The prevalence of bulimia nervosa in persons seeking treatment has been rapidly increasing since the first description of the disorder by Russell in 1979 (
1). Psychological treatments for bulimia nervosa that produce good improvement of symptoms have been developed. These treatments require specialized therapists and from 14 to more than 40 sessions (
2–
6). Pharmacological treatment with fluoxetine (at a dose of 60 mg/day) is less labor-intensive but produces an abstinence rate of only 20%–30% (
7), in contrast to psychological treatments provided by specialized therapists (e.g., an abstinence rate of 50% for cognitive behavior therapy [2]).
A self-care manual for sufferers of bulimia nervosa that contains cognitive behavior educational and treatment strategies (
8) was translated into German by the first author's research team in 1996. The English version had been examined in a randomized, controlled trial and produced an abstinence rate of 20% (
9). In a staged approach, use of the self-treatment manual followed by up to eight sessions of cognitive behavior therapy, as required, was found to be as effective as 16 sessions of cognitive behavior therapy, both at the end of treatment, when 30% of the sequential treatment group and 30% of the standard treatment group were free from all bulimic symptoms, and at 18-month follow-up, when 40% of the sequential treatment group and 41% of the cognitive behavior therapy group were symptom free (
10). A proportion of patients were poorly compliant with the instructions in the manual, and this may explain the sub~optimal response (
11). In the present study the manual was used in conjunction with cognitive behavior therapy—in the form of guided self-change—in a design similar to that of a pilot study which used a different manual in the context of a different method of providing health care (
12).
The aim of this study was to evaluate whether guided self-change with eight sessions of cognitive behavior therapy was as effective as 16 sessions of standard cognitive behavior therapy. We opted for guided self-change rather than a stepped-care approach because there is no self-care culture in Germany, and there is skepticism on the part of both patients and clinicians about shorter and less costly treatments (
13). There is an overdependence by patients on professional care, except for self-help groups, which provide support and information on treatment rather than treatment itself. In addition, there is resistance to self-care among health care professionals, probably for economic reasons and out of true concern for their patients. In Germany's therapeutic culture there is a heavy bias toward insight-oriented psychodynamic treatments, especially in university departments of psychosomatic medicine rather than departments of psychiatry (
14). This bias might in part be a backlash from the persecution of the Jews during the Third Reich; they provided the vast majority of psychoanalysts at that time. In addition, psychoanalysis was not welcomed in the German Democratic Republic, and therefore in that part of Germany, it is largely thought of as the treatment preferred by intellectuals who were in opposition to the ruling power in the German Democratic Republic. The German insurance system pays for psychodynamically oriented treatments and behavior therapy, even on an inpatient basis; however, it has not yet included newer forms of treatment.
We predicted that in a German setting, compliance would be poor in a stepped-care design. In contrast to the insurance system in Germany, which pays for long-term dynamic psychotherapy, in the United Kingdom private health care insurance does not cover outpatient psychotherapy. Most research is done within the National Health Service, where there is an implicit recognition of rationing, and short-term treatments are favored. Thus, experience in the use of minimal treatments in the United Kingdom may not be generalizable to other cultures where there are different expectations about treatment. An additional reason for the design chosen for this study is that one potential disadvantage of a stepped-care approach is that patients who have “failed” in the early stages of treatment may feel less motivated to carry on, losing confidence in their ability to succeed.
There is abundant evidence (
15–
18) that bulimic patients do not improve while they are on a waiting list and may even deteriorate. In a previous study that used the English version of this manual (
9), a waiting list control group was included and showed no clinically significant change. We therefore decided not to include a waiting list control group in the present study.
Our hypothesis was that guided self-change would be as effective as the standard cognitive behavior therapy, but with a reduced number of therapist-led sessions. We also predicted that a self-care manual that includes relapse prevention skills would lead to sustained, rather than transient, recovery at follow-up.
