Predictors of Antidepressant Recommendation
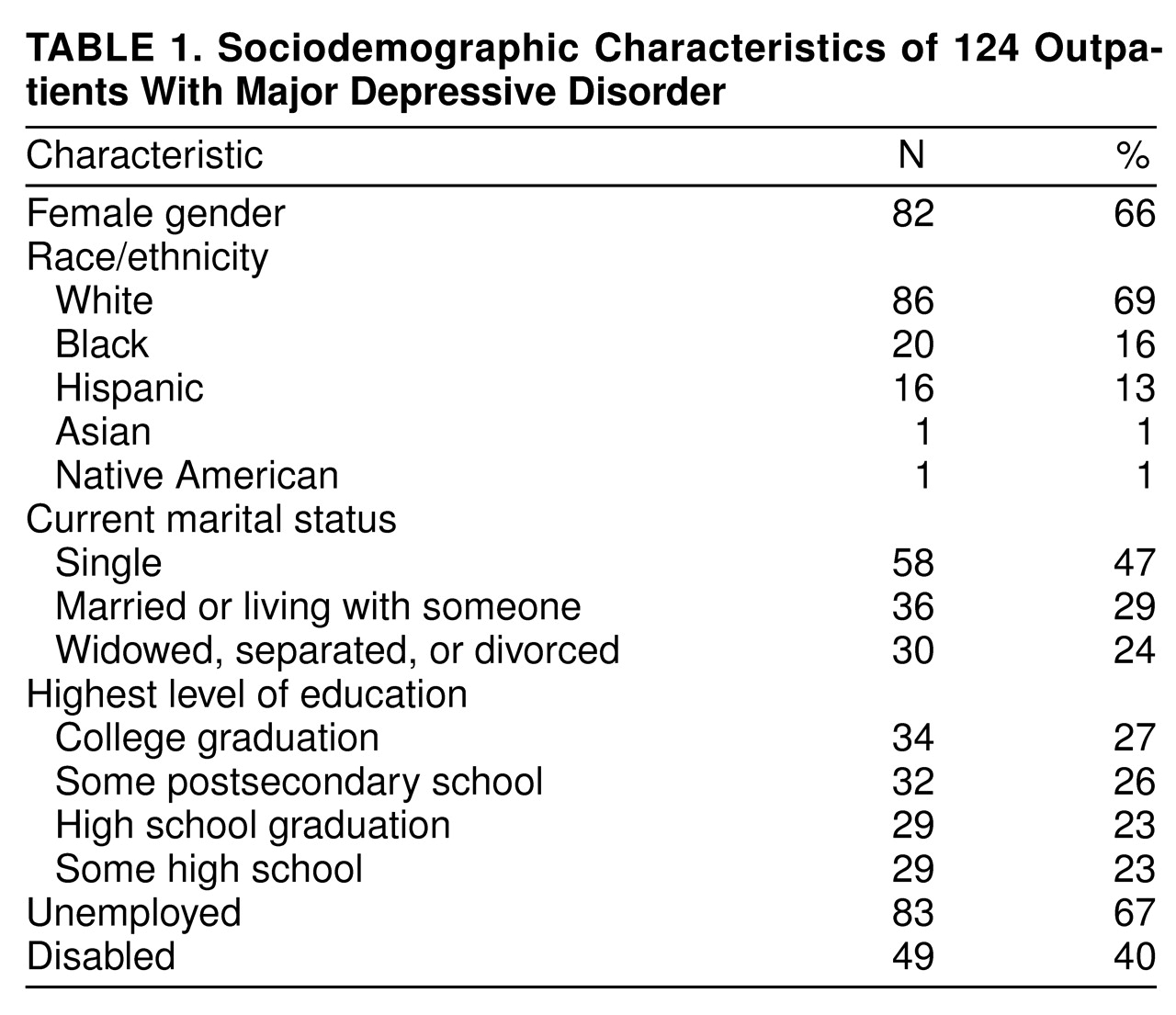
Analyses of bivariate associations between patient sociodemographic characteristics and medication recommendation revealed that only ethnicity/race was associated with antidepressant recommendation: a larger proportion of nonminority patients (84%, N=72) than minority patients (45%, N=17) received recommendations for antidepressants (χ2=17.89, df=1, p<0.001). The number of minority patients (N=38) was too small for stratified analyses. Post hoc comparisons of the black, Hispanic, and white patients indicated that a larger proportion of white patients (84%, N=72) received a recommendation for antidepressant drugs than either the black patients (30%, N=6) (χ2=18.16, df=1, p<0.001) or Hispanic patients (56%, N=9) (χ2=4.67, df=1, p=0.03). There was no difference in recommendations for medication between the two minority groups (χ2=1.56, df=1, p=0.21). Recommendation for antidepressant medication was not associated with differences in gender, age, education, employment status, disability status, income, marital status, living arrangements, or method of payment (Medicaid, fee for service, managed care, or other insurance).
