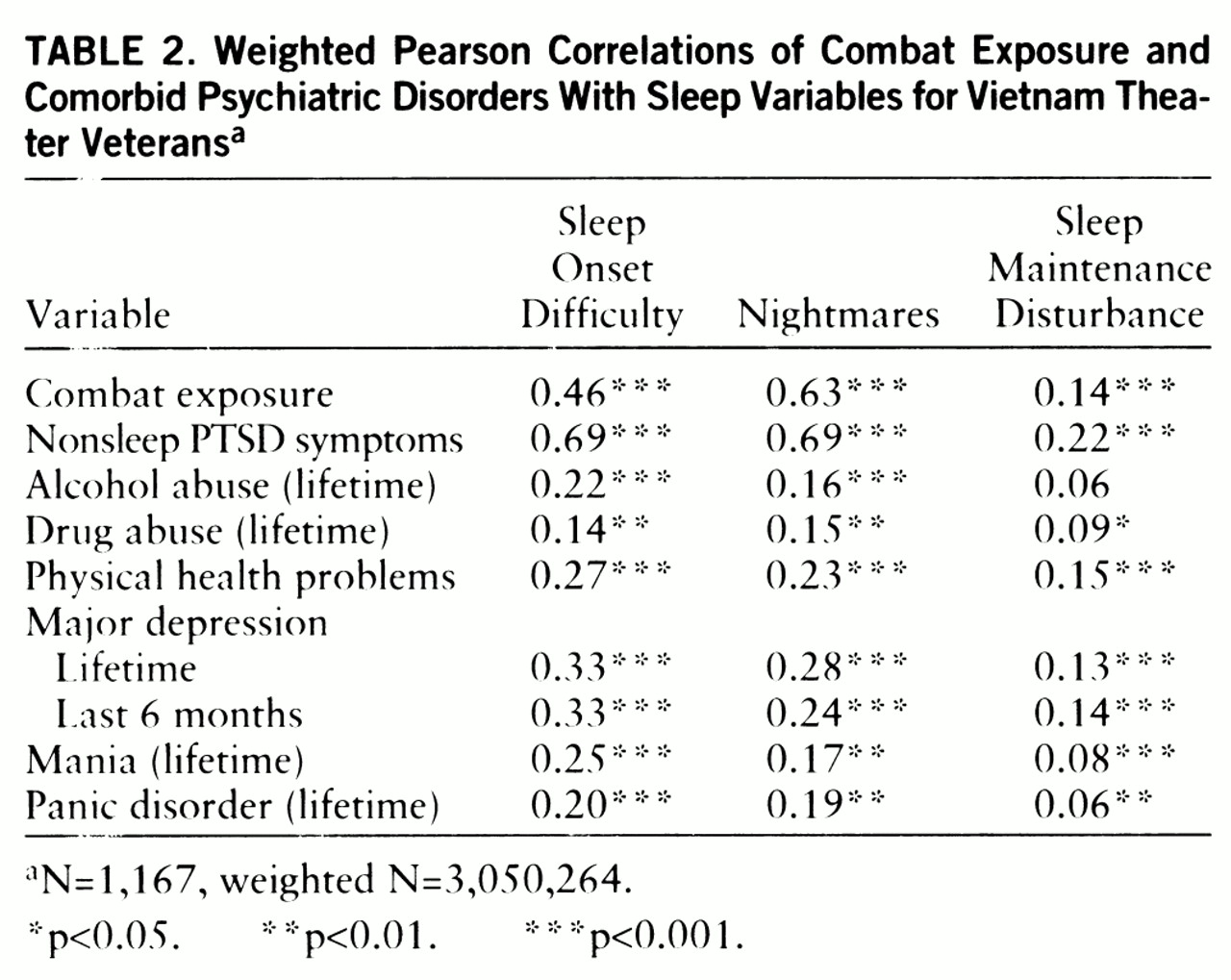
Table 2 shows the correlation matrix of the predictor and sleep variables in the combat veteran group. Of interest, combat exposure was strongly correlated with frequency of nightmares, moderately correlated with sleep onset insomnia, and weakly correlated with disrupted sleep maintenance.