METHOD
Family physicians, psychiatrists, gynecologists, and various counseling services in and around Bielefeld, a town in Germany with 320,000 inhabitants, were invited to refer patients aged 15 years or older who complained of symptoms suggesting bulimia nervosa (the clinical picture of which was briefly described). An article about our bulimia proj~ect in a local newspaper also led to several self-referrals. Patients were assessed by one of three therapists, but not the one who later treated them. The assessors determined whether the patients met the DSM-III-R criteria for bulimia nervosa. After complete description of the study to the patients, written informed consent was obtained. Patients who both met the DSM-III-R criteria and gave informed consent were included in the study. If there had been recent improvement in a patient after a prolonged period of DSM-III-R-defined bulimia nervosa, the patient was offered treatment in the study even though the DSM-III-R criteria were not fully met at the baseline assessment. Recruitment continued until 62 patients had entered the study; 31 patients were allocated to each of the two treatments on an alternating basis.
Both treatment modalities were carried out on an individual outpatient basis. They consisted of either 16 weekly or eight fortnightly treatment sessions within the limits of availability of therapist and patient; thus, the duration of the two treatments was similar, but the intensity of therapist involvement was different (i.e., eight versus 16 sessions in which there was contact). The sessions lasted 50–60 minutes for both treatments. One of the patients was already in psychodynamic psychotherapy when she sought help for her eating problem. No other patient had psychotherapy or treatment with psychoactive drugs during treatment in the study.
Cognitive behavior therapy followed the principles outlined by Fairburn et al. (
19), Freeman (
20), and Schmidt and Treasure (
8). The cognitive aspects of this therapy are mainly directed at overvalued ideas regarding weight and shape, with emphasis also on problem-solving skills and core maladaptive assumptions. Psychoeducation is used to correct faulty ideas about the effect of dieting, vomiting, and laxative and diuretic abuse on weight and shape. Behavioral approaches are used to introduce a healthy diet and to eliminate vomiting and abuse of laxatives and diuretics.
In the guided self-change group, less time was spent on the educational and skills-training aspects of cognitive behavior therapy, since these were covered in the self-treatment manual. In sessions 1–4, therapist and patient worked with chapters 1–6 of the self-treatment manual. In short, these deal with 1) motivation; 2) keeping a food diary; 3) information on biological and cultural influences on actual and desired weight and shape, the advantages of a healthy diet versus the dangers of starvation, and ways to regain control over eating; 4) information on and strategies to deal with binge eating, vomiting, and other weight-control measures; and 5) how to learn to like one's own body. Thereafter, therapist and patient chose the most relevant additional chapters to focus on during the remaining sessions. Generally, therapy sessions were used to help and encourage the use of the book and to tackle obstacles such as poor motivation, depression, and acute crises.
At the end of treatment, therapist and patient reviewed progress and discussed further treatment options. Additional therapy was one of the outcome measures.
Treatment was conducted by three female part-time therapists. All were trained in several approaches to psychotherapy. Two of the therapists were psychologists, and one was completing her postgraduate Diploma in Health Sciences. Each therapist was trained to implement the forms of treatment we have described. During the treatment phase of the study, the therapists met once a week with the first author to discuss hurdles in using the treatments. Each therapist treated equal numbers of patients from the two treatment conditions. Probands were assigned to one of the therapists as they became available.
Assessments
All of the assessments were done by the therapists involved in the study for patients whom they did not treat or by the first author. The therapists were trained by the first author—an experienced psychiatrist who had received detailed training at the Maudsley Hospital, the Institute of Psychiatry, and the Medical Research Council Institute of Social Psychiatry in London—to use the instruments described below.
Eating and attitudes toward eating, weight, and shape were measured with use of the Eating Disorder Examination (edition 11.5, unpublished instrument by C.G. Fairburn). This investigator-based, semistructured interview covers the clinical picture of bulimia nervosa. It assesses in detail the patient's state during the preceding month in terms of both behavior and attitudes.