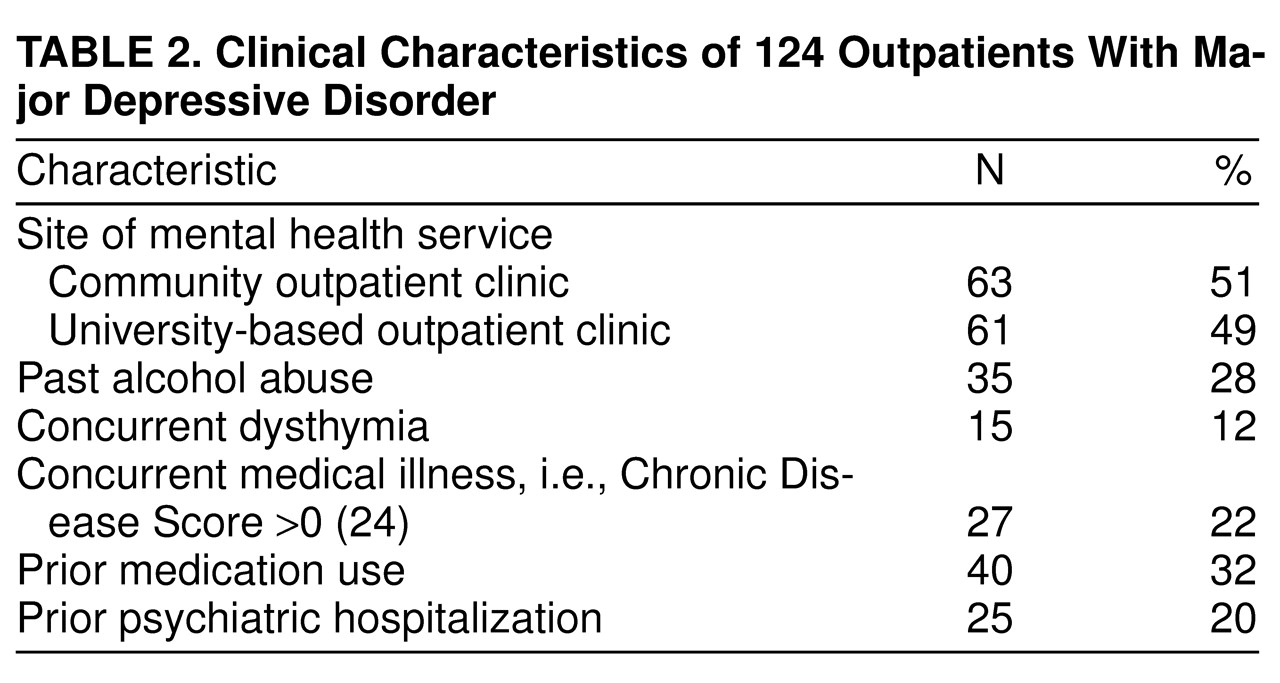
The two types of clinics, university based and community, differed in the association between ethnic/racial status and recommendation for antidepressant drugs. At the community sites, medication was significantly less likely to be recommended to minority patients; 74% of the nonminority patients (25 of 34) and only 38% of the minority patients (11 of 29) received recommendations for medication (χ2=6.71, df=1, p=0.01). At the university-based clinic, the difference was not significant: medication was recommended for 90% of the nonminority patients (47 of 52) and 67% of the minority patients (six of nine) (χ2=1.99, df=1, p=0.16). According to the data elicited by the SCID-P, there were no differences between minority and nonminority patients in the presence of specific depressive phenomena (such as melancholic or atypical symptoms), suicidality, age at onset, or duration of current episode. Exploratory comparisons of the minority and nonminority patients’ symptoms as shown by the Hamilton depression scale indicated that the minority patients reported greater weight loss (t=2.15, df=123, p=0.03) and the white patients reported greater disruption of work and/or activities. According to the SCID-P, there were no differences in clinical presentation (e.g., specific major depression criteria endorsed, presence of melancholic or atypical symptoms, suicidal ideation, age at onset, or duration of current episode). There were no other sociodemographic variables (e.g., gender, age, employment, self-reported disability, or marital status) that differed between the patients who did and did not receive recommendations for antidepressant medication.