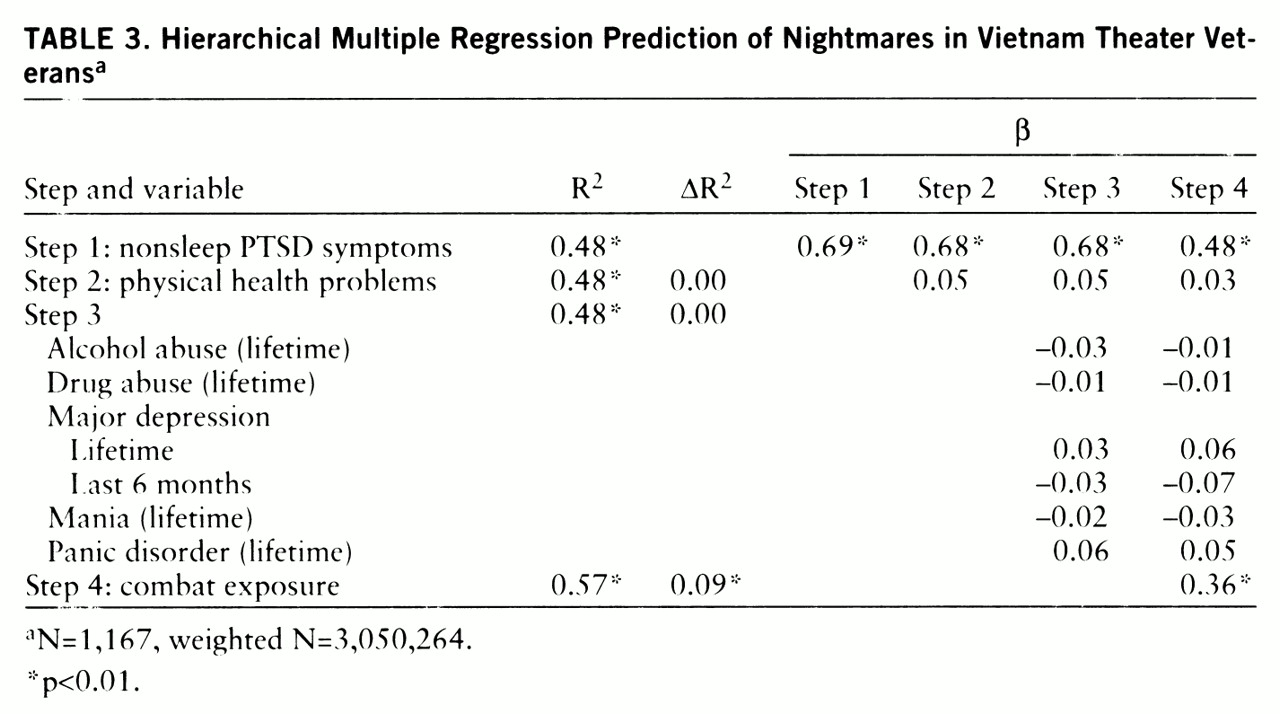
A hierarchical multiple regression model was developed to explain nightmares in Vietnam theater veterans. In this model (
table 3), nonsleep PTSD symptoms accounted for 48% of the variance in nightmare frequency. Adding physical health problems, comorbid psychiatric disorder, and substance abuse to the model accounted for less than 1% of incremental variance. When an alternative model was developed in which physical health problems were entered first, followed by comorbid psychiatric disorder and substance abuse, these variables explained 5% and 11% of the variance, respectively. However,
table 3 demonstrates that these variables do not contribute to unique variance not explained by the presence of nonsleep PTSD symptoms. The addition of the final predictor variable, combat exposure, yielded an additional 9% of the variance.
DISCUSSION
We found that for male veterans, frequent nightmares were virtually specific for those diagnosed with PTSD at the time of the survey and that combat exposure was highly associated with nightmares, moderately associated with sleep onset insomnia, and only weakly related to sleep maintenance insomnia. Our data are consistent with the results of the twin study (
2), which showed that combat exposure was highly correlated with reports of dreams and nightmares and only weakly associated with sleep maintenance insomnia. This observation is also consistent with several other studies that show a low to moderate correlation between nightmares and other domains of sleep disturbance (
14,
15). The nightmare appears to be the primary domain of sleep disturbance related to exposure to war zone traumatic stress. Further, our findings show that the frequency of nightmares has a strong relationship to level of exposure to war zone trauma even after accounting for nonsleep PTSD symptoms, comorbid psychiatric disorders, substance abuse, and general medical illness. In a manner similar to the acquisition of agoraphobia in individuals with panic disorder, we speculate that sleep onset insomnia in PTSD subjects is driven predominantly by sleep phobia resulting from the experience of frequent nightmares.
There are several limitations of this study that are a consequence of the cross-sectional design of the National Vietnam Veterans Readjustment Study, the retrospective measurement of combat exposure, and the lack of standardized measures of sleep disturbance. Recent prospective data from studies of Gulf War veterans suggest that the development of PTSD symptoms may amplify the recall of combat exposure (
16). Thus, the correlation between combat exposure and nightmares might be influenced by this phenomenon. Further, the experience of frequent nightmares could contribute to an increase in the recall of traumatic experiences (
17). The longitudinal course of sleep disturbances in PTSD awaits a future hypothetical study in which sleep in a population at high risk for exposure to trauma is studied at baseline and longitudinally after exposure to traumatic stress, after development of PTSD, and after the emergence of comorbidity.
The National Vietnam Veterans Readjustment Study did not use a standardized self-report measure of sleep quality. However, the domains of sleep analyzed here are easily identified and have been assessed with single items in validated instruments. For example, sleep onset, sleep maintenance, and disturbed dreams are assessed with single items in the Pittsburgh Sleep Quality Index, which has been shown to be highly reliable and valid when referenced to polysomnography (
18).
The low correlation between our sleep continuity measure and current major depression may suggest that this single item is an insufficient measure. It is also possible that it reflects the fact that most depressed subjects in the National Vietnam Veterans Readjustment Study also had PTSD (
11). Given that 90.7% of PTSD subjects reported sleep maintenance difficulties sometimes or more frequently, it is possible that the effects of depression were obscured. Several investigators have suggested that depression in the presence of PTSD may be biologically modified and hence may display different sleep characteristics (
19,
20). Dow et al. (
21) showed that subjects with both PTSD and major depression had shorter sleep latencies and higher sleep efficiency than subjects with depression alone. More studies of sleep in individuals with PTSD, with and without depression, are needed to clarify this issue.
Ross and colleagues (
22) have reviewed the prevalence of nightmares in normal and clinical populations and have suggested that anxiety dreams are relatively specific to PTSD. Historically, nightmares have long been postulated as being a hallmark feature of responses to traumatic stress (
23–
27). Hartmann, in his studies of frequent nightmare sufferers, found that adult exposure to violent assault increased nightmare frequency; however, he was not able to find a history of early childhood trauma (
28). He and others obtained data from frequent nightmare sufferers and suggested that these individuals were distrustful, schizoid, and alienated but not psychotic (
29,
30). Kales et al. (
30) also found that the onset of nightmares was preceded by “major life events.” The National Comorbidity Survey estimates that the lifetime prevalence of PTSD in the U.S. population is 7.8% (
31). It is possible that prior surveys of frequent nightmare sufferers did not account for the presence of PTSD.