On the basis of information from the Eating Disorder Examination, the interviewer made a DSM-III-R diagnosis of bulimia nervosa and assessed global severity of the disorder on a scale of 1–5 points (1=fully recovered, no serious concerns regarding shape and weight, 2=mild residual symptoms, 3=moderate residual symptoms, 4=meets DSM-III-R criteria for bulimia nervosa, 5=severe bulimia nervosa).
We also used the patient-rated Bulimic Investigatory Test Edinburgh (
21). It includes questions on eating habits and concerns about eating, shape, and weight as found in bulimia nervosa.
The Structured Clinical Interview for DSM-III-R (
22) was used to determine additional psychiatric morbidity at the first assessment only. In addition, subjects made self-ratings on the Beck Depression Inventory (
23) and the Self-Concept Questionnaire (
24), which measures self-esteem.
The subject-rated Eating Disorders Awareness Test (
25) was used to assess the patients' knowledge about issues relevant to eating disorders (nutrition, weight control, etc.).
Between 6 months and well over 2 years after the end of therapy (mean=43 weeks, SD=25, median=40, range=23–123), the 62 patients originally assigned to treatment were contacted by letter—and if that failed, by telephone—and invited for a follow-up interview and completion of questionnaires. This assessment included the Eating Disorders Examination, severity scale ratings, and the self-report ratings on the Bulimic Investigatory Test Edinburgh, Beck Depression Inventory, Self-Concept Questionnaire, and Eating Disorders Awareness Test. Ten patients had moved and could not be traced. One had moved too far to attend the interview but completed the questionnaires, one declined to attend the assessment session, one never answered letters and phone calls, and two did not keep their appointments.
Statistical Analysis
This study was a treatment evaluation trial, testing whether guided self-change was a therapist-time-saving alternative to standard cognitive behavior therapy. Therefore, we analyzed the course of all patients who undertook treatment. Patients who left treatment prematurely had their last known assessment (baseline or midtherapy) carried forward as the midtreatment and/or end-of-treatment record. In contrast, during follow-up, no carrying forward was done, and only the patients who completed the follow-up a mean of 43 weeks (SD=25) after the end of therapy were included in the analyses. Analysis of covariance was used to study whether additional treatment undertaken during this period influenced outcome. We used t tests for differences between treatments in effects on main outcome measures either across therapy time or across follow-up time and also to test for differences between groups in demographic data. Two-factor analyses of variance for repeated measures were calculated. The greater the number of repeated measures, the greater the likelihood of violating assumptions of sphericity and normality (
26). Therefore, we present the most conservative F values. These are obtained by setting epsilon to its lower bound, which represents the maximum violation of these assumptions (
27,
28). When a significant result is obtained, it is assumed to be robust. However, since this test may be overly conservative, Greenhouse and Geisser (
27,
28) recommend that when the lower-bound epsilon gives a nonsignificant result, it should be followed by an approximate test (based on a sample estimate of epsilon).
Yates-corrected chi-square tests were used for categorical data. Confidence interval analysis (
29,
30) was carried out for abstinence rates only. Patients were classified as fully recovered if they were not binge eating or vomiting. Since only one patient seriously abused laxatives, this variable was omitted. The main outcome measures were the Eating Disorder Examination subscores for overeating (items 9, 10.1, 10.2, 12.1, and 19.1), vomiting (items 25.1 and 25.2), dietary restraint (items 2–6), shape concern (34.1, 35, 36.1, 38.1, 39, and 40), and weight concern (33.1, 33.2, 35, 37.1); the 5-point severity scale regarding the DSM-III-R diagnosis of bulimia nervosa based on the Eating Disorder Examination interview; and the Bulimic Investigatory Test Edinburgh score. Subsidiary outcome measures were scores on the Beck Depression Inventory, Self-Concept Questionnaire, and Eating Disorders Awareness Test and whether probands had additional treatment after the end of therapy. Data were analyzed with use of the SPSS program (
31).
RESULTS
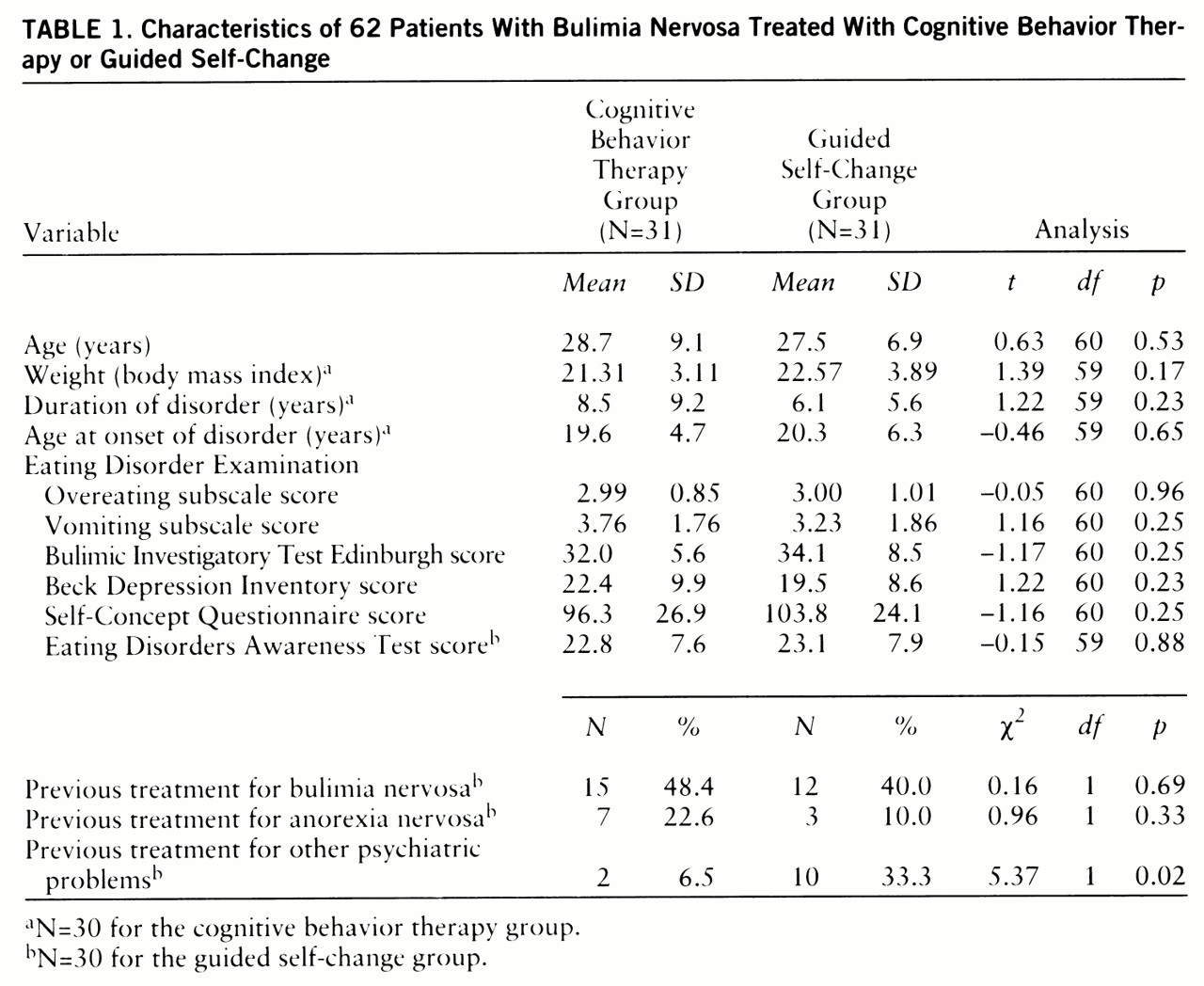
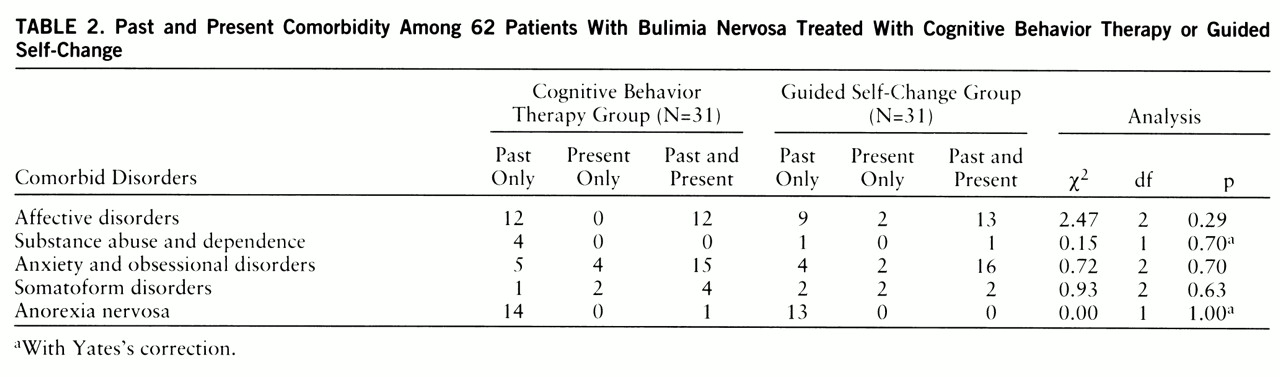
All 62 patients met the DSM-III-R criteria for bulimia nervosa either at baseline or within the preceding month. Fifty-five (88.7%) of the patients practiced self-induced vomiting; four (7.3%) of these also took laxatives to influence their shape and weight, but only one did so more than once a month. Seven patients (11.3%) neither vomited nor took laxatives but restricted their eating or exercised sufficiently to meet the DSM-III-R criteria. Sociodemographic and clinical details at the time of the first assessment are shown in
table 1 and
table 2. In the guided self-change group, previous treatment for psychiatric problems other than eating disorders was reported more frequently. There were no significant differences between treatment groups on any of the other variables.
Thirteen subjects (21.0%) dropped out during the treatment phase of the study: nine (29.0%) of the 31 in the guided self-change group and four (12.9%) of the 31 in the cognitive behavior therapy group. The difference was not statistically significant (χ2=1.56, df=1, p=0.21, with Yates's correction).
Fourteen (22.6%) of the original study group were not assessed at follow-up. There were no significant differences between the groups in terms of the proportion of patients responding to the follow-up: 74.2% (N=23) of the 31 subjects in the guided self-change group and 80.6% (N=25) of the 31 in the cognitive behavior therapy group responded. The patients who were not assessed at follow-up differed from those who completed the follow-up assessment on the following clinical features only: at first assessment they had higher scores on the Bulimic Investigatory Test Edinburgh (t=1.99, df=60, p=0.05) and lower scores on the Eating Disorders Awareness Test (t=1.99, df=59, p=0.05). Regarding the effect of treatment, the patients who did not complete the follow-up assessment improved as much as the rest of the patients on all variables except Eating Disorders Awareness Test score, for which there was a smaller difference for noncompleters between baseline and end-of-treatment assessments according to their last known assessment. There was no significant difference between the patients who completed follow-up and the rest on any other measure, including abstinence rate.
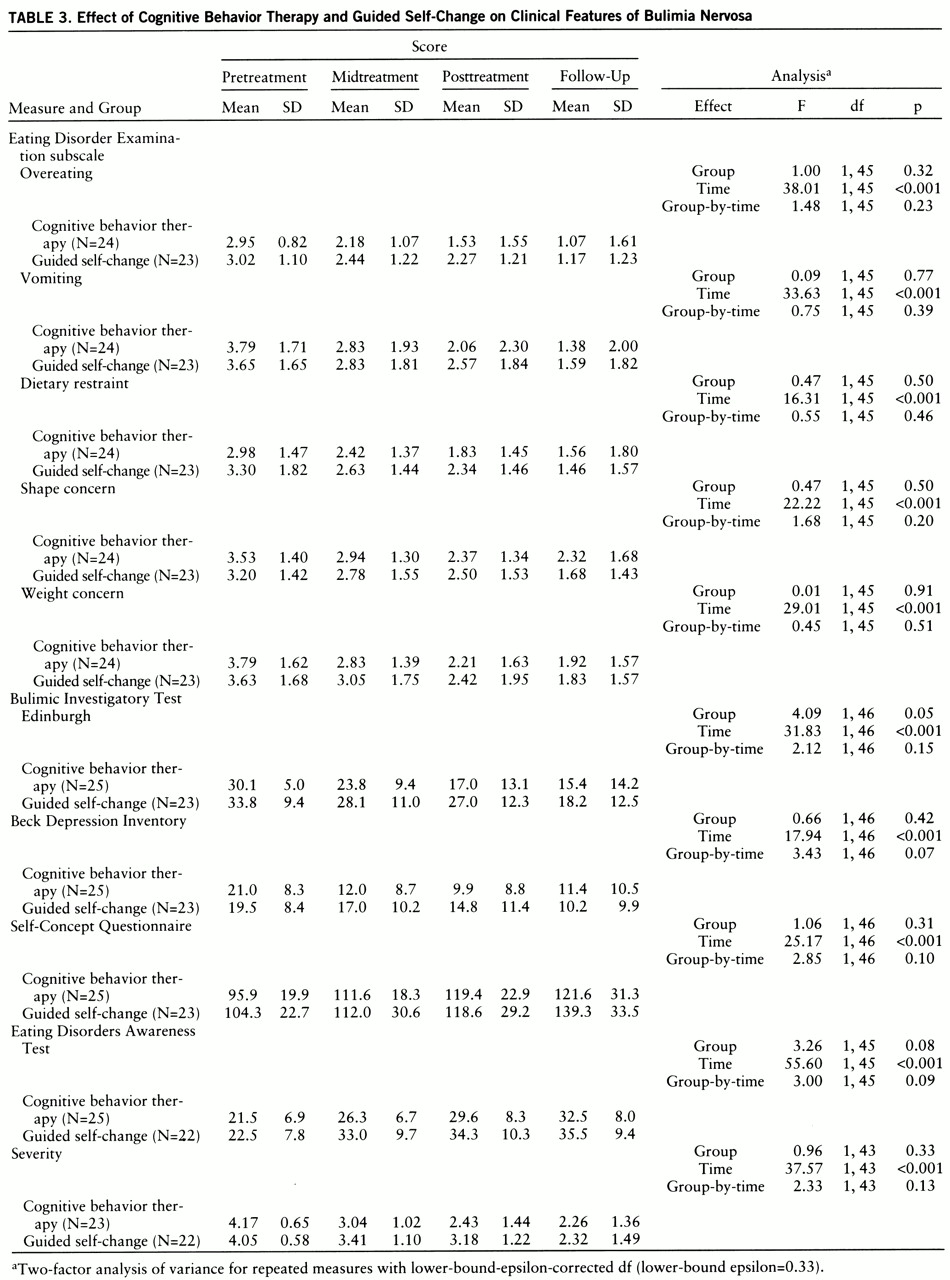
Both cognitive behavior therapy and guided self-change led to significant improvement according to the overeating, vomiting, dietary restraint, shape concern, and weight concern subscales of the Eating Disorder Examination, and this continued during the time of follow-up (
table 3). Therapy effects differed significantly between the groups on the Bulimic Investigatory Test Edinburgh only. There were no treatment-by-time interactions (
table 3). When the nonsignificant F values were recalculated on the basis of the approximate rather than the conservative epsilon as suggested by Geisser and Greenhouse (
27,
28), the results were essentially unchanged; all but two of the nonsignificant results remained nonsignificant at the 0.05 level. Only the interaction terms (treatment by time) for Beck depression scores and Eating Disorders Awareness Test (knowledge) scores became significant (F=3.43, df=2,107, p<0.05, and F=3.00, df=2,97, p<0.05, respectively). As can be seen from
table 3, subjects in the cognitive behavior therapy group appear to have had a faster reduction in levels of depression than those in the guided self-change group, while subjects in the guided self-change group showed a faster increase in their knowledge than those in the cognitive behavior therapy group. However, by the time of follow-up the two groups had quite similar Beck depression scores and Eating Disorders Awareness Test scores.
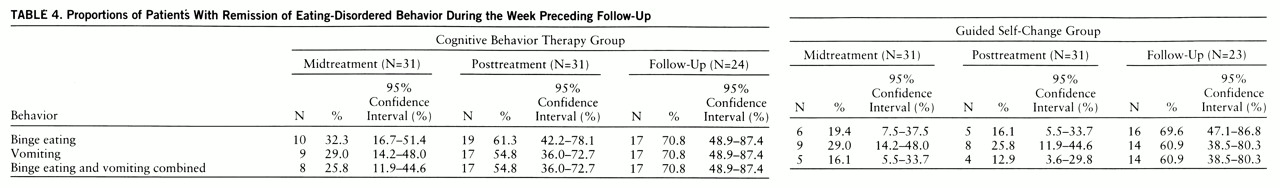
Table 4 shows the proportions of patients assigned to the two treatment groups who had stopped binge eating and vomiting during the week preceding assessment. At the end of therapy, 54.8% of the cognitive behavior therapy group and 12.9% of the guided self-change group had not binged or vomited during the preceding week. At follow-up, there was a significant increase in the percentage of subjects in the guided self-change group who had stopped binge eating and vomiting—60.9%. In the cognitive behavior therapy group, the proportion rose to 70.8%.
The two treatment modalities did not differ significantly in decreasing the likelihood of binge eating or vomiting at follow-up (difference=10%, 95% confidence interval=–17% to 37%) (see also
table 4).
An analysis of covariance showed that additional treatment did not explain the improvement made during follow-up for either the cognitive behavior therapy group or the guided self-change group.
In general, the changes in the subsidiary outcome measures paralleled those in the main outcome variables (
table 3). One difference was that the guided self-change group had more knowledge about issues related to eating disorders at the midtreatment assessment. In addition, at follow-up their self-esteem was higher.
There was a significant difference between cognitive behavior therapy and guided self-change with respect to their effects on body mass index (t=2.41, df=59, p=0.02). The change was not clinically significant; for the guided self-change and cognitive behavior therapy groups combined, the mean body mass index was 21.95 (SD=3.56) at baseline and 21.93 (SD=3.11) at follow-up. At follow-up, weight had increased significantly in the subgroup of patients who had stopped binge eating and vomiting; the mean body mass index was 21.63 (SD=2.83) before treatment and 22.28 (SD=3.26) at follow-up (t=–2.59, df=19, p=0.02).
Of the 47 patients who completed the follow-up, 20 (43.5%) had not taken an oral contraceptive at any stage of the study. Four of them had had either irregular or no menstruation at baseline. One of them had a regular cycle at follow-up.
There were no significant differences between cognitive behavior therapy and guided self-change in the number of patients who had additional treatment after the trial. Of those who provided information about further interventions, 44% (N=11 of 25) of the guided self-change group and 32% (N=8 of 25) of the cognitive behavior therapy group sought extra treatment (χ2=0.34, df=1, p=0.56). Patients who had not recovered at follow-up sought extra treatment more often than those who had recovered: three (16.7%) of the 18 who had fully recovered and 13 (50%) of the 26 who had not recovered had had further treatment (χ2=3.77, df=1, p=0.05).
DISCUSSION
Self-care manuals for bulimia nervosa have been found to be effective when used in the British health care system; in that system, although health care is free at the source to all, it is recognized that rationing of care is necessary (
9,
10,
12). Fairburn (
32) has suggested that self-care or guided self-care may be a useful first phase in treatment, but such a form of treatment may not be effective in other cultures with different expectations about provision of health care. It is interesting that the present study found that guided self-care can be generalized to the German health care system, which has excellent provision of long-term psychotherapy.
The patients in this study appeared to be similar to those reported in other treatment studies; their ages and duration of illness were similar to those in a study by Agras et al. (
5), but they were older (28 years versus 24 years) and more chronically ill (8 years versus 6 years) than the groups reported by Fairburn et al. (
4) and Garner et al. (
33). An interesting finding which suggests that there may be cultural differences in the clinical presentation of bulimia nervosa is that very few patients abused laxatives. This is in contrast to patients in the United Kingdom, where laxative abuse occurred in 28% (
4), and in the United States, where it occurred in 10% (
7).
Despite German skepticism about pragmatic minimal interventions, there was no significant difference between groups in dropout rate, although there was a tendency for the dropout rate to be higher in the guided self-change group (29.0%, N=9) than in the cognitive behavior therapy group (12.9%, N=4). This dropout rate lies within the range of 0%–34% reported in a review of treatments of bulimia nervosa (
34). One of our study's shortcomings is that we did not measure expectations of improvement. In any case, one might have expected rather more reserve regarding guided self-change and therefore less success with this treatment modality. Thus, the good outcome in the experimental group is even more impressive.
While the more conservative F test showed all time-by-treatment interactions to be nonsignificant at the 0.05 level, approximate tests showed that there were significant interactions for Beck depression scores and Eating Disorders Awareness Test scores. These suggest that levels of depression fell earlier in treatment among subjects in the cognitive behavior therapy group, while knowledge increased earlier in treatment in the guided self-change group. However, by the time of follow-up, the two groups had similar levels of depression and knowledge, suggesting that while a particular treatment may have a faster or slower effect on depression and knowledge, the treatments are equally effective in the longer term. On the other hand, perhaps too much should not be made of these results, since they are only approximate, and the more conservative tests had yielded nonsignificant results. Although the differences between the groups in the timing of responses on these two variables are interesting, it may be unwise to reject the null hypothesis too confidently.
An intriguing question raised by our study is how the guided self-change patients managed to “catch up” during follow-up. We are confident that this was not simply the result of this group's additional therapy. One possibility is that the posttreatment improvement of this group resulted from their being able to make further gains by continuing to work with the self-care manual once their therapist-aided sessions had ended.
One criticism of our study is that with the design we used, we could not rule out the possibility that improvement was due to nonspecific treatment effects, although this would not account for differences in rates of change/abstinence. In a future study it might be interesting to compare directly eight sessions of cognitive behavior therapy plus use of the manual with the same amount of nonspecific support plus use of the manual, in order to tease out nonspecific effects of contact with a therapist and participation in a study in a therapeutic setting. An open study by Cooper et al. (
12) addressed this issue to some extent.
One of the limitations of this study was that we only succeeded in obtaining a follow-up rate of 77%. Any conclusions from this study therefore have to take this into account. Many centers find similar difficulties in obtaining follow-up information from their patients, and there has to be a balance between high completion rates and intrusiveness. Another limitation of this study is that although it raised questions of the cost-effectiveness of treatment, it did not address economic issues. Further studies with larger groups that could examine the course of treatment in more detail by using sophisticated health economics methods would be of great interest. Larger, phase-3-type studies where factors such as treatment dose and matching patient characteristics to type of therapy are examined may be an important next step in research into the management of bulimia nervosa.