The patients who received a recommendation for antidepressant treatment had higher overall scores on the Hamilton depression scale (mean=9.7, SD=5.0) than the patients who did not receive a recommendation for medication (mean=18.0, SD=3.6) (t=2.00, df=123, p=0.02). Medication recommendation was more likely among patients with a prior psychiatric hospitalization (88%, N=22) than among individuals who had never been hospitalized (67%, N=67) (χ2=3.13, df=1, p=0.08). Medication recommendation was not associated with differences in the subtype of depression (atypical, melancholic), suicidal ideation, duration of current illness, prior episodes of depression, or presence of a medical illness. Using the cutoff score of 1.1 on the Inventory of Interpersonal Problems, the screen for personality disorders, we found that patients with and without significant personality pathology were equally likely to receive recommendations for medication. Recent antidepressant treatment was a significant predictor of medication recommendation; 98% of the patients (39 of 40) with a recent history of prior antidepressant use (at least 1 week of use during the 3 months before intake) received a recommendation for antidepressant medication, compared to 60% of the patients without recent antidepressant use (50 of 84) (χ2=17.46, df=1, p<0.001).
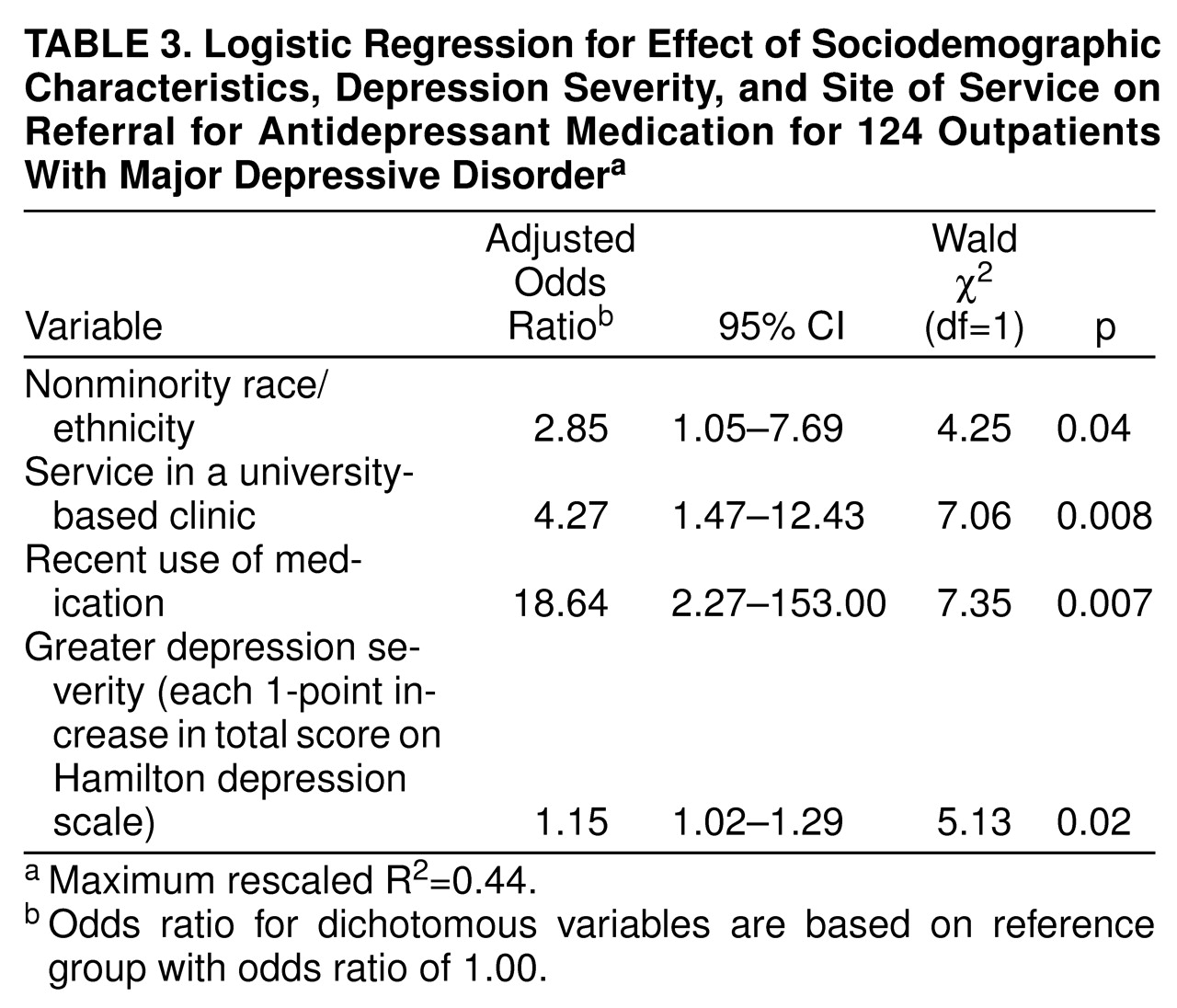
Logistic regression was used to determine the independent effects of historical, sociodemographic, clinical, and site factors significant in bivariate comparisons at the p<0.10 level (
table 3). White patients were almost three times as likely to receive a recommendation for antidepressants than minority patients, even after we controlled for severity of depression, site, and recent use of medication. Site of service remained a significant predictor of medication recommendation, such that patients with major depressive disorder who sought help at the university-based clinic were more than four times as likely to receive a medication recommendation than patients seen at other outpatient mental health clinics. To explore the differential treatment of minority patients by site, an interaction term (clinic type by ethnicity) was entered into the model. The term did not significantly contribute to the model. With depression severity controlled, the patients with recent antidepressant use were 18 times as likely to receive a medication recommendation than individuals without recent antidepressant use. When the Hamilton score was used as a continuous variable, overall depression severity continued to predict the likelihood of medication recommendation, such that each additional point on the scale was associated with a 1.15 odds of having medication recommended. Prior hospitalization did not contribute to the model. The four variables in the model accounted for 44% of the total variance.
The model created by the logistic regression analyses correctly predicted group membership (medication recommended or not recommended) for 82% of the patients, 92% of those who actually received medication recommendations (81 of 88) and 60% of those who did not receive medication recommendations (21 of 36).
To identify the depressive symptom profile of individuals who received a medication recommendation, we compared scores on the individual items of the Hamilton depression scale for these patients with scores for the patients who were not referred for medication. The patients referred for medication had significantly higher scores on the item for depressed mood than did the patients not referred for antidepressant treatment (t=3.84, df=123, p<0.001). This was the only symptom significant at the p=0.002 level or better; none of the other items approached significance. To examine whether depressed mood contributed more to the overall model than did the total Hamilton depression scale score, a separate logistic regression was conducted. Depressed mood was a more significant clinical predictor of medication recommendation than overall severity (odds ratio=3.80, χ2=6.78, df=1, p=0.